“The Role of Stress in Chronic Disease Progression – Part 10: Therapeutic Interventions Targeting the Stress Response to Mitigate Disease
Related Articles The Role of Stress in Chronic Disease Progression – Part 10: Therapeutic Interventions Targeting the Stress Response to Mitigate Disease
- The Impact Of Chronic Illness On Mental Health – Part 9
- Patient Empowerment In Chronic Disease Management – Part 2: Strategies, Technologies, And Future Directions
- Yoga And Mindfulness Practices For Chronic Disease Patients – Part 9
- Social Support Networks For Chronic Disease Patients – Part 5: Leveraging Technology And Expanding Horizons
- Challenges In Diagnosing Rare Chronic Illnesses – Part 5
Introduction
We will be happy to explore interesting topics related to The Role of Stress in Chronic Disease Progression – Part 10: Therapeutic Interventions Targeting the Stress Response to Mitigate Disease. Let’s knit interesting information and provide new insights to readers.
Table of Content
The Role of Stress in Chronic Disease Progression – Part 10: Therapeutic Interventions Targeting the Stress Response to Mitigate Disease

Chronic diseases, ranging from cardiovascular disorders and diabetes to autoimmune conditions and neurodegenerative illnesses, represent a significant global health burden. While genetic predisposition and environmental factors play crucial roles in their development and progression, the influence of chronic stress cannot be overstated. As explored throughout this series, sustained activation of the stress response system – involving the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system (SNS) – contributes to systemic inflammation, immune dysregulation, metabolic dysfunction, and cellular damage, all of which accelerate the pathogenesis of chronic diseases.
Given the profound impact of stress on chronic disease, therapeutic interventions aimed at modulating the stress response represent a promising avenue for mitigating disease progression, improving patient outcomes, and enhancing overall quality of life. This article, Part 10 of our series, delves into various therapeutic strategies that target the stress response, examining their mechanisms of action, clinical evidence supporting their efficacy, and potential limitations.
I. Lifestyle Modifications: The Foundation of Stress Management
Lifestyle modifications form the cornerstone of stress management and represent the first line of defense against the detrimental effects of chronic stress. These interventions are generally accessible, cost-effective, and carry minimal risk of adverse effects when implemented appropriately.
-
Regular Physical Activity: Exercise is a potent stress reliever, acting through multiple pathways. It reduces levels of stress hormones like cortisol and adrenaline, while simultaneously increasing the production of endorphins, natural mood elevators. Regular physical activity also improves sleep quality, enhances cardiovascular health, and promotes weight management, all of which contribute to reduced stress levels and improved overall well-being. Studies have shown that exercise can significantly reduce symptoms of anxiety and depression, common comorbidities associated with chronic diseases. The type and intensity of exercise should be tailored to individual capabilities and preferences, ranging from brisk walking and swimming to yoga and strength training.
-
Healthy Diet and Nutrition: A balanced diet rich in fruits, vegetables, whole grains, and lean protein provides essential nutrients that support optimal physiological function and enhance resilience to stress. Conversely, diets high in processed foods, sugar, and unhealthy fats can exacerbate inflammation and impair stress response regulation. Specific nutrients, such as omega-3 fatty acids, magnesium, and B vitamins, play critical roles in brain health and stress management. Mindful eating practices, which involve paying attention to hunger cues and savoring each bite, can also promote relaxation and reduce stress-related overeating.
-
Adequate Sleep Hygiene: Sleep deprivation is a major stressor that disrupts HPA axis function, impairs immune function, and increases susceptibility to chronic diseases. Establishing a regular sleep schedule, creating a relaxing bedtime routine, optimizing the sleep environment (e.g., dark, quiet, cool), and avoiding caffeine and alcohol before bed can significantly improve sleep quality and reduce stress levels. Cognitive behavioral therapy for insomnia (CBT-I) is an effective non-pharmacological treatment for chronic insomnia that addresses the underlying behavioral and cognitive factors contributing to sleep problems.
-
Mindfulness and Meditation Practices: Mindfulness-based interventions, such as mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), cultivate present moment awareness and acceptance, allowing individuals to observe their thoughts and feelings without judgment. These practices have been shown to reduce activity in the amygdala, the brain region associated with fear and anxiety, and increase activity in the prefrontal cortex, which is involved in emotional regulation. Regular mindfulness practice can lower cortisol levels, improve immune function, and reduce symptoms of anxiety, depression, and chronic pain.
II. Psychological Therapies: Addressing the Cognitive and Emotional Components of Stress
Psychological therapies target the cognitive and emotional aspects of stress, helping individuals develop coping mechanisms, reframe negative thought patterns, and manage their emotional responses to stressors.
