“Targeted Therapy in Leukemia: Precision Medicine Approaches
Related Articles Targeted Therapy in Leukemia: Precision Medicine Approaches
- Dietary Strategies For Coping With Chronic Diseases – Part 5
- Public Health Initiatives To Combat Chronic Illnesses
- Sleep Disorders And Chronic Disease Relationships – Part 9
- Psychological Resilience In Chronic Disease Patients – Part 8
- Dietary Strategies For Coping With Chronic Diseases – Part 10
Introduction
We will be happy to explore interesting topics related to Targeted Therapy in Leukemia: Precision Medicine Approaches. Let’s knit interesting information and provide new insights to readers.
Table of Content
Targeted Therapy in Leukemia: Precision Medicine Approaches

Introduction
Leukemia, a group of cancers affecting the blood and bone marrow, has long posed a significant challenge in oncology. Traditional treatments like chemotherapy, radiation, and stem cell transplantation have improved outcomes for many patients. However, these approaches often come with significant side effects due to their lack of specificity, damaging healthy cells alongside cancerous ones.
The advent of targeted therapy has revolutionized leukemia treatment by offering more precise and effective strategies. These therapies exploit specific vulnerabilities within leukemia cells, leading to improved outcomes and reduced toxicity. This article explores the principles of targeted therapy in leukemia, highlighting the key targets, available drugs, clinical applications, and future directions of this precision medicine approach.
Understanding Leukemia and its Molecular Landscape
Leukemia is broadly classified into acute and chronic forms, each with subtypes based on the lineage of the affected blood cells (myeloid or lymphoid). Acute leukemias, such as acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL), are characterized by rapid proliferation of immature blood cells, while chronic leukemias, like chronic myeloid leukemia (CML) and chronic lymphocytic leukemia (CLL), progress more slowly.
The development of leukemia is driven by genetic and molecular abnormalities that disrupt normal blood cell development and function. These abnormalities can include:
- Gene Mutations: Mutations in genes involved in cell growth, differentiation, and apoptosis (programmed cell death).
- Chromosomal Translocations: Rearrangements of chromosomes that create fusion genes with altered functions.
- Epigenetic Modifications: Changes in DNA methylation and histone modification patterns that affect gene expression.
Identifying these specific molecular drivers is crucial for developing targeted therapies that selectively inhibit their activity.
Principles of Targeted Therapy
Targeted therapy differs from traditional chemotherapy in its mechanism of action. Instead of indiscriminately killing rapidly dividing cells, targeted therapies interfere with specific molecules or pathways that are essential for cancer cell growth, survival, and proliferation.
The key principles of targeted therapy include:
- Identifying the Target: Identifying a molecule or pathway that is uniquely or disproportionately important for the survival or proliferation of leukemia cells.
- Developing a Drug: Designing or discovering a drug that specifically inhibits the activity of the target molecule.
- Selecting Patients: Identifying patients whose leukemia cells express the target molecule or pathway, making them more likely to respond to the targeted therapy.
- Monitoring Response: Assessing the effectiveness of the targeted therapy by monitoring changes in disease burden, molecular markers, and patient outcomes.
Key Targets and Targeted Therapies in Leukemia
Several molecular targets have been successfully exploited in the development of targeted therapies for leukemia. Some of the most important targets and their corresponding drugs are:
-
BCR-ABL1 (CML): The Philadelphia chromosome, resulting from a translocation between chromosomes 9 and 22, creates the BCR-ABL1 fusion gene. This gene encodes a constitutively active tyrosine kinase that drives uncontrolled proliferation of myeloid cells in CML.
- Targeted Therapies: Tyrosine kinase inhibitors (TKIs) such as imatinib, dasatinib, nilotinib, bosutinib, and ponatinib specifically inhibit the BCR-ABL1 kinase activity. These drugs have dramatically improved outcomes for CML patients, transforming it from a deadly disease to a manageable chronic condition.
-
FLT3 (AML): FMS-like tyrosine kinase 3 (FLT3) is a receptor tyrosine kinase that is frequently mutated in AML. FLT3 mutations, particularly internal tandem duplications (ITDs) and tyrosine kinase domain (TKD) mutations, lead to constitutive activation of the receptor and increased cell proliferation.
- Targeted Therapies: FLT3 inhibitors such as midostaurin, gilteritinib, and quizartinib specifically target FLT3-mutated AML cells. These drugs have shown promising results in clinical trials, particularly in combination with chemotherapy.
