“The Connection Between Thyroid Disorders and the Heart
Related Articles The Connection Between Thyroid Disorders and the Heart
- Challenges In Diagnosing Rare Chronic Illnesses – Part 7
- Integrating Mental Health Care In Chronic Disease Clinics – Part 3
- Financial Toxicity Of Leukemia Treatment: Challenges And Solutions
- Running Vs. Cycling: Which Is Better For The Heart?
- Cardiovascular Complications Of COVID-19
Introduction
On this special occasion, we are happy to review interesting topics related to The Connection Between Thyroid Disorders and the Heart. Let’s knit interesting information and provide new insights to readers.
Table of Content
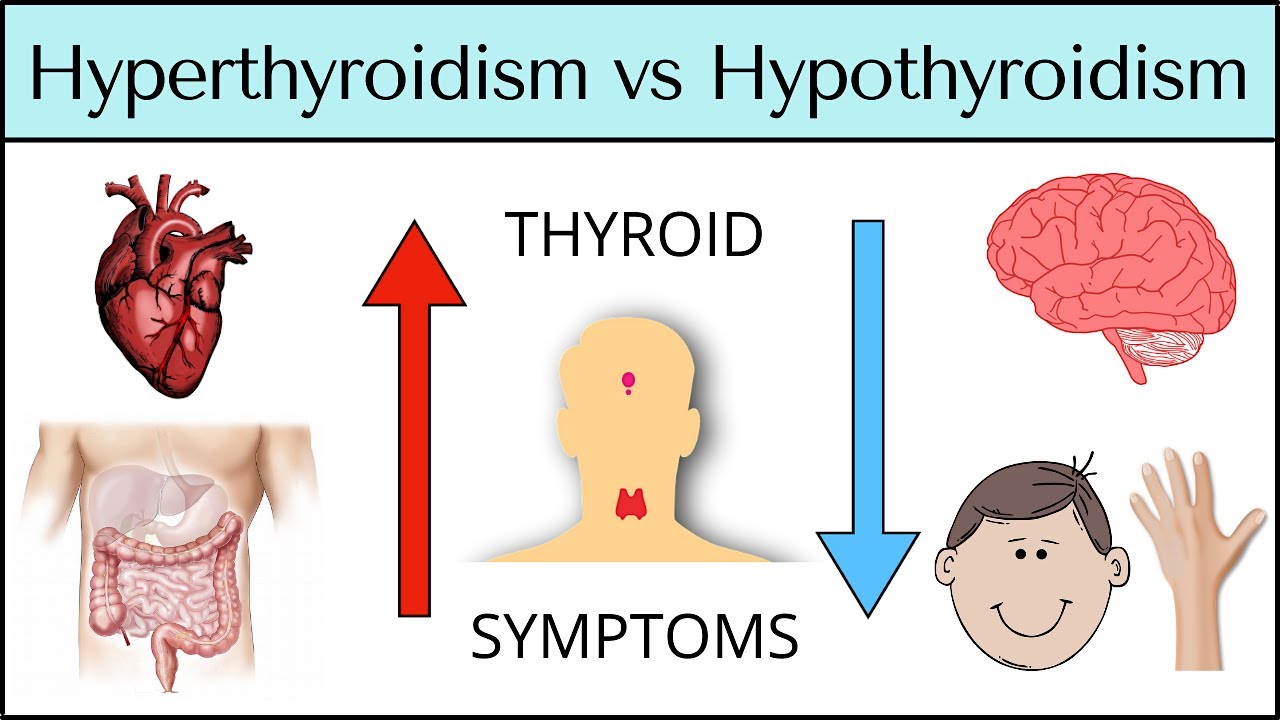
The Connection Between Thyroid Disorders and the Heart

The thyroid gland, a small butterfly-shaped organ located at the base of the neck, plays a pivotal role in regulating metabolism, growth, and development. It produces hormones, primarily thyroxine (T4) and triiodothyronine (T3), which influence nearly every cell in the body. When the thyroid gland malfunctions, leading to either an overproduction (hyperthyroidism) or underproduction (hypothyroidism) of these hormones, a cascade of physiological effects can occur, significantly impacting the cardiovascular system.
