“Rheumatic Heart Disease in Developing Countries: A Persistent Burden
Related Articles Rheumatic Heart Disease in Developing Countries: A Persistent Burden
- The Role Of Genetics In Chronic Disease Development – Part 9
- Social Determinants Of Health And Chronic Disease Outcomes – Part 9
- Preventive Screening Guidelines For Chronic Conditions – Part 7
- Public Policy And Chronic Disease Prevention Strategies – Part 2
- Psychological Resilience In Chronic Disease Patients: Part 4 – Cultivating Resilience: Practical Strategies And Future Directions
Introduction
We will be happy to explore interesting topics related to Rheumatic Heart Disease in Developing Countries: A Persistent Burden. Let’s knit interesting information and provide new insights to readers.
Table of Content
Rheumatic Heart Disease in Developing Countries: A Persistent Burden

Rheumatic heart disease (RHD) remains a significant public health challenge in developing countries, disproportionately affecting children and young adults. This chronic heart condition results from acute rheumatic fever (ARF), an inflammatory response triggered by group A Streptococcus (GAS) bacterial infection, commonly known as strep throat. While ARF itself can cause temporary joint pain, fever, and rash, the most severe consequence is the potential for long-term damage to the heart valves, leading to RHD.
Epidemiology: A Tale of Disparity
The global burden of RHD is heavily skewed towards low- and middle-income countries (LMICs). While RHD has been virtually eliminated in most developed nations due to improved sanitation, access to healthcare, and widespread use of antibiotics, it persists as a major cause of cardiovascular morbidity and mortality in developing regions.
Several factors contribute to this disparity:
- Poverty and Overcrowding: Overcrowded living conditions and poor sanitation facilitate the spread of GAS infections, increasing the risk of ARF and subsequent RHD.
- Limited Access to Healthcare: In many developing countries, access to timely and effective healthcare is limited. This includes inadequate diagnosis and treatment of strep throat, as well as a lack of secondary prophylaxis (regular antibiotic injections) to prevent recurrent ARF attacks.
- Malnutrition: Malnutrition weakens the immune system, making individuals more susceptible to GAS infections and ARF.