-
IDH1/2 (AML): Isocitrate dehydrogenase 1 and 2 (IDH1/2) are metabolic enzymes that are mutated in a subset of AML patients. IDH1/2 mutations lead to the production of an oncometabolite called 2-hydroxyglutarate (2-HG), which disrupts normal cellular differentiation and promotes leukemogenesis.
- Targeted Therapies: IDH1/2 inhibitors such as ivosidenib and enasidenib specifically inhibit the mutant IDH1/2 enzymes, leading to a reduction in 2-HG levels and restoration of normal differentiation.
-
BCL-2 (CLL and AML): B-cell lymphoma 2 (BCL-2) is an anti-apoptotic protein that is overexpressed in many leukemia cells, particularly in CLL and AML. BCL-2 overexpression inhibits programmed cell death, allowing leukemia cells to survive and proliferate.
- Targeted Therapies: BCL-2 inhibitors such as venetoclax specifically bind to and inhibit BCL-2, restoring the ability of leukemia cells to undergo apoptosis. Venetoclax has shown remarkable efficacy in CLL and is being investigated in combination with other therapies for AML.
-
CD30 (Hodgkin Lymphoma transformed into T-cell Lymphoma): CD30 is a type I transmembrane protein belonging to the tumor necrosis factor receptor superfamily and is a marker for Hodgkin lymphoma (HL) and anaplastic large cell lymphoma (ALCL).
- Targeted Therapies: Brentuximab vedotin is an antibody-drug conjugate (ADC) composed of an anti-CD30 monoclonal antibody conjugated to monomethyl auristatin E (MMAE), a microtubule-disrupting agent.
-
CD19 and CD22 (ALL): CD19 and CD22 are B-cell surface proteins that are expressed on most B-cell ALL cells.
- Targeted Therapies: Blinatumomab is a bispecific T-cell engager (BiTE) antibody that binds to CD19 on B-cell ALL cells and CD3 on T cells, bringing them into close proximity and activating T cells to kill the leukemia cells. Inotuzumab ozogamicin is an antibody-drug conjugate that targets CD22 and delivers a cytotoxic payload to leukemia cells.
Clinical Applications of Targeted Therapy in Leukemia
Targeted therapies have significantly improved outcomes for patients with various types of leukemia. Some of the key clinical applications include:
- CML: TKIs have revolutionized CML treatment, allowing most patients to achieve complete cytogenetic and molecular remission.
- AML: FLT3 inhibitors, IDH1/2 inhibitors, and BCL-2 inhibitors have shown promise in improving remission rates and overall survival for patients with specific genetic mutations.
- ALL: Blinatumomab and inotuzumab ozogamicin have improved outcomes for patients with relapsed or refractory B-cell ALL.
- CLL: BCL-2 inhibitors, such as venetoclax, have become a cornerstone of CLL treatment, offering durable remissions and improved quality of life.
Challenges and Future Directions
Despite the significant advances in targeted therapy for leukemia, several challenges remain:
- Drug Resistance: Leukemia cells can develop resistance to targeted therapies through various mechanisms, including mutations in the target molecule, activation of alternative signaling pathways, and increased drug efflux.
- Off-Target Effects: Some targeted therapies can have off-target effects, leading to adverse events.
- Limited Availability of Targets: Not all leukemia patients have targetable mutations or pathways.
- Cost: The high cost of targeted therapies can be a barrier to access for some patients.
Future directions in targeted therapy for leukemia include:
- Developing New Targets and Drugs: Identifying new molecular targets and developing novel drugs that can overcome resistance and improve efficacy.
- Combination Therapies: Combining targeted therapies with other treatments, such as chemotherapy, immunotherapy, or stem cell transplantation, to improve outcomes.
