“Pulmonary Hypertension and the Heart
Related Articles Pulmonary Hypertension and the Heart
- Social Support Networks For Chronic Disease Patients – Part 8: Cultivating Resilience Through Strong Social Connections
- Leukemia Treatment Guidelines: Updates And Recommendations
- Emerging Technologies In Leukemia Research: A Glimpse Into The Future Of Diagnosis And Treatment
- Telemedicine And Remote Monitoring For Chronic Illness Care – Part 8: Ethical Considerations, Data Privacy, And Future Directions
- Holistic Approaches To Chronic Disease Prevention – Part 3
Introduction
With great enthusiasm, let’s explore interesting topics related to Pulmonary Hypertension and the Heart. Let’s knit interesting information and provide new insights to readers.
Table of Content
Pulmonary Hypertension and the Heart
Pulmonary hypertension (PH) is a progressive and life-threatening condition characterized by elevated blood pressure in the pulmonary arteries, the blood vessels that carry blood from the heart to the lungs. This increased pressure puts a strain on the right side of the heart, leading to right ventricular hypertrophy (RVH) and, eventually, right heart failure, also known as cor pulmonale. Understanding the intricate relationship between pulmonary hypertension and the heart is crucial for effective diagnosis, management, and improved outcomes for patients with this complex disorder.
The Pulmonary Circulation: A Brief Overview
To appreciate the impact of pulmonary hypertension on the heart, it’s essential to understand the basics of pulmonary circulation. Unlike the systemic circulation, which delivers oxygenated blood to the entire body, the pulmonary circulation has a more limited scope:
- Right Ventricle: The right ventricle of the heart pumps deoxygenated blood into the pulmonary artery.
- Pulmonary Artery: The pulmonary artery branches into the left and right pulmonary arteries, which carry blood to the corresponding lungs.
- Pulmonary Capillaries: Within the lungs, the pulmonary arteries further divide into a network of tiny capillaries that surround the air sacs (alveoli).
- Gas Exchange: Oxygen from inhaled air diffuses into the blood, while carbon dioxide from the blood diffuses into the alveoli to be exhaled.
- Pulmonary Veins: Oxygenated blood then flows from the pulmonary capillaries into the pulmonary veins.
- Left Atrium: The pulmonary veins carry the oxygenated blood back to the left atrium of the heart.
- Left Ventricle: Finally, the left ventricle pumps the oxygenated blood into the aorta for distribution throughout the body.
In a healthy individual, the pulmonary circulation operates at a lower pressure than the systemic circulation. This lower pressure is necessary for efficient gas exchange and to prevent fluid from leaking out of the pulmonary capillaries into the air sacs.
Pulmonary Hypertension: A Definition and Classification
Pulmonary hypertension is defined as a mean pulmonary artery pressure (mPAP) of 20 mmHg or higher at rest, as assessed by right heart catheterization. This threshold was revised downward from 25 mmHg in recent years to reflect a better understanding of the disease and its impact on patient outcomes.
The World Health Organization (WHO) classifies pulmonary hypertension into five main groups based on etiology and underlying mechanisms:
- Pulmonary Arterial Hypertension (PAH): This group includes idiopathic PAH (iPAH), heritable PAH, drug- and toxin-induced PAH, and PAH associated with other conditions such as connective tissue diseases, HIV infection, and congenital heart disease.
- Pulmonary Hypertension Due to Left Heart Disease: This is the most common cause of PH and results from elevated pressures in the left side of the heart, such as mitral valve disease, aortic valve disease, or left ventricular dysfunction.
- Pulmonary Hypertension Due to Lung Diseases and/or Hypoxia: This group includes PH associated with chronic obstructive pulmonary disease (COPD), interstitial lung disease, sleep-disordered breathing, and chronic exposure to high altitude.
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH): CTEPH occurs when blood clots in the pulmonary arteries do not dissolve properly, leading to chronic obstruction and increased pulmonary artery pressure.
- Pulmonary Hypertension with Unclear Multifactorial Mechanisms: This group includes PH associated with hematologic disorders, systemic diseases, metabolic disorders, and other conditions.
The Impact of Pulmonary Hypertension on the Heart
The primary consequence of pulmonary hypertension on the heart is the increased workload placed on the right ventricle. The right ventricle must pump blood against a higher resistance in the pulmonary arteries, leading to a cascade of structural and functional changes:
- Right Ventricular Hypertrophy (RVH): Initially, the right ventricle adapts to the increased pressure by thickening its walls, a process known as hypertrophy. This compensatory mechanism allows the right ventricle to maintain cardiac output despite the elevated pulmonary artery pressure.
