“The Role of Gut Microbiome in Heart Disease: A Comprehensive Overview
Related Articles The Role of Gut Microbiome in Heart Disease: A Comprehensive Overview
- Integrative Care Models For Complex Chronic Diseases – Part 6: The Role Of Technology And Telehealth
- Integrative Medicine In Leukemia Care: A Comprehensive Approach To Healing
- Public Health Initiatives To Combat Chronic Illnesses – Part 4: Leveraging Technology And Data Analytics
- Cardiac Risk Factors In LGBTQ+ Populations
- Dietary Strategies For Coping With Chronic Diseases – Part 6
Introduction
With great enthusiasm, let’s explore interesting topics related to The Role of Gut Microbiome in Heart Disease: A Comprehensive Overview. Let’s knit interesting information and provide new insights to readers.
Table of Content
The Role of Gut Microbiome in Heart Disease: A Comprehensive Overview
Introduction
Heart disease remains the leading cause of death worldwide, a complex condition influenced by genetics, lifestyle, and environmental factors. In recent years, the spotlight has increasingly turned to the gut microbiome – the vast community of microorganisms residing in our digestive tract – as a significant player in the development and progression of heart disease. This article delves into the intricate relationship between the gut microbiome and heart health, exploring the mechanisms by which gut bacteria can influence cardiovascular risk, and highlighting potential therapeutic strategies targeting the microbiome.
Understanding the Gut Microbiome
The gut microbiome is a complex ecosystem comprising trillions of bacteria, fungi, viruses, and other microorganisms. This community plays a crucial role in various physiological processes, including:
- Digestion and Nutrient Absorption: Gut bacteria aid in breaking down complex carbohydrates, fibers, and other nutrients that the human body cannot digest on its own. They also produce essential vitamins, such as vitamin K and certain B vitamins.
- Immune System Development and Regulation: The gut microbiome interacts extensively with the immune system, helping to train and regulate immune responses. It can promote immune tolerance to harmless substances while mounting defenses against pathogens.
- Metabolic Regulation: Gut bacteria influence energy metabolism, glucose homeostasis, and lipid metabolism. They can affect the levels of circulating lipids, such as cholesterol and triglycerides.
- Production of Bioactive Compounds: Gut bacteria produce a wide range of bioactive compounds, including short-chain fatty acids (SCFAs), trimethylamine N-oxide (TMAO), and bile acid metabolites, which can have both beneficial and detrimental effects on health.
The Gut-Heart Axis
The gut and the heart are connected through a complex network of interactions known as the gut-heart axis. This axis involves several pathways, including:
- Inflammation: The gut microbiome can influence systemic inflammation, a key driver of heart disease. Dysbiosis, an imbalance in the gut microbiome, can lead to increased intestinal permeability ("leaky gut"), allowing bacteria and their products to enter the bloodstream. This triggers an inflammatory response, contributing to the development of atherosclerosis (plaque buildup in arteries) and other cardiovascular problems.
- Metabolic Products: Gut bacteria produce various metabolic products that can directly or indirectly affect heart health. For example, TMAO, a metabolite produced from dietary choline, carnitine, and betaine, has been linked to an increased risk of heart disease. On the other hand, SCFAs, such as butyrate, acetate, and propionate, have been shown to have anti-inflammatory and cardioprotective effects.
- Nervous System Communication: The gut and the brain communicate through the vagus nerve, a major nerve that connects the gut to the brainstem. This bidirectional communication can influence heart rate variability, blood pressure, and other cardiovascular functions.
- Endocrine Function: The gut microbiome can influence the production and release of hormones, such as insulin and glucagon-like peptide-1 (GLP-1), which play a role in glucose metabolism and appetite regulation. These hormones can indirectly affect heart health by influencing risk factors such as diabetes and obesity.
Mechanisms Linking the Gut Microbiome to Heart Disease
Several specific mechanisms have been identified that link the gut microbiome to the development and progression of heart disease:
-
Atherosclerosis: Atherosclerosis is a chronic inflammatory disease characterized by the buildup of plaques in the arteries. The gut microbiome can contribute to atherosclerosis through several mechanisms:
- TMAO Production: As mentioned earlier, TMAO is a metabolite produced by gut bacteria from dietary choline, carnitine, and betaine. TMAO has been shown to promote atherosclerosis by increasing the accumulation of cholesterol in arterial walls, enhancing platelet aggregation, and promoting inflammation.
- Inflammation: Dysbiosis can lead to increased intestinal permeability and the release of bacterial products into the bloodstream, triggering systemic inflammation. Chronic inflammation contributes to the development and progression of atherosclerotic plaques.
