“Ventricular Fibrillation: Life-Threatening Arrhythmia
Related Articles Ventricular Fibrillation: Life-Threatening Arrhythmia
- Understanding Coronary Artery Disease: Causes And Risk Factors
- Telemedicine And Remote Monitoring For Chronic Illness Care – Part 2
- Exercise And Physical Activity Guidelines For Chronic Illness Management – Part 7
- Palliative Care And Quality Of Life For Chronic Illness Patients – Part 7
- Psychological Resilience In Chronic Disease Patients: Navigating Challenges And Fostering Well-being
Introduction
We will be happy to explore interesting topics related to Ventricular Fibrillation: Life-Threatening Arrhythmia. Let’s knit interesting information and provide new insights to readers.
Table of Content
Ventricular Fibrillation: Life-Threatening Arrhythmia
Ventricular fibrillation (VF) is a life-threatening cardiac arrhythmia characterized by rapid, disorganized electrical activity in the ventricles of the heart. This chaotic electrical activity causes the ventricles to quiver instead of contracting effectively, leading to a complete cessation of effective blood flow and cardiac output. VF is a medical emergency that requires immediate intervention to prevent sudden cardiac death.
Understanding the Heart’s Electrical System
To comprehend ventricular fibrillation, it’s essential to grasp the fundamentals of the heart’s electrical system. The heart’s rhythmic contractions are orchestrated by a complex electrical conduction system. The sinoatrial (SA) node, often referred to as the heart’s natural pacemaker, initiates the electrical impulse. This impulse travels through the atria, causing them to contract and pump blood into the ventricles.
The electrical signal then reaches the atrioventricular (AV) node, which briefly delays the impulse, allowing the ventricles to fill completely. Subsequently, the impulse travels down the bundle of His and into the Purkinje fibers, which spread the electrical signal throughout the ventricles, causing them to contract and pump blood out to the body.
What is Ventricular Fibrillation?
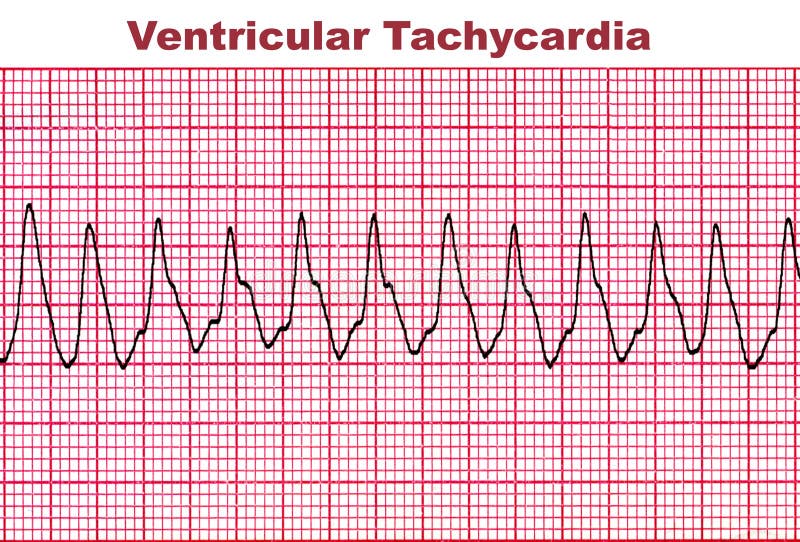
Ventricular fibrillation occurs when the normal electrical impulses in the ventricles become chaotic and disorganized. Instead of a coordinated contraction, the ventricles quiver rapidly and irregularly. This quivering prevents the heart from effectively pumping blood to the brain, lungs, and other vital organs.
Without prompt treatment, ventricular fibrillation can lead to loss of consciousness, seizures, and sudden cardiac death within minutes.
Causes and Risk Factors of Ventricular Fibrillation
Ventricular fibrillation can be triggered by various underlying heart conditions and external factors. Some of the common causes and risk factors include:
-
Coronary Artery Disease (CAD): CAD is the most prevalent underlying cause of VF. When the coronary arteries become narrowed or blocked by plaque buildup, it can lead to ischemia (reduced blood flow) to the heart muscle. Ischemia can disrupt the heart’s electrical stability and trigger VF.
-
Heart Attack (Myocardial Infarction): A heart attack occurs when blood flow to a portion of the heart muscle is completely blocked, leading to tissue damage. The damaged heart tissue can disrupt the heart’s electrical system and increase the risk of VF.
-
Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle. These conditions can alter the heart’s structure and electrical properties, making it more susceptible to VF.