-
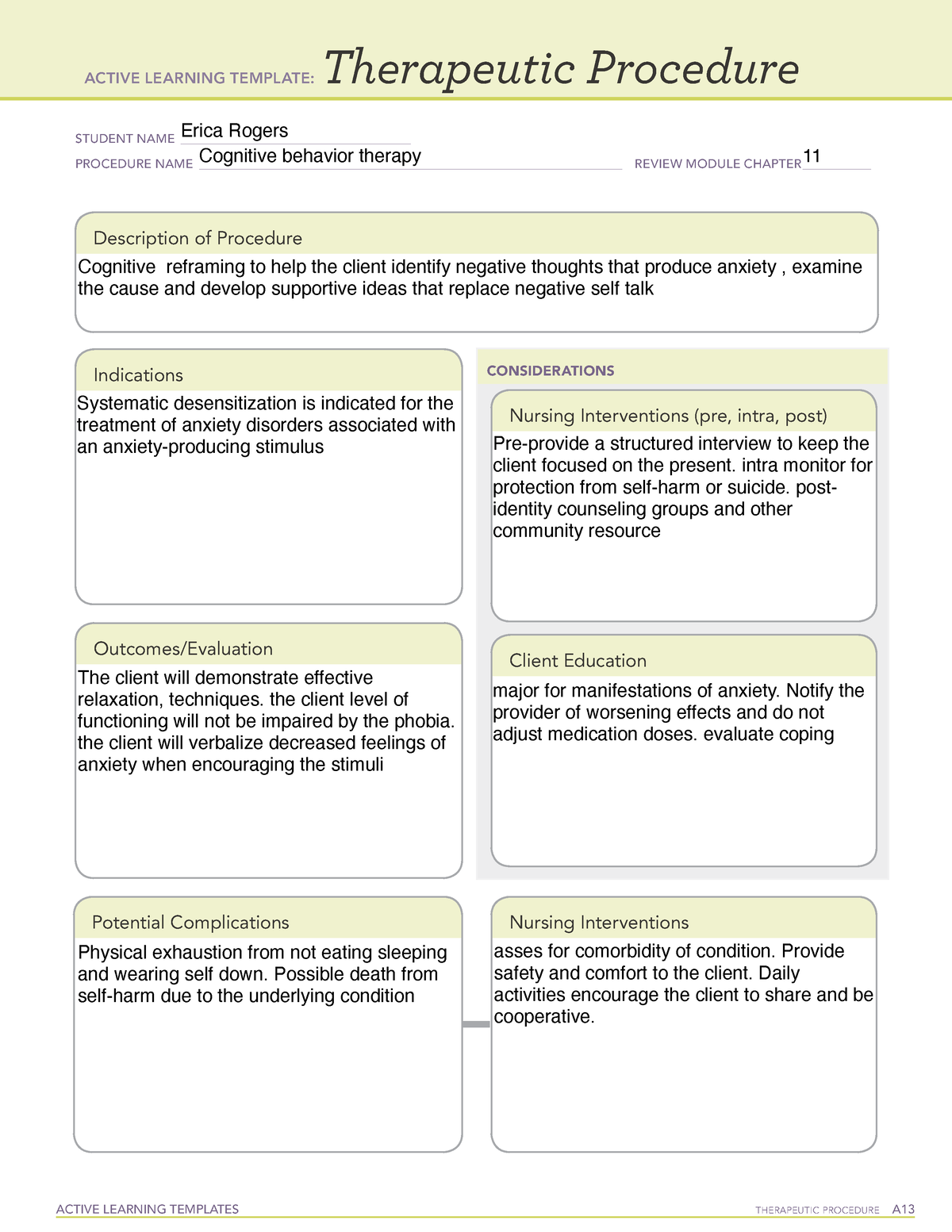
Cognitive Behavioral Therapy (CBT): CBT is a widely used and evidence-based therapy that focuses on identifying and modifying maladaptive thoughts, feelings, and behaviors that contribute to stress and emotional distress. CBT techniques, such as cognitive restructuring, behavioral activation, and exposure therapy, help individuals challenge negative beliefs, develop problem-solving skills, and manage anxiety-provoking situations. CBT has been shown to be effective in treating a wide range of stress-related conditions, including anxiety disorders, depression, and chronic pain.
-
Stress Management Training (SMT): SMT encompasses a variety of techniques designed to enhance individuals’ ability to cope with stress. These techniques may include relaxation training (e.g., progressive muscle relaxation, deep breathing exercises), time management skills, assertiveness training, and social support enhancement. SMT programs often involve a combination of education, skills training, and practice sessions, empowering individuals to proactively manage stress and improve their overall well-being.