- Lipid Metabolism: The gut microbiome can influence lipid metabolism, affecting the levels of circulating cholesterol and triglycerides. Certain gut bacteria can promote the absorption of cholesterol from the diet, while others can help to reduce cholesterol levels.
-
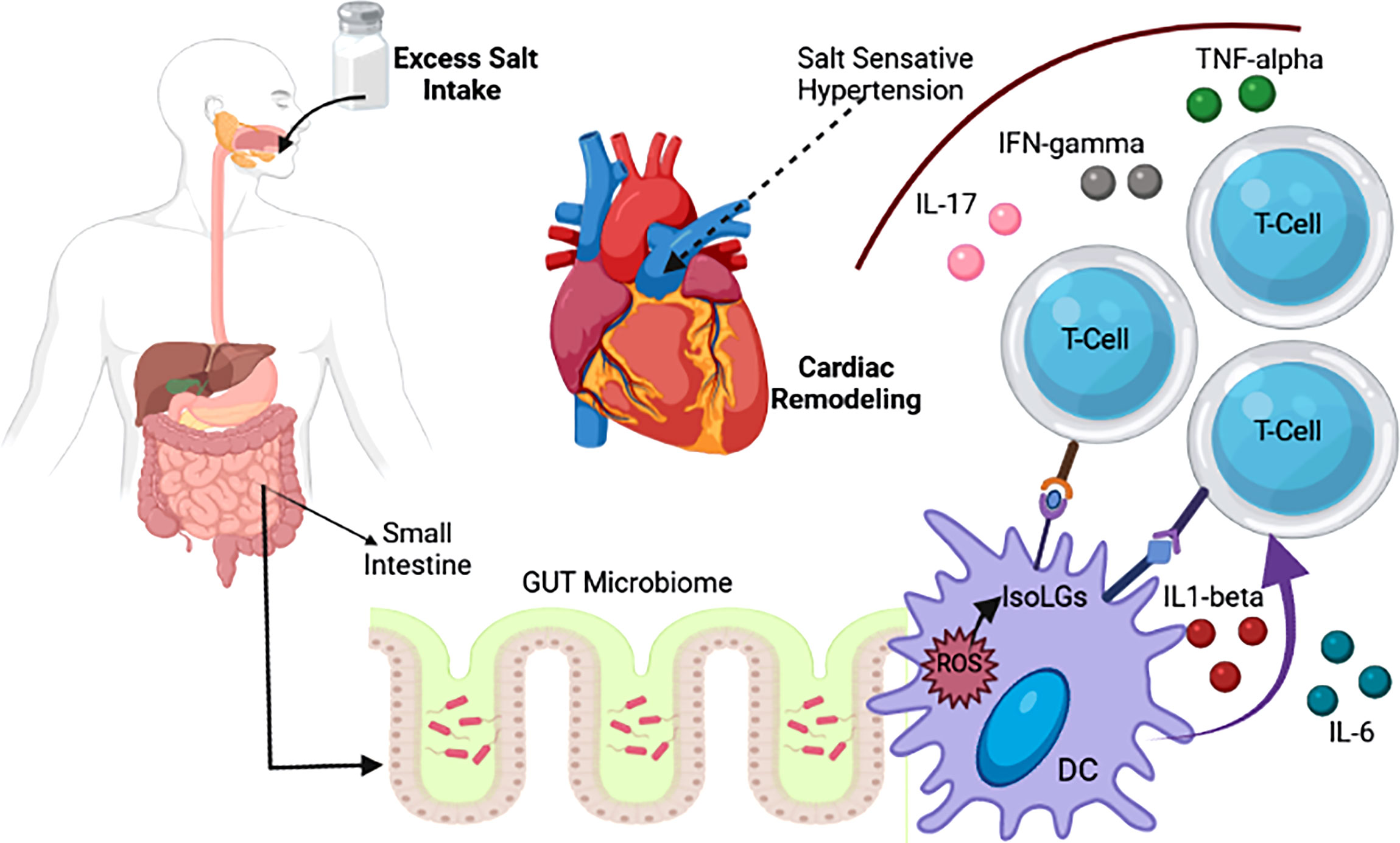
Hypertension: Hypertension, or high blood pressure, is a major risk factor for heart disease. The gut microbiome has been implicated in the development of hypertension through several mechanisms:
- Inflammation: Chronic inflammation can contribute to endothelial dysfunction, a condition in which the lining of blood vessels becomes less flexible and responsive to changes in blood flow. Endothelial dysfunction can lead to increased blood pressure.