The intricate relationship between thyroid disorders and heart health is well-established. Thyroid hormones exert direct and indirect effects on the heart, influencing heart rate, blood pressure, cardiac contractility, and vascular resistance. Consequently, thyroid dysfunction can manifest as a range of cardiovascular complications, underscoring the importance of early diagnosis and management.
Understanding Thyroid Hormones and Their Cardiovascular Effects
Thyroid hormones exert their influence on the heart through several mechanisms:
- Direct Genomic Effects: Thyroid hormones bind to receptors within heart cells (cardiomyocytes), altering gene expression and protein synthesis. This can affect the production of proteins involved in cardiac contractility, ion channel function, and energy metabolism.
- Indirect Non-Genomic Effects: Thyroid hormones can also interact with signaling pathways on the cell membrane, leading to rapid changes in cardiac function.
- Regulation of Adrenergic Receptors: Thyroid hormones modulate the sensitivity of the heart to catecholamines (such as adrenaline and noradrenaline), which are involved in the "fight-or-flight" response.
- Influence on Vascular Tone: Thyroid hormones affect the smooth muscle cells in blood vessels, influencing their ability to constrict or dilate, thereby affecting blood pressure and vascular resistance.
Hyperthyroidism and the Heart
Hyperthyroidism, characterized by excessive thyroid hormone production, places a significant strain on the cardiovascular system. The elevated levels of T3 and T4 lead to:
- Increased Heart Rate: Hyperthyroidism stimulates the sinoatrial (SA) node, the heart’s natural pacemaker, leading to tachycardia (rapid heart rate). This can manifest as palpitations, a sensation of a racing or pounding heart.
- Increased Cardiac Contractility: Thyroid hormones enhance the force of heart muscle contraction, increasing cardiac output (the amount of blood pumped by the heart per minute).
- Decreased Systemic Vascular Resistance: Hyperthyroidism causes vasodilation (widening of blood vessels), reducing the resistance the heart has to pump against.
- Increased Blood Volume: Hyperthyroidism can lead to an increase in blood volume, further increasing the workload on the heart.
Cardiovascular Manifestations of Hyperthyroidism:
The combined effects of hyperthyroidism on the heart can result in a variety of cardiovascular complications:
- Atrial Fibrillation: This is the most common cardiac arrhythmia associated with hyperthyroidism. Atrial fibrillation is characterized by rapid, irregular electrical activity in the atria (upper chambers of the heart), leading to an irregular heartbeat. It increases the risk of stroke and heart failure.
- Heart Failure: In some cases, the chronic strain on the heart caused by hyperthyroidism can lead to heart failure, a condition in which the heart is unable to pump enough blood to meet the body’s needs.
- Angina: Increased heart rate and contractility can increase the heart’s demand for oxygen. In individuals with underlying coronary artery disease, this can trigger angina (chest pain) due to insufficient blood flow to the heart muscle.
- Hypertension: While hyperthyroidism typically reduces systemic vascular resistance, some individuals may develop hypertension (high blood pressure) due to increased cardiac output and other factors.
- Cardiomyopathy: In rare cases, prolonged untreated hyperthyroidism can lead to dilated cardiomyopathy, a condition in which the heart muscle becomes enlarged and weakened.
- Sudden Cardiac Death: Although rare, hyperthyroidism can increase the risk of sudden cardiac death, particularly in individuals with pre-existing heart conditions.
Hypothyroidism and the Heart
Hypothyroidism, characterized by insufficient thyroid hormone production, has the opposite effects on the cardiovascular system compared to hyperthyroidism. The reduced levels of T3 and T4 lead to:
- Decreased Heart Rate: Hypothyroidism slows down the SA node, leading to bradycardia (slow heart rate).
- Decreased Cardiac Contractility: Thyroid hormones are essential for normal heart muscle function. Hypothyroidism reduces the force of heart muscle contraction, decreasing cardiac output.
