“Understanding Heart Block: A Comprehensive Guide to Types, Causes, Symptoms, and Management
Related Articles Understanding Heart Block: A Comprehensive Guide to Types, Causes, Symptoms, and Management
- Public Health Initiatives To Combat Chronic Illnesses – Part 9: Leveraging Technology And Data Analytics For Personalized Interventions
- The Role Of Artificial Intelligence In Leukemia Diagnosis
- Patient Empowerment In Chronic Disease Management – Part 10: Leveraging Technology For Enhanced Self-Care And Remote Monitoring
- Role Of Community Support In Heart Disease Prevention
- Alternative Therapies For Chronic Pain Management – Part 9
Introduction
On this special occasion, we are happy to review interesting topics related to Understanding Heart Block: A Comprehensive Guide to Types, Causes, Symptoms, and Management. Let’s knit interesting information and provide new insights to readers.
Table of Content
Understanding Heart Block: A Comprehensive Guide to Types, Causes, Symptoms, and Management
Heart block, also known as atrioventricular (AV) block, is a condition in which the electrical signals that control the heart’s rhythm are partially or completely blocked from traveling from the atria (upper chambers) to the ventricles (lower chambers). This disruption can lead to a slower and irregular heartbeat, potentially affecting the heart’s ability to pump blood effectively throughout the body. Understanding heart block is crucial for early detection, appropriate management, and improving patient outcomes.
The Heart’s Electrical System: A Brief Overview
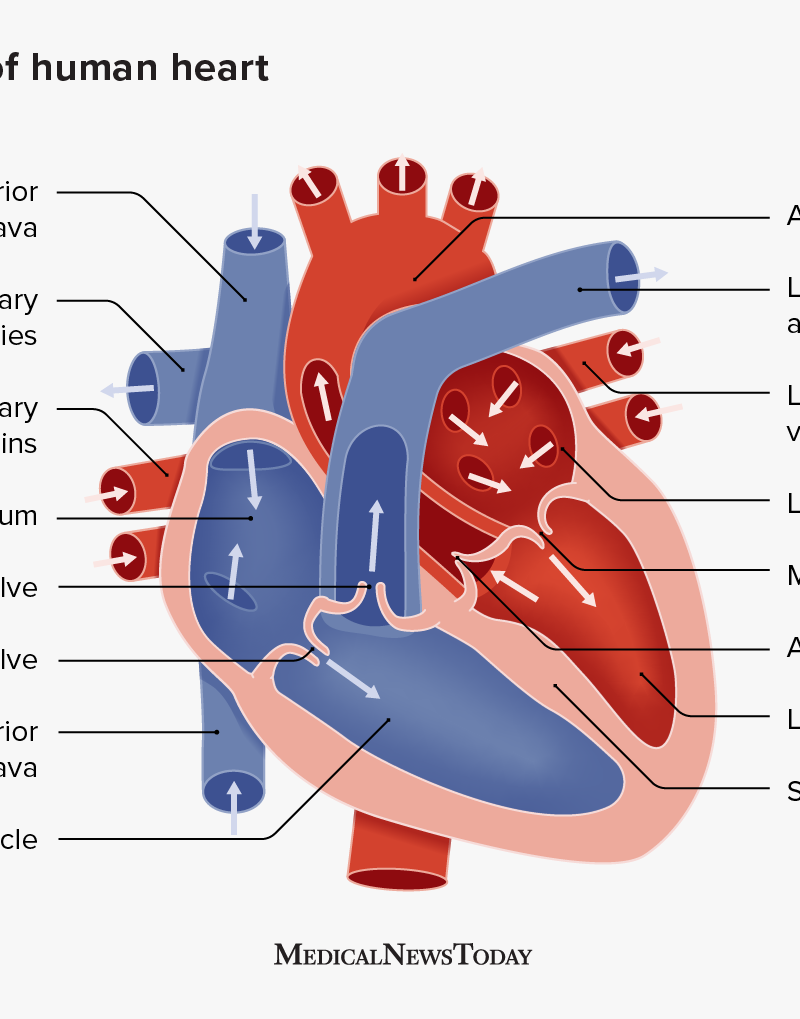
To fully grasp the concept of heart block, it is essential to understand the heart’s electrical system. The heart’s natural pacemaker, the sinoatrial (SA) node, located in the right atrium, generates electrical impulses that initiate each heartbeat. These impulses travel through the atria, causing them to contract and pump blood into the ventricles.
