“The Impact of HIV on Cardiovascular Health
Related Articles The Impact of HIV on Cardiovascular Health
- Holistic Wellness Programs For Chronic Disease Patients – Part 9: Leveraging Community Support And Peer Mentorship For Sustained Health
- Challenges In Diagnosing Rare Chronic Illnesses – Part 6
- Psychological Resilience In Chronic Disease Patients – Part 5
- Medical Advances In Treating Rare Chronic Conditions – Part 5
- Faktor Lingkungan Dan Risiko Penyakit Kronis – Bagian 10
Introduction
With great enthusiasm, let’s explore interesting topics related to The Impact of HIV on Cardiovascular Health. Come on knit interesting information and provide new insights to readers.
Table of Content
The Impact of HIV on Cardiovascular Health

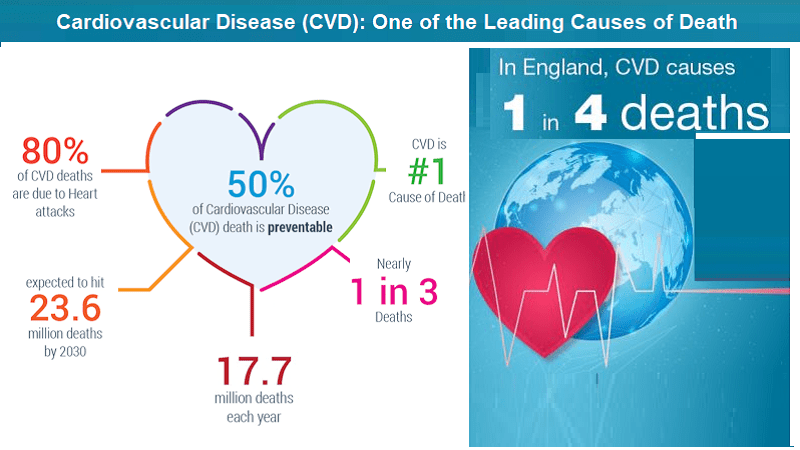
Human Immunodeficiency Virus (HIV) has evolved from a deadly disease to a chronic, manageable condition, largely due to the advent of antiretroviral therapy (ART). However, this success has brought new challenges to the forefront, notably the increased risk of cardiovascular disease (CVD) among people living with HIV (PLWH). This article delves into the complex relationship between HIV and cardiovascular health, exploring the underlying mechanisms, risk factors, clinical manifestations, and strategies for prevention and management.
Understanding HIV and Its Effects
HIV is a retrovirus that primarily targets the immune system, specifically CD4+ T cells, which are crucial for coordinating immune responses. As HIV replicates and destroys these cells, the immune system weakens, making individuals susceptible to opportunistic infections and malignancies. While ART effectively suppresses viral replication and restores immune function, it does not completely eliminate the virus from the body. Chronic inflammation and immune activation persist even in virally suppressed individuals, contributing to long-term health complications, including CVD.
The Link Between HIV and Cardiovascular Disease
The association between HIV and CVD is multifaceted, involving direct viral effects, immune-mediated mechanisms, ART-related factors, and traditional cardiovascular risk factors.
-
Direct Viral Effects: HIV can directly infect and damage cells within the cardiovascular system, including endothelial cells, smooth muscle cells, and cardiomyocytes. This can lead to endothelial dysfunction, inflammation, and impaired vascular function. HIV proteins, such as Tat and gp120, have been shown to promote atherosclerosis and increase the risk of thrombosis.
-
Immune-Mediated Mechanisms: Chronic immune activation and inflammation are hallmarks of HIV infection, even in individuals on ART. This persistent immune activation releases inflammatory cytokines, such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP), which promote endothelial dysfunction, lipid abnormalities, and plaque formation in arteries.
-
Antiretroviral Therapy (ART): While ART is essential for controlling HIV replication and preventing disease progression, certain ART medications have been linked to adverse cardiovascular effects. Some older ART drugs, such as protease inhibitors (PIs), have been associated with dyslipidemia, insulin resistance, and increased risk of myocardial infarction. Newer ART regimens are generally safer, but some may still have metabolic effects that contribute to CVD risk.
-
Traditional Cardiovascular Risk Factors: PLWH often have a higher prevalence of traditional cardiovascular risk factors, such as smoking, hypertension, dyslipidemia, diabetes, and obesity. These risk factors, combined with the effects of HIV and ART, can synergistically increase the risk of CVD.
Specific Cardiovascular Conditions Associated with HIV
PLWH are at increased risk for a range of cardiovascular conditions, including:
-
Atherosclerotic Cardiovascular Disease (ASCVD): This includes coronary artery disease (CAD), peripheral artery disease (PAD), and stroke. PLWH tend to develop ASCVD at a younger age and have more aggressive disease progression compared to HIV-negative individuals.
