“Palliative Care and Quality of Life for Chronic Illness Patients – Part 5: Navigating Ethical Dilemmas and Future Directions
Related Articles Palliative Care and Quality of Life for Chronic Illness Patients – Part 5: Navigating Ethical Dilemmas and Future Directions
- Long-Term Effects Of Chronic Illness On Children
- Educational Interventions For Chronic Disease Prevention – Part 2: Advanced Strategies And Future Directions
- Technology’s Role In Chronic Disease Self-Management – Part 2
- Financial Challenges Of Living With Chronic Illness
- Nutritional Therapy For Chronic Disease Prevention – Part 3: Personalized Nutrition Plans And Implementation Strategies
Introduction
With great enthusiasm, let’s explore interesting topics related to Palliative Care and Quality of Life for Chronic Illness Patients – Part 5: Navigating Ethical Dilemmas and Future Directions. Let’s knit interesting information and provide new insights to readers.
Table of Content
Palliative Care and Quality of Life for Chronic Illness Patients – Part 5: Navigating Ethical Dilemmas and Future Directions