-
Heart Failure: Heart failure is a condition in which the heart is unable to pump enough blood to meet the body’s needs. Heart failure can lead to electrical instability and increase the risk of VF.
-
Electrolyte Imbalances: Imbalances in electrolytes such as potassium, magnesium, and calcium can disrupt the heart’s electrical activity and trigger VF.
-
Certain Medications: Some medications, such as antiarrhythmics, can paradoxically increase the risk of VF in certain individuals.
-
Genetic Predisposition: Certain genetic mutations can predispose individuals to VF. These mutations can affect the heart’s electrical channels and increase the risk of arrhythmias.
-
Structural Heart Abnormalities: Congenital or acquired structural heart abnormalities can disrupt the heart’s electrical system and increase the risk of VF.
-
Electrical Shock or Trauma: Electrical shock or trauma to the chest can disrupt the heart’s electrical activity and trigger VF.
-
Substance Abuse: The use of illicit drugs, such as cocaine and methamphetamine, can increase the risk of VF.
Symptoms of Ventricular Fibrillation
Ventricular fibrillation is a medical emergency, and symptoms typically occur suddenly and without warning. The most common symptoms include:
- Sudden collapse or loss of consciousness
- Absence of pulse
- Absence of breathing
- Seizures
Diagnosis of Ventricular Fibrillation
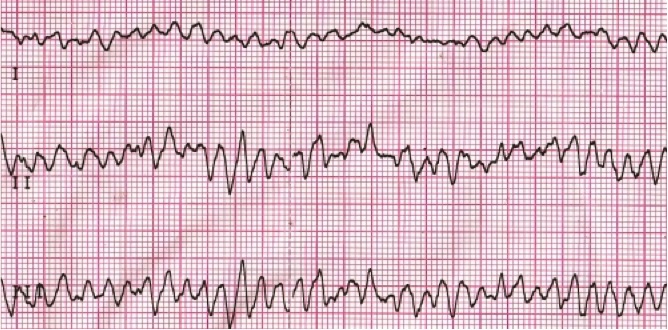
Ventricular fibrillation is diagnosed using an electrocardiogram (ECG). An ECG is a non-invasive test that records the heart’s electrical activity. In VF, the ECG will show a chaotic, irregular pattern with no discernible P waves, QRS complexes, or T waves.
Treatment of Ventricular Fibrillation
Ventricular fibrillation requires immediate treatment to restore a normal heart rhythm and prevent sudden cardiac death. The primary treatment for VF is defibrillation.
-
Defibrillation: Defibrillation involves delivering a controlled electrical shock to the heart to depolarize the heart muscle and allow the heart’s natural pacemaker (SA node) to regain control. Defibrillation is most effective when administered within minutes of the onset of VF.
-
Cardiopulmonary Resuscitation (CPR): CPR is an essential life-saving technique that provides artificial circulation and breathing until defibrillation can be performed. CPR involves chest compressions and rescue breaths.
-
Medications: Medications such as epinephrine and amiodarone may be administered during CPR to help restore a normal heart rhythm.
-
Implantable Cardioverter-Defibrillator (ICD): An ICD is a small device implanted in the chest that continuously monitors the heart’s rhythm. If the ICD detects VF, it will deliver an electrical shock to restore a normal heart rhythm.
Prevention of Ventricular Fibrillation
Preventing ventricular fibrillation involves addressing the underlying risk factors and heart conditions that can lead to VF. Some preventive measures include:
-
Managing Coronary Artery Disease: Lifestyle modifications such as a healthy diet, regular exercise, and smoking cessation can help manage CAD and reduce the risk of VF.
-
Controlling Blood Pressure and Cholesterol: High blood pressure and high cholesterol can contribute to CAD. Managing these conditions through medication and lifestyle changes can reduce the risk of VF.
-
Treating Heart Failure: Medications and lifestyle changes can help manage heart failure and reduce the risk of VF.
-
Avoiding Substance Abuse: Substance abuse can increase the risk of VF. Avoiding illicit drugs can help prevent VF.
-
Regular Medical Checkups: Regular medical checkups can help identify and manage underlying heart conditions that can increase the risk of VF.
-
Knowing CPR: Learning CPR can help save lives in the event of VF.
Conclusion
Ventricular fibrillation is a life-threatening arrhythmia that requires immediate intervention. Understanding the causes, symptoms, diagnosis, treatment, and prevention of VF is crucial for healthcare professionals and the general public. Prompt recognition and treatment of VF can significantly improve the chances of survival and prevent sudden cardiac death.







Leave a Reply