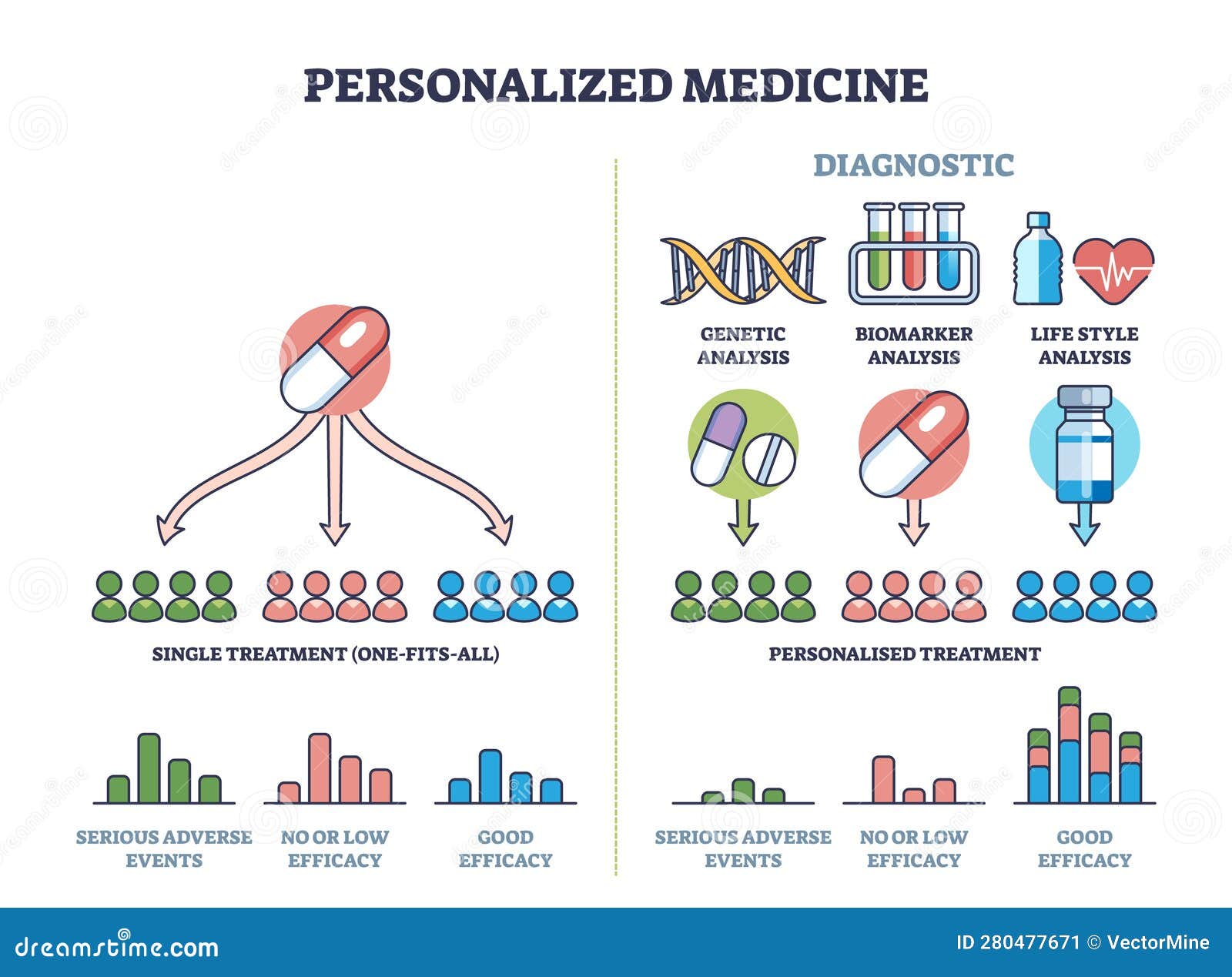
- Personalized Medicine Approaches: Using genomic and molecular profiling to identify the most appropriate targeted therapy for each patient.
- Immunotherapy: Combining targeted therapies with immunotherapeutic approaches, such as checkpoint inhibitors or CAR T-cell therapy, to enhance anti-leukemia immune responses.
- Epigenetic Therapies: Targeting epigenetic modifications to restore normal gene expression patterns in leukemia cells.
Conclusion
Targeted therapy has transformed the treatment of leukemia by offering more precise and effective strategies that exploit specific vulnerabilities within leukemia cells. The development of TKIs for CML, FLT3 inhibitors, IDH1/2 inhibitors, and BCL-2 inhibitors for AML, and blinatumomab and inotuzumab ozogamicin for ALL have significantly improved outcomes for patients with these diseases.
Despite the challenges of drug resistance and off-target effects, the future of targeted therapy in leukemia is bright. Ongoing research is focused on identifying new targets, developing novel drugs, and combining targeted therapies with other treatment modalities to further improve outcomes and quality of life for patients with leukemia. By embracing precision medicine approaches, we can tailor treatment strategies to the individual characteristics of each patient’s leukemia, leading to more effective and less toxic therapies.







Leave a Reply