“Pregnancy and Heart Disease: Risks for Mothers
Related Articles Pregnancy and Heart Disease: Risks for Mothers
- Exercise And Physical Activity Guidelines For Chronic Illness Management – Part 9
- Exercise And Physical Activity Guidelines For Chronic Illness Management – Part 10: Managing Rheumatoid Arthritis Through Exercise
- Integrating Mental Health Care In Chronic Disease Clinics – Part 10: Measuring Impact And Ensuring Sustainability
- Holistic Approaches To Chronic Disease Prevention – Part 7: Integrating Mind-Body Practices For Enhanced Well-being
- Clinical Trials In Leukemia Treatment: Patient Considerations
Introduction
On this special occasion, we are happy to review interesting topics related to Pregnancy and Heart Disease: Risks for Mothers. Come on knit interesting information and provide new insights to readers.
Pregnancy and Heart Disease: Risks for Mothers

For many women, pregnancy is a time of joy and anticipation. However, for those with pre-existing heart conditions or those who develop heart problems during pregnancy, it can present significant challenges. Heart disease is a leading cause of maternal mortality, making it crucial for women and their healthcare providers to understand the risks, potential complications, and management strategies associated with pregnancy and heart disease.
Prevalence and Types of Heart Disease in Pregnancy
Heart disease affects approximately 1-4% of pregnancies. The types of heart conditions encountered can vary, including:
-
Congenital Heart Disease: These are heart defects present at birth, such as septal defects, valve abnormalities, and complex structural issues. With advances in pediatric cardiology, more women with congenital heart disease are reaching childbearing age.
-
Valvular Heart Disease: Conditions like mitral stenosis, aortic stenosis, and valve regurgitation can strain the heart during pregnancy due to increased blood volume and cardiac output.
-
Cardiomyopathy: This involves weakening of the heart muscle, making it difficult for the heart to pump effectively. Peripartum cardiomyopathy (PPCM) is a specific type that develops during the late stages of pregnancy or in the months following delivery.
-
Arrhythmias: Irregular heart rhythms can occur or worsen during pregnancy, posing risks to both the mother and the fetus.
-
Ischemic Heart Disease: While less common in women of reproductive age, conditions like coronary artery disease can occur, especially in women with risk factors like high cholesterol, hypertension, or diabetes.
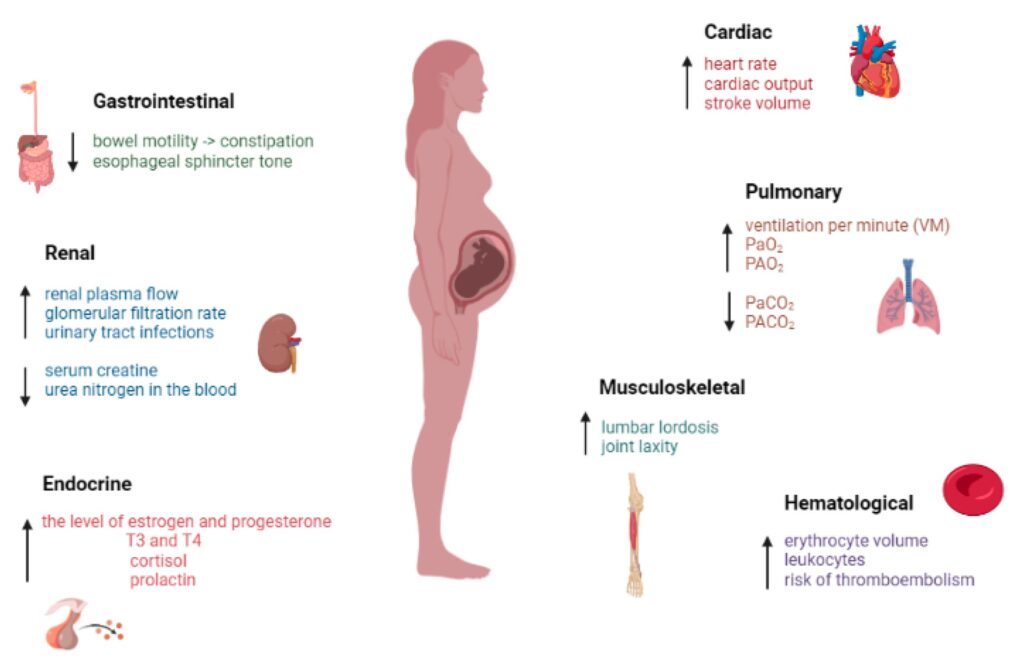
Physiological Changes of Pregnancy and Their Impact on the Heart
Pregnancy induces significant physiological changes that place extra demands on the cardiovascular system. These changes include:
-
Increased Blood Volume: Blood volume increases by 30-50% during pregnancy, starting early in the first trimester. This increase helps meet the metabolic demands of the growing fetus but also requires the heart to pump more blood with each beat.
-
Increased Cardiac Output: Cardiac output, the amount of blood pumped by the heart per minute, rises significantly, peaking in the mid-second trimester. This increase is due to both the increased blood volume and a higher heart rate.