The electrical signal then reaches the AV node, which acts as a gatekeeper, briefly delaying the signal to allow the atria to fully contract before the ventricles are stimulated. From the AV node, the electrical impulse travels down the bundle of His, which divides into the left and right bundle branches, and then spreads throughout the ventricles via the Purkinje fibers. This coordinated electrical activity causes the ventricles to contract, pumping blood out to the lungs and the rest of the body.
What is Heart Block?
Heart block occurs when there is a disruption in the electrical pathway between the atria and the ventricles. This disruption can be partial or complete, leading to varying degrees of severity. The block can occur at the AV node itself or in the bundle branches below the AV node.
Types of Heart Block
Heart block is classified into different degrees, based on the severity of the block:
-
First-Degree Heart Block: This is the mildest form of heart block. In first-degree heart block, the electrical impulses from the atria to the ventricles are slowed down, but they still reach the ventricles. On an electrocardiogram (ECG), this is characterized by a prolonged PR interval (the time it takes for the electrical impulse to travel from the atria to the ventricles). First-degree heart block usually does not cause any symptoms and often does not require treatment.
-
Second-Degree Heart Block: In second-degree heart block, some electrical impulses from the atria fail to reach the ventricles. This can manifest in two different forms:
- Mobitz Type I (Wenckebach): In this type, the PR interval progressively lengthens with each heartbeat until a beat is dropped altogether. This pattern repeats itself. Mobitz Type I is usually caused by a block within the AV node and is often temporary and benign.
- Mobitz Type II: In this type, the PR interval remains constant, but some beats are suddenly blocked, resulting in a skipped ventricular contraction. Mobitz Type II is more serious than Mobitz Type I, as it is often associated with a block below the AV node (in the bundle branches) and can progress to complete heart block.
-
Third-Degree Heart Block (Complete Heart Block): This is the most severe form of heart block. In third-degree heart block, there is a complete block of electrical impulses between the atria and the ventricles. The atria and ventricles beat independently of each other. The ventricles generate their own electrical impulses, but at a much slower rate than normal. This can lead to a very slow heart rate (bradycardia) and can be life-threatening.
Causes of Heart Block
Heart block can be caused by a variety of factors, including:
- Congenital Heart Defects: Some individuals are born with heart defects that can disrupt the heart’s electrical system.
- Coronary Artery Disease (CAD): CAD can reduce blood flow to the heart muscle, including the AV node and the bundle branches, leading to heart block.
- Myocardial Infarction (Heart Attack): A heart attack can damage the heart muscle and the electrical pathways, resulting in heart block.
- Medications: Certain medications, such as beta-blockers, calcium channel blockers, digoxin, and antiarrhythmic drugs, can slow down the heart’s electrical activity and cause heart block.
- Electrolyte Imbalances: Imbalances in electrolytes, such as potassium, calcium, and magnesium, can affect the heart’s electrical function and lead to heart block.
- Inflammatory Conditions: Conditions such as myocarditis (inflammation of the heart muscle) and rheumatic fever can damage the heart’s electrical system.
- Age-Related Degeneration: As people age, the heart’s electrical system can degenerate, increasing the risk of heart block.
- Cardiac Surgery: Heart block can sometimes occur as a complication of cardiac surgery.
- Lyme Disease: In rare cases, Lyme disease can cause heart block.
- Hyperkalemia: Elevated potassium levels can cause heart block.
- Hypothermia: Low body temperature can also lead to heart block.
Symptoms of Heart Block
The symptoms of heart block can vary depending on the severity of the block and the individual’s overall health. Some people with mild heart block may not experience any symptoms, while others with more severe heart block may experience:
- Dizziness or Lightheadedness: A slow heart rate can reduce blood flow to the brain, leading to dizziness or lightheadedness.
- Fainting (Syncope): In severe cases, a very slow heart rate can cause fainting.
- Fatigue: A slow heart rate can reduce the amount of oxygen delivered to the body’s tissues, leading to fatigue.
- Shortness of Breath: A slow heart rate can make it difficult for the heart to pump enough blood to meet the body’s needs, leading to shortness of breath.