- Right Ventricular Dilation: Over time, the right ventricle may become dilated as it struggles to pump blood against the persistently high pressure. Dilation further impairs the right ventricle’s ability to contract effectively.
- Right Ventricular Dysfunction: As RVH and dilation progress, the right ventricle eventually becomes dysfunctional. It is no longer able to pump enough blood to meet the body’s needs, leading to symptoms of heart failure.
- Tricuspid Regurgitation: The increased pressure in the right ventricle can also cause the tricuspid valve, which separates the right atrium and right ventricle, to leak. This condition, known as tricuspid regurgitation, further reduces the efficiency of the heart.
- Interventricular Dependence: The right and left ventricles share the interventricular septum, the wall that separates them. In PH, the enlarged right ventricle can compress the left ventricle, impairing its ability to fill and contract properly. This phenomenon is known as interventricular dependence.
- Cor Pulmonale: Cor pulmonale is defined as right ventricular enlargement and failure secondary to pulmonary hypertension. It represents the end-stage of the cardiac complications of PH.
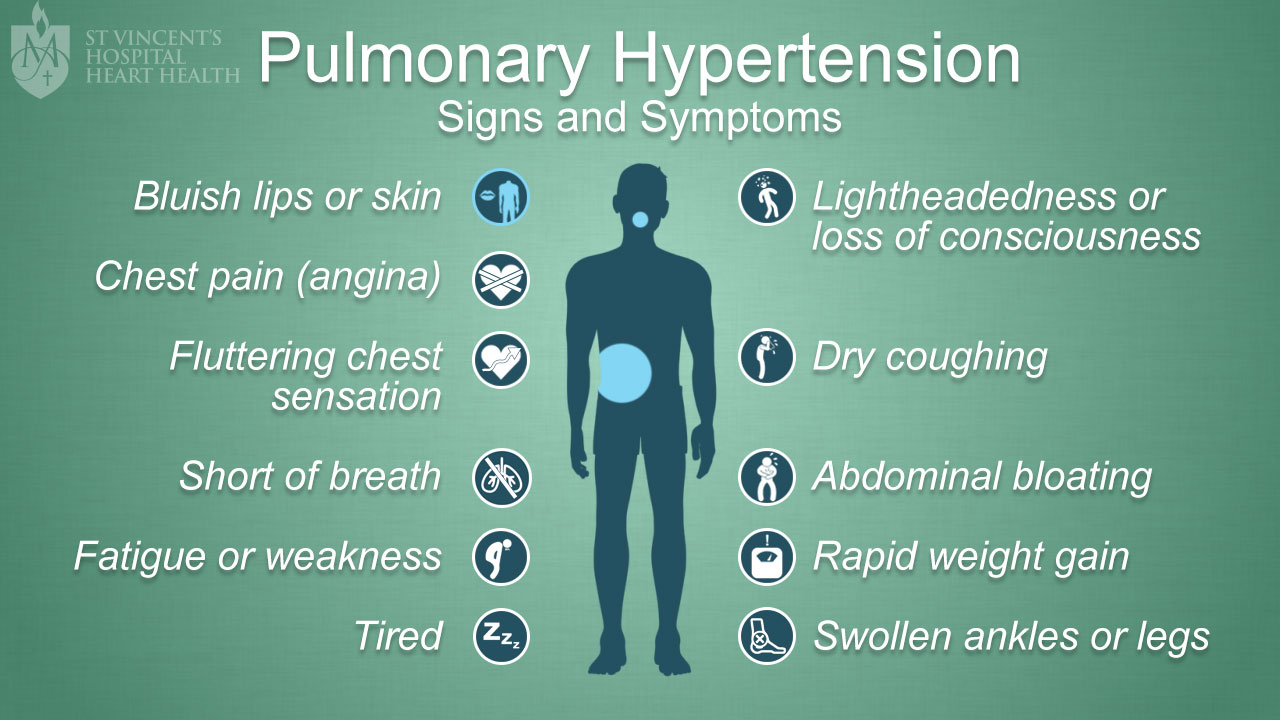
Symptoms of Pulmonary Hypertension and Heart Failure
The symptoms of pulmonary hypertension and right heart failure can be nonspecific and may overlap with other conditions, making diagnosis challenging. Common symptoms include:
- Shortness of breath (dyspnea), especially during exertion
- Fatigue
- Chest pain
- Dizziness or lightheadedness
- Swelling in the ankles, legs, and abdomen (edema)
- Cyanosis (bluish discoloration of the skin)
- Rapid heart rate (tachycardia)
- Palpitations
- Cough
- Wheezing
Diagnosis of Pulmonary Hypertension and Assessment of Cardiac Function
Diagnosing pulmonary hypertension and assessing its impact on the heart requires a combination of clinical evaluation, noninvasive tests, and invasive procedures:
- Clinical Evaluation: A thorough medical history and physical examination are essential to identify potential risk factors and symptoms of PH.