-
Decreased Systemic Vascular Resistance: Blood vessels relax during pregnancy, leading to a decrease in systemic vascular resistance (SVR). This drop in SVR helps accommodate the increased blood volume and cardiac output, but it can also cause a drop in blood pressure, especially in early pregnancy.
-
Increased Heart Rate: Resting heart rate increases by 10-20 beats per minute during pregnancy, further contributing to the increased cardiac output.
-
Changes in Blood Coagulation: Pregnancy is a procoagulant state, meaning the blood is more likely to clot. This is a protective mechanism to prevent excessive bleeding during childbirth, but it also increases the risk of thromboembolism (blood clots).
For women with pre-existing heart disease, these physiological changes can exacerbate their condition, leading to heart failure, arrhythmias, stroke, or other complications.
Risks and Complications for Mothers with Heart Disease
Pregnancy in women with heart disease carries several risks and potential complications:
-
Heart Failure: The increased demands on the heart can lead to heart failure, where the heart is unable to pump enough blood to meet the body’s needs. Symptoms include shortness of breath, swelling in the legs and ankles, and fatigue.
-
Arrhythmias: Pregnancy can trigger or worsen arrhythmias, which can be dangerous for both the mother and the fetus. Some arrhythmias can lead to sudden cardiac arrest.
-
Stroke: The increased risk of blood clots during pregnancy can lead to stroke, which can cause permanent disability or death.
-
Pulmonary Hypertension: This condition involves high blood pressure in the arteries of the lungs, making it difficult for the heart to pump blood through the lungs. Pregnancy can worsen pulmonary hypertension, leading to severe complications.
-
Pre-eclampsia and Eclampsia: These pregnancy-specific conditions involve high blood pressure and protein in the urine. They can lead to seizures, stroke, and other complications, especially in women with pre-existing heart disease.
-
Maternal Mortality: Women with heart disease have a higher risk of dying during pregnancy or in the postpartum period compared to women without heart disease.
Risks and Complications for the Fetus
Maternal heart disease can also affect the fetus, leading to:
-
Premature Birth: Women with heart disease are more likely to deliver prematurely, which can lead to complications for the baby, such as respiratory distress syndrome, infections, and developmental delays.
-
Low Birth Weight: Babies born to mothers with heart disease may have lower birth weights, which can increase their risk of health problems.
-
Fetal Growth Restriction: The fetus may not grow properly in the womb due to inadequate blood flow and oxygen supply.
-
Congenital Heart Defects: There is a slightly increased risk of congenital heart defects in babies born to mothers with heart disease.
-
Fetal Death: In severe cases, maternal heart disease can lead to fetal death.
Management and Treatment Strategies
Managing pregnancy in women with heart disease requires a multidisciplinary approach involving cardiologists, obstetricians, maternal-fetal medicine specialists, and other healthcare professionals. Key strategies include:
-
Preconception Counseling: Women with heart disease should receive preconception counseling to assess the risks of pregnancy and discuss management options. This may involve optimizing medical therapy, addressing any structural heart problems, and discussing the risks and benefits of pregnancy.
-
Risk Stratification: Assessing the severity of the heart condition is crucial. The World Health Organization (WHO) classification is often used to categorize the risk associated with different heart conditions during pregnancy.
-
Medication Management: Some heart medications are safe to use during pregnancy, while others are not. Careful consideration must be given to the benefits and risks of each medication. Adjustments to medication dosages may be necessary.
-
Regular Monitoring: Frequent monitoring of the mother’s heart function and the baby’s growth and well-being is essential. This may involve echocardiograms, electrocardiograms (ECGs), and fetal ultrasounds.
-
Lifestyle Modifications: Lifestyle changes such as limiting sodium intake, maintaining a healthy weight, and avoiding smoking and alcohol can help manage heart disease during pregnancy.
-
Labor and Delivery Management: The mode of delivery (vaginal vs. cesarean) should be individualized based on the mother’s heart condition and obstetric factors. Continuous monitoring of the mother’s heart function during labor and delivery is crucial. Epidural anesthesia is often preferred for pain management, as it minimizes stress on the heart.
-
Postpartum Care: The postpartum period is a high-risk time for women with heart disease. Close monitoring is necessary to detect and manage any complications, such as heart failure or arrhythmias.
Prevention Strategies
Preventing heart disease in women of reproductive age is essential for reducing the risks associated with pregnancy. Strategies include:
-
Promoting Heart-Healthy Lifestyles: Encouraging women to adopt healthy lifestyles, including regular exercise, a balanced diet, and avoiding smoking, can help prevent heart disease.
-
Managing Risk Factors: Identifying and managing risk factors for heart disease, such as high blood pressure, high cholesterol, and diabetes, is crucial.
-
Early Detection and Treatment: Screening for heart disease in women with risk factors can help detect problems early and allow for timely treatment.
Conclusion
Pregnancy in women with heart disease presents significant challenges and risks for both the mother and the fetus. However, with careful management and a multidisciplinary approach, many women with heart disease can have successful pregnancies. Preconception counseling, risk stratification, regular monitoring, and individualized treatment plans are essential for optimizing outcomes. By understanding the risks and implementing appropriate management strategies, healthcare providers can help women with heart disease navigate pregnancy safely and achieve the joy of motherhood.







Leave a Reply