- Lack of Awareness: Limited awareness among the public and healthcare providers about the signs and symptoms of ARF and RHD contributes to delayed diagnosis and treatment.
Pathophysiology: The Road to Heart Damage
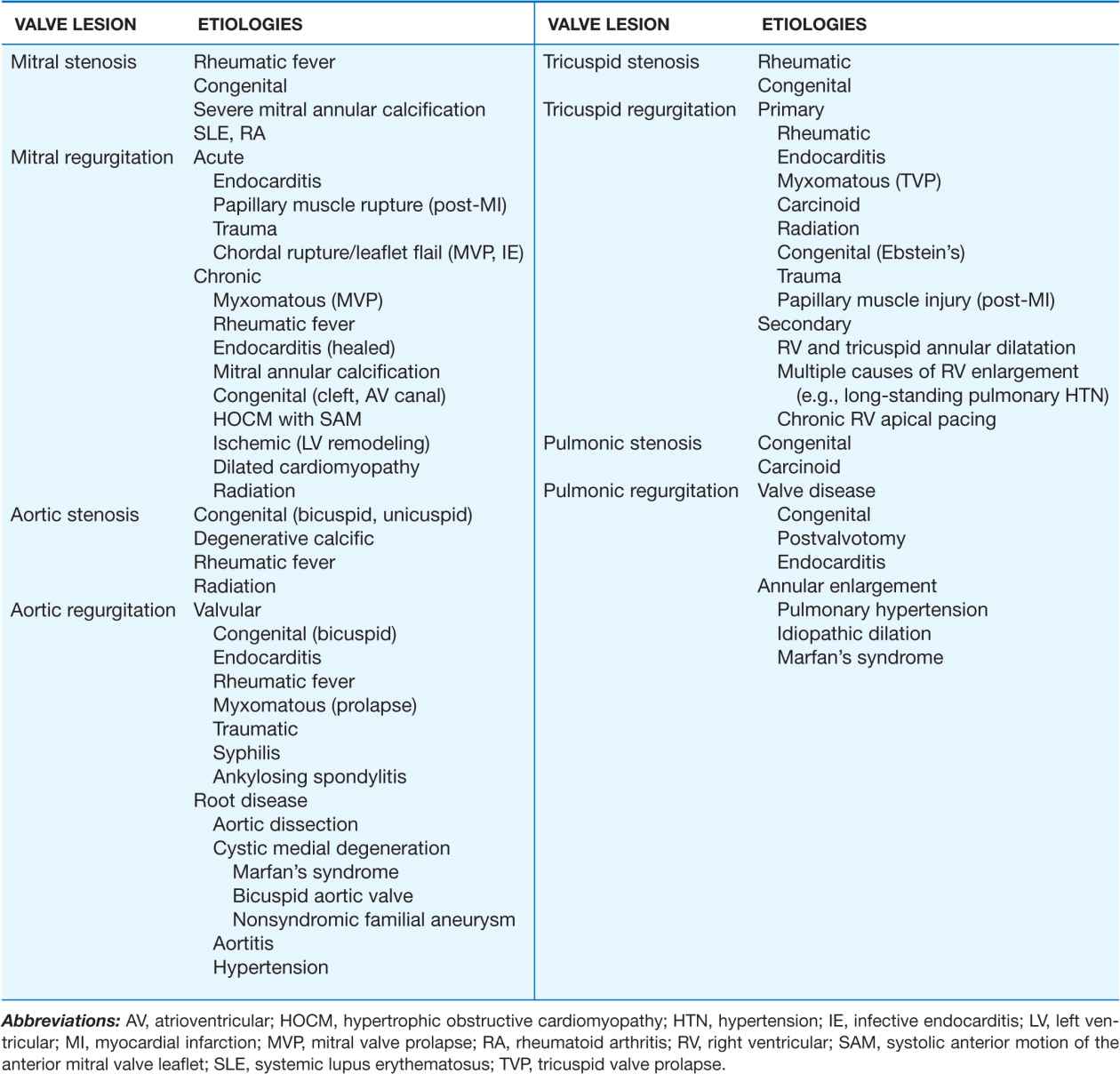
ARF is an autoimmune reaction that occurs when the body’s immune system mistakenly attacks its own tissues after a GAS infection. The heart, joints, brain, and skin can be affected. In the heart, inflammation can damage the heart valves, particularly the mitral and aortic valves. This damage can lead to valve stenosis (narrowing) or regurgitation (leakage), impairing the heart’s ability to pump blood efficiently.
Over time, repeated ARF attacks can cause progressive and irreversible damage to the heart valves, leading to chronic RHD. The heart muscle itself may also be affected, leading to heart failure.
Clinical Manifestations: Recognizing the Signs
The clinical manifestations of RHD vary depending on the severity of valve damage and the presence of heart failure. Common symptoms include:
- Shortness of Breath: This is often the earliest and most common symptom, particularly during exertion.
- Fatigue: Reduced cardiac output can lead to fatigue and weakness.
- Chest Pain: Chest pain may occur, especially during physical activity.
- Palpitations: Irregular heartbeats or palpitations may be felt.
- Swelling: Swelling of the ankles and legs (edema) is a sign of heart failure.
- Heart Murmurs: Abnormal heart sounds (murmurs) can be heard during a physical examination, indicating valve abnormalities.
Diagnosis: Identifying the Problem
Diagnosing RHD involves a combination of clinical evaluation, medical history, and diagnostic tests. The modified Jones criteria are commonly used to diagnose ARF, which is a precursor to RHD. These criteria include major and minor manifestations of ARF, such as:
Major Manifestations:
- Carditis (inflammation of the heart)
- Polyarthritis (inflammation of multiple joints)
- Chorea (involuntary movements)
- Erythema marginatum (a skin rash)
- Subcutaneous nodules (painless lumps under the skin)
Minor Manifestations:
- Fever
- Arthralgia (joint pain)
- Elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP)
- Prolonged PR interval on electrocardiogram (ECG)
Diagnostic tests for RHD include:
- Echocardiography: This is the most important diagnostic tool for RHD. It uses ultrasound waves to create images of the heart, allowing doctors to assess the structure and function of the heart valves.