- Echocardiography: Echocardiography is a noninvasive imaging technique that uses ultrasound waves to visualize the heart’s structure and function. It can estimate pulmonary artery pressure, assess right ventricular size and function, and detect tricuspid regurgitation.
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can reveal signs of right ventricular hypertrophy or strain.
- Chest X-ray: A chest X-ray can show enlargement of the pulmonary arteries and right ventricle.
- Pulmonary Function Tests (PFTs): PFTs assess lung function and can help differentiate PH due to lung disease from other causes.
- Ventilation-Perfusion (V/Q) Scan: A V/Q scan is used to detect blood clots in the pulmonary arteries and can help diagnose CTEPH.
- Computed Tomography (CT) Scan: A CT scan of the chest can provide detailed images of the lungs and pulmonary arteries, helping to identify underlying lung diseases or blood clots.
- Right Heart Catheterization: Right heart catheterization is the gold standard for diagnosing pulmonary hypertension. It involves inserting a catheter into the pulmonary artery to directly measure pulmonary artery pressure and assess cardiac output.
Management of Pulmonary Hypertension and Heart Failure
The management of pulmonary hypertension and right heart failure is complex and requires a multidisciplinary approach involving cardiologists, pulmonologists, and other specialists. Treatment strategies aim to:
- Reduce pulmonary artery pressure
- Improve right ventricular function
- Relieve symptoms
- Slow disease progression
- Improve quality of life
Treatment options include:
- General Measures: General measures include lifestyle modifications such as smoking cessation, weight management, and regular exercise. Patients should also receive vaccinations against influenza and pneumococcal pneumonia.
- Diuretics: Diuretics help reduce fluid overload and alleviate symptoms of edema.
- Oxygen Therapy: Supplemental oxygen is used to improve oxygen levels in patients with PH due to lung disease or hypoxia.
-
Pulmonary Vasodilators: Pulmonary vasodilators are medications that relax the pulmonary arteries and lower pulmonary artery pressure. These medications include:
- Prostacyclin analogs (e.g., epoprostenol, treprostinil, iloprost)
- Endothelin receptor antagonists (ERAs) (e.g., bosentan, ambrisentan, macitentan)
- Phosphodiesterase-5 (PDE-5) inhibitors (e.g., sildenafil, tadalafil)
- Soluble guanylate cyclase (sGC) stimulators (e.g., riociguat)
- Anticoagulation: Anticoagulation with warfarin or other blood thinners may be used in patients with CTEPH to prevent further blood clot formation.
- Pulmonary Thromboendarterectomy (PTE): PTE is a surgical procedure to remove blood clots from the pulmonary arteries in patients with CTEPH.
- Balloon Pulmonary Angioplasty (BPA): BPA is a minimally invasive procedure to dilate narrowed pulmonary arteries in patients with CTEPH who are not candidates for PTE.
- Lung Transplantation: Lung transplantation may be considered in patients with severe PH who do not respond to other treatments.
- Atrial Septostomy: Creating an opening between the right and left atria to relieve pressure on the right heart.
Conclusion
Pulmonary hypertension is a serious condition that has a profound impact on the heart, leading to right ventricular hypertrophy, right heart failure, and ultimately, cor pulmonale. Early diagnosis, accurate assessment of cardiac function, and appropriate management are crucial for improving outcomes and quality of life for patients with PH. A multidisciplinary approach involving cardiologists, pulmonologists, and other specialists is essential to provide comprehensive care and optimize treatment strategies. Continued research is needed to develop new and more effective therapies for pulmonary hypertension and to better understand the complex interplay between the lungs and the heart in this challenging disease.








Leave a Reply