- Increased Systemic Vascular Resistance: Hypothyroidism causes vasoconstriction (narrowing of blood vessels), increasing the resistance the heart has to pump against.
- Increased Blood Volume: Hypothyroidism can lead to an increase in blood volume, further increasing the workload on the heart.
Cardiovascular Manifestations of Hypothyroidism:
The cardiovascular effects of hypothyroidism can result in the following complications:
- Bradycardia: A slow heart rate is a common finding in hypothyroidism. While mild bradycardia may not be problematic, severe bradycardia can cause fatigue, dizziness, and fainting.
- Heart Failure: Reduced cardiac contractility and increased vascular resistance can contribute to heart failure, particularly in individuals with pre-existing heart conditions.
- Hypertension: Hypothyroidism can lead to diastolic hypertension (elevated diastolic blood pressure) due to increased vascular resistance.
- Hyperlipidemia: Hypothyroidism often leads to elevated levels of cholesterol and triglycerides in the blood, increasing the risk of atherosclerosis (plaque buildup in arteries) and coronary artery disease.
- Coronary Artery Disease: Hypothyroidism increases the risk of developing coronary artery disease, which can lead to angina, heart attack, and sudden cardiac death.
- Pericardial Effusion: In severe cases, hypothyroidism can cause pericardial effusion, an accumulation of fluid around the heart, which can compress the heart and impair its function.
- Prolonged QT Interval: Hypothyroidism can prolong the QT interval on an electrocardiogram (ECG), increasing the risk of potentially life-threatening arrhythmias.
Subclinical Thyroid Disorders and the Heart
Subclinical thyroid disorders are characterized by abnormal thyroid hormone levels but normal thyroid-stimulating hormone (TSH) levels. Subclinical hyperthyroidism is defined as a low TSH level with normal T4 and T3 levels, while subclinical hypothyroidism is defined as a high TSH level with normal T4 and T3 levels.
Even subclinical thyroid disorders can have subtle but significant effects on the cardiovascular system:
- Subclinical Hyperthyroidism: Has been associated with an increased risk of atrial fibrillation, particularly in older adults.
- Subclinical Hypothyroidism: Has been linked to increased levels of cholesterol and triglycerides, as well as an increased risk of coronary artery disease and heart failure.
Diagnosis and Management
Early diagnosis and management of thyroid disorders are crucial to prevent or minimize cardiovascular complications.
- Diagnosis: Thyroid disorders are typically diagnosed through blood tests that measure TSH, T4, and T3 levels. An ECG may be performed to assess heart rhythm and identify any abnormalities.
- Treatment:
- Hyperthyroidism: Treatment options include antithyroid medications (such as methimazole or propylthiouracil), radioactive iodine therapy, or surgery to remove part or all of the thyroid gland. Beta-blockers may be used to control heart rate and other symptoms.
- Hypothyroidism: Treatment involves thyroid hormone replacement therapy with levothyroxine (synthetic T4). The dosage is carefully adjusted to normalize TSH levels and alleviate symptoms.
Importance of Monitoring and Follow-Up
Individuals with thyroid disorders should undergo regular monitoring of their thyroid hormone levels and cardiovascular health. This includes:
- Regular Blood Tests: To ensure that thyroid hormone levels are within the target range.
- Blood Pressure Monitoring: To detect and manage hypertension.
- Cholesterol Screening: To identify and treat hyperlipidemia.
- ECG: To monitor heart rhythm and detect any abnormalities.
- Echocardiogram: To assess heart structure and function, particularly in individuals with heart failure.
Conclusion
The connection between thyroid disorders and the heart is undeniable. Both hyperthyroidism and hypothyroidism can have profound effects on the cardiovascular system, leading to a range of complications. Early diagnosis, appropriate treatment, and regular monitoring are essential to protect heart health and improve outcomes for individuals with thyroid dysfunction. If you suspect you may have a thyroid disorder or have a family history of thyroid disease, it is important to consult with a healthcare professional for evaluation and management.







Leave a Reply