- Sodium Metabolism: Some gut bacteria can influence sodium metabolism, affecting the levels of sodium in the body. High sodium levels can lead to increased blood pressure.
- Nitric Oxide Production: Nitric oxide (NO) is a molecule that helps to relax blood vessels and lower blood pressure. The gut microbiome can influence NO production, affecting blood pressure regulation.
-
Heart Failure: Heart failure is a condition in which the heart is unable to pump enough blood to meet the body’s needs. The gut microbiome has been linked to heart failure through several mechanisms:
- Inflammation: Chronic inflammation can contribute to myocardial dysfunction, a condition in which the heart muscle becomes weakened and less able to pump blood effectively.
- Cardiac Remodeling: The gut microbiome can influence cardiac remodeling, a process in which the heart changes its shape and size in response to stress or injury. Cardiac remodeling can lead to heart failure.
- Nutrient Metabolism: The gut microbiome can influence nutrient metabolism, affecting the availability of essential nutrients for heart function.
-
Arrhythmias: Arrhythmias are irregular heartbeats that can increase the risk of stroke and sudden cardiac death. The gut microbiome has been implicated in the development of arrhythmias through several mechanisms:
- Inflammation: Chronic inflammation can disrupt the electrical activity of the heart, leading to arrhythmias.
- Autonomic Nervous System: The gut microbiome can influence the autonomic nervous system, which controls heart rate and rhythm. Imbalances in the autonomic nervous system can lead to arrhythmias.
- Electrolyte Balance: The gut microbiome can influence electrolyte balance, affecting the levels of potassium, magnesium, and calcium in the body. Electrolyte imbalances can disrupt the electrical activity of the heart and lead to arrhythmias.
Factors Influencing the Gut Microbiome
The composition and function of the gut microbiome are influenced by a variety of factors, including:
- Diet: Diet is one of the most important factors influencing the gut microbiome. A diet high in fiber, fruits, and vegetables promotes the growth of beneficial bacteria, while a diet high in processed foods, sugar, and saturated fat can lead to dysbiosis.
- Antibiotics: Antibiotics can disrupt the gut microbiome, killing both harmful and beneficial bacteria. This can lead to dysbiosis and an increased risk of various health problems.
- Age: The gut microbiome changes throughout life, with significant shifts occurring in infancy, childhood, and old age.
- Genetics: Genetic factors can influence the composition of the gut microbiome.
- Environment: Environmental factors, such as exposure to pollutants and toxins, can affect the gut microbiome.
- Lifestyle: Lifestyle factors, such as smoking, alcohol consumption, and physical activity, can influence the gut microbiome.
- Medications: Besides antibiotics, other medications, such as proton pump inhibitors (PPIs) and nonsteroidal anti-inflammatory drugs (NSAIDs), can affect the gut microbiome.
Therapeutic Strategies Targeting the Gut Microbiome
Given the significant role of the gut microbiome in heart disease, therapeutic strategies targeting the microbiome have emerged as promising approaches for preventing and treating cardiovascular conditions. These strategies include:
- Dietary Interventions: Modifying the diet to promote the growth of beneficial bacteria is a key strategy for improving gut health and reducing cardiovascular risk. This includes increasing fiber intake, consuming a variety of fruits and vegetables, and limiting processed foods, sugar, and saturated fat.
- Probiotics: Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. Probiotics can help to restore balance to the gut microbiome and improve various health outcomes, including cardiovascular health.
- Prebiotics: Prebiotics are non-digestible food ingredients that promote the growth of beneficial bacteria in the gut. Prebiotics can be found in foods such as onions, garlic, bananas, and oats.
- Fecal Microbiota Transplantation (FMT): FMT involves transferring fecal material from a healthy donor to a recipient. FMT has shown promise in treating certain gut disorders and may also have potential for improving cardiovascular health.
- Targeted Therapies: Researchers are developing targeted therapies that specifically modulate the gut microbiome to reduce cardiovascular risk. These therapies may include drugs that inhibit the production of TMAO or promote the growth of beneficial bacteria.
Conclusion
The gut microbiome plays a significant role in heart disease, influencing inflammation, metabolism, and other key processes that contribute to cardiovascular risk. Understanding the complex interactions between the gut microbiome and the heart is crucial for developing effective strategies to prevent and treat heart disease. Dietary interventions, probiotics, prebiotics, and other therapeutic approaches targeting the gut microbiome hold promise for improving cardiovascular health and reducing the burden of heart disease. As research in this field continues to advance, we can expect to see even more innovative and effective strategies for harnessing the power of the gut microbiome to promote heart health.








Leave a Reply