- Chest Pain: In some cases, heart block can cause chest pain, especially if it is associated with coronary artery disease.
- Palpitations: Some people with heart block may feel palpitations, or a sensation of a skipped or irregular heartbeat.
- Confusion: Reduced blood flow to the brain can cause confusion.
- Cardiac Arrest: In rare cases, complete heart block can lead to cardiac arrest.
Diagnosis of Heart Block
Heart block is typically diagnosed using an electrocardiogram (ECG). An ECG records the electrical activity of the heart and can reveal abnormalities in the heart’s rhythm and conduction. The ECG can help determine the type and severity of heart block.
In addition to an ECG, other tests may be performed to evaluate the heart’s function and identify the underlying cause of heart block. These tests may include:
- Holter Monitor: A Holter monitor is a portable ECG that records the heart’s electrical activity over a 24- to 48-hour period. This can help detect intermittent heart block or other arrhythmias that may not be apparent on a standard ECG.
- Event Recorder: An event recorder is a device that can be worn for several weeks or months. It records the heart’s electrical activity when the patient experiences symptoms.
- Echocardiogram: An echocardiogram is an ultrasound of the heart that can assess the heart’s structure and function.
- Stress Test: A stress test involves monitoring the heart’s electrical activity while the patient exercises. This can help identify heart block that is triggered by exertion.
- Electrophysiology Study (EPS): An EPS is an invasive procedure that involves inserting catheters into the heart to map the heart’s electrical activity. This can help pinpoint the location of the block and determine the best course of treatment.
- Blood Tests: Blood tests may be performed to check for electrolyte imbalances, thyroid disorders, or other conditions that can contribute to heart block.
Management of Heart Block
The treatment for heart block depends on the type and severity of the block, as well as the patient’s symptoms and overall health.
- First-Degree Heart Block: First-degree heart block usually does not require treatment. However, the underlying cause of the block should be addressed, if possible.
- Second-Degree Heart Block Mobitz Type I: Second-degree heart block Mobitz Type I often does not require treatment, especially if the patient is asymptomatic. However, if the patient is symptomatic, or if the block is caused by a reversible factor such as medication, treatment may be necessary.
- Second-Degree Heart Block Mobitz Type II and Third-Degree Heart Block: Second-degree heart block Mobitz Type II and third-degree heart block typically require treatment with a pacemaker. A pacemaker is a small, battery-powered device that is implanted under the skin and connected to the heart via wires. The pacemaker monitors the heart’s electrical activity and delivers electrical impulses to the heart when the heart rate is too slow.
Other Management Strategies
In addition to pacemakers, other management strategies for heart block may include:
- Medication Adjustment: If heart block is caused by a medication, the medication may need to be adjusted or discontinued.
- Treatment of Underlying Conditions: If heart block is caused by an underlying condition such as coronary artery disease or electrolyte imbalance, the underlying condition should be treated.
- Lifestyle Modifications: Lifestyle modifications such as avoiding smoking, maintaining a healthy weight, and eating a healthy diet can help improve overall heart health and reduce the risk of heart block.
Living with a Pacemaker
Living with a pacemaker requires some adjustments, but most people with pacemakers are able to live normal, active lives.
- Regular Checkups: People with pacemakers need to have regular checkups with their doctor to ensure that the pacemaker is functioning properly.
- Avoidance of Strong Magnetic Fields: People with pacemakers should avoid close contact with strong magnetic fields, such as those produced by MRI machines.
- Monitoring for Symptoms: People with pacemakers should be aware of the symptoms of pacemaker malfunction, such as dizziness, fainting, or palpitations.
- Medication Adherence: People with pacemakers should take their medications as prescribed.
Conclusion
Heart block is a condition in which the electrical signals that control the heart’s rhythm are disrupted. It can range from mild to severe and can be caused by a variety of factors. Early diagnosis and appropriate management are crucial for improving patient outcomes. With proper treatment, most people with heart block can live normal, active lives. Understanding the types, causes, symptoms, and management of heart block is essential for both healthcare professionals and individuals at risk. If you suspect you may have heart block, it’s crucial to consult with a healthcare professional for accurate diagnosis and personalized treatment.








Leave a Reply