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and can detect abnormalities in heart rhythm and conduction.
- Chest X-ray: This can help assess the size and shape of the heart and detect any fluid in the lungs.
- Blood Tests: Blood tests can help detect evidence of a recent GAS infection and inflammation.
Management: A Multifaceted Approach
The management of RHD aims to prevent recurrent ARF attacks, treat heart failure, and manage complications. The following strategies are commonly employed:
- Primary Prevention: This involves preventing the initial GAS infection by promoting good hygiene practices and providing prompt treatment for strep throat with antibiotics.
- Secondary Prophylaxis: This involves regular antibiotic injections (usually penicillin) to prevent recurrent ARF attacks. Secondary prophylaxis is crucial for individuals who have had ARF or RHD.
- Medical Management: Medications are used to manage heart failure symptoms, such as diuretics to reduce fluid retention, ACE inhibitors to lower blood pressure, and beta-blockers to slow the heart rate.
- Surgical Intervention: In severe cases of RHD, surgery may be necessary to repair or replace damaged heart valves. Valve replacement is a major surgical procedure that requires specialized expertise and resources.
- Rehabilitation: Cardiac rehabilitation programs can help patients improve their physical fitness and quality of life.
Prevention Strategies: Breaking the Cycle
Preventing RHD requires a comprehensive approach that addresses the underlying social, economic, and environmental factors that contribute to its prevalence. Key prevention strategies include:
- Improving Sanitation and Hygiene: Promoting good hygiene practices, such as frequent handwashing, can reduce the spread of GAS infections.
- Ensuring Access to Healthcare: Improving access to timely and effective healthcare, including diagnosis and treatment of strep throat, is essential.
- Implementing School-Based Programs: School-based programs can raise awareness about ARF and RHD, promote hygiene practices, and provide screening for strep throat.
- Strengthening Surveillance Systems: Establishing surveillance systems to monitor the incidence of ARF and RHD can help track progress and identify areas where interventions are needed.
- Advocacy and Awareness Campaigns: Raising awareness among the public, healthcare providers, and policymakers about the burden of RHD is crucial for mobilizing resources and support for prevention and control efforts.
Challenges and Future Directions
Despite progress in understanding and managing RHD, significant challenges remain:
- Limited Resources: Many developing countries lack the resources needed to implement comprehensive RHD prevention and control programs.
- Lack of Infrastructure: Inadequate healthcare infrastructure, including diagnostic facilities and specialized cardiac centers, limits access to care.
- Shortage of Trained Personnel: There is a shortage of healthcare professionals trained in the diagnosis and management of RHD.
- Cost of Treatment: The cost of medications, surgery, and long-term care for RHD can be prohibitive for many patients in developing countries.
Future directions for RHD research and control include:
- Developing a Vaccine: A vaccine against GAS infection could potentially eliminate ARF and RHD.
- Improving Diagnostic Tools: Developing more accurate and affordable diagnostic tools for ARF and RHD is essential.
- Strengthening Healthcare Systems: Strengthening healthcare systems in developing countries is crucial for improving access to care and reducing the burden of RHD.
- Promoting International Collaboration: International collaboration is needed to share knowledge, resources, and best practices for RHD prevention and control.
Conclusion
Rheumatic heart disease remains a significant public health problem in developing countries, causing substantial morbidity and mortality. Addressing this challenge requires a multifaceted approach that includes primary prevention, secondary prophylaxis, medical management, and surgical intervention. By improving sanitation, ensuring access to healthcare, raising awareness, and strengthening healthcare systems, we can reduce the burden of RHD and improve the lives of millions of people in developing countries.







Leave a Reply