-
Heart Failure: HIV can directly damage the heart muscle, leading to cardiomyopathy and heart failure. Chronic inflammation and immune activation can also contribute to heart failure development.
-
Pulmonary Hypertension: This condition involves high blood pressure in the arteries of the lungs. HIV-associated pulmonary hypertension (HIV-PAH) is a rare but serious complication that can lead to right heart failure.
-
Pericardial Disease: Inflammation of the pericardium, the sac surrounding the heart, is more common in PLWH. Pericardial effusion and constrictive pericarditis can occur.
-
Venous Thromboembolism (VTE): This includes deep vein thrombosis (DVT) and pulmonary embolism (PE). PLWH have an increased risk of VTE due to inflammation, immune activation, and hypercoagulability.
Risk Factors for Cardiovascular Disease in PLWH
Several factors contribute to the increased risk of CVD in PLWH:
-
HIV-Specific Factors:
- Duration of HIV infection
- Viral load
- CD4+ T cell count
- History of opportunistic infections
- Specific ART regimens
-
Traditional Cardiovascular Risk Factors:
- Smoking
- Hypertension
- Dyslipidemia
- Diabetes
- Obesity
- Family history of CVD
- Sedentary lifestyle
-
Socioeconomic Factors:
- Poverty
- Lack of access to healthcare
- Food insecurity
- Mental health issues
- Substance abuse
Clinical Manifestations of Cardiovascular Disease in PLWH
The symptoms of CVD in PLWH are similar to those in the general population. These may include:
- Chest pain or discomfort
- Shortness of breath
- Fatigue
- Palpitations
- Swelling in the legs or ankles
- Dizziness or lightheadedness
- Sudden weakness or numbness on one side of the body
It is important for PLWH to be aware of these symptoms and seek prompt medical attention if they occur.
Prevention and Management Strategies
Preventing and managing CVD in PLWH requires a comprehensive approach that addresses both HIV-specific and traditional cardiovascular risk factors.
-
Early HIV Diagnosis and Treatment: Early initiation of ART is crucial for suppressing viral replication, restoring immune function, and reducing inflammation. This can help prevent or delay the development of CVD.
-
Cardiovascular Risk Assessment: Regular cardiovascular risk assessment is essential for PLWH. This includes assessing traditional risk factors, such as blood pressure, cholesterol levels, and blood sugar. Risk calculators, such as the Framingham Risk Score or the Pooled Cohort Equations, can be used to estimate the 10-year risk of ASCVD.
-
Lifestyle Modifications: Lifestyle modifications are critical for reducing cardiovascular risk. These include:
- Smoking cessation: Smoking is a major risk factor for CVD and should be avoided.
- Healthy diet: A diet low in saturated fat, cholesterol, and sodium, and high in fruits, vegetables, and whole grains is recommended.
- Regular exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
- Weight management: Maintaining a healthy weight can reduce the risk of CVD.
-
Medications: Medications may be necessary to manage cardiovascular risk factors. These may include:
- Antihypertensive medications: To lower blood pressure.
- Statins: To lower cholesterol levels.
- Antiplatelet medications: Such as aspirin, to prevent blood clots.
- Antidiabetic medications: To control blood sugar levels.
-
ART Selection: When selecting ART regimens, consider the potential cardiovascular effects of different medications. Newer ART drugs are generally safer than older ones, but some may still have metabolic effects.
-
Management of Specific Cardiovascular Conditions: PLWH who develop CVD should be managed according to standard guidelines for the specific condition. This may include medications, procedures such as angioplasty or bypass surgery, and lifestyle modifications.
-
Addressing Socioeconomic Factors: Addressing socioeconomic factors, such as poverty, lack of access to healthcare, and food insecurity, is essential for improving cardiovascular health in PLWH.
The Role of Healthcare Providers
Healthcare providers play a crucial role in preventing and managing CVD in PLWH. They should:
- Screen PLWH for cardiovascular risk factors.
- Provide education and counseling on lifestyle modifications.
- Prescribe medications to manage cardiovascular risk factors.
- Monitor PLWH for signs and symptoms of CVD.
- Refer PLWH to specialists as needed.
- Advocate for policies that improve access to healthcare and address socioeconomic factors.
Conclusion
Cardiovascular disease is a significant concern for people living with HIV. The increased risk of CVD in PLWH is due to a complex interplay of direct viral effects, immune-mediated mechanisms, ART-related factors, and traditional cardiovascular risk factors. Early HIV diagnosis and treatment, cardiovascular risk assessment, lifestyle modifications, and appropriate medications are essential for preventing and managing CVD in PLWH. Healthcare providers play a crucial role in providing comprehensive care to PLWH and addressing the multifaceted challenges they face. By working together, we can improve the cardiovascular health and overall well-being of people living with HIV.







Leave a Reply