-
Biofeedback: Biofeedback is a technique that allows individuals to gain awareness of their physiological responses to stress, such as heart rate, muscle tension, and skin conductance. By using real-time feedback from sensors, individuals can learn to consciously control these physiological responses through relaxation techniques and mental imagery. Biofeedback has been shown to be effective in reducing stress, anxiety, and chronic pain, and may be particularly helpful for individuals who struggle with identifying and managing their physiological responses to stress.
III. Pharmacological Interventions: Targeting Neurotransmitter Systems and Hormonal Imbalances
Pharmacological interventions may be considered when lifestyle modifications and psychological therapies are insufficient to manage stress effectively, particularly in individuals with severe anxiety, depression, or other stress-related disorders.
-
Selective Serotonin Reuptake Inhibitors (SSRIs): SSRIs are commonly prescribed antidepressants that increase serotonin levels in the brain, which can improve mood, reduce anxiety, and enhance stress resilience. SSRIs are generally well-tolerated, but potential side effects may include nausea, insomnia, and sexual dysfunction.
-
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): SNRIs increase both serotonin and norepinephrine levels in the brain, offering a broader range of effects than SSRIs. SNRIs may be particularly helpful for individuals with chronic pain or fatigue in addition to anxiety or depression.
-
Benzodiazepines: Benzodiazepines are a class of anti-anxiety medications that enhance the effects of GABA, a neurotransmitter that inhibits brain activity. Benzodiazepines can provide rapid relief from anxiety symptoms, but they are associated with a risk of dependence and withdrawal symptoms, and should be used with caution.
-
Beta-Blockers: Beta-blockers are medications that block the effects of adrenaline, reducing heart rate, blood pressure, and other physical symptoms of anxiety. Beta-blockers may be helpful for managing performance anxiety or social anxiety.
-
Hormone Replacement Therapy (HRT): In certain cases, hormonal imbalances may contribute to stress and mood disturbances. For example, women experiencing menopause may benefit from hormone replacement therapy to alleviate symptoms such as hot flashes, sleep disturbances, and mood swings.
IV. Complementary and Alternative Medicine (CAM): Integrating Holistic Approaches
Complementary and alternative medicine (CAM) modalities offer a holistic approach to stress management, addressing the mind-body connection and promoting relaxation, balance, and well-being.
-
Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body to stimulate energy flow and promote healing. Acupuncture has been shown to reduce stress, anxiety, and pain, and may be particularly helpful for individuals who prefer a non-pharmacological approach to stress management.
-
Yoga: Yoga combines physical postures, breathing techniques, and meditation to promote relaxation, flexibility, and strength. Yoga has been shown to reduce cortisol levels, improve sleep quality, and reduce symptoms of anxiety and depression.
-
Massage Therapy: Massage therapy involves the manipulation of soft tissues to relieve muscle tension, reduce pain, and promote relaxation. Massage therapy has been shown to reduce cortisol levels, improve mood, and enhance overall well-being.
-
Herbal Remedies: Certain herbal remedies, such as ashwagandha, rhodiola, and chamomile, have been traditionally used to reduce stress and anxiety. However, it is important to consult with a healthcare professional before using herbal remedies, as they may interact with medications or have potential side effects.
V. Personalized Approaches and Future Directions
The optimal approach to stress management is highly individualized, taking into account the specific stressors, coping styles, and underlying health conditions of each individual. A comprehensive assessment of stress levels, physiological markers, and psychological well-being is essential for developing a personalized treatment plan.
Future research should focus on identifying biomarkers of stress vulnerability and resilience, developing more targeted interventions that address specific aspects of the stress response, and integrating technology-based approaches to enhance accessibility and adherence to stress management programs. Furthermore, exploring the potential of personalized nutrition, genetic testing, and epigenetic modifications to optimize stress resilience represents a promising avenue for future research.
Conclusion
Stress plays a significant role in the progression of chronic diseases, and therapeutic interventions that target the stress response represent a valuable strategy for mitigating disease progression and improving patient outcomes. Lifestyle modifications, psychological therapies, pharmacological interventions, and complementary and alternative medicine modalities all offer potential benefits for managing stress and promoting overall well-being. A personalized approach that considers the individual’s unique needs and preferences is essential for developing an effective stress management plan. By addressing the underlying causes and consequences of chronic stress, we can empower individuals to live healthier, more resilient lives in the face of chronic disease.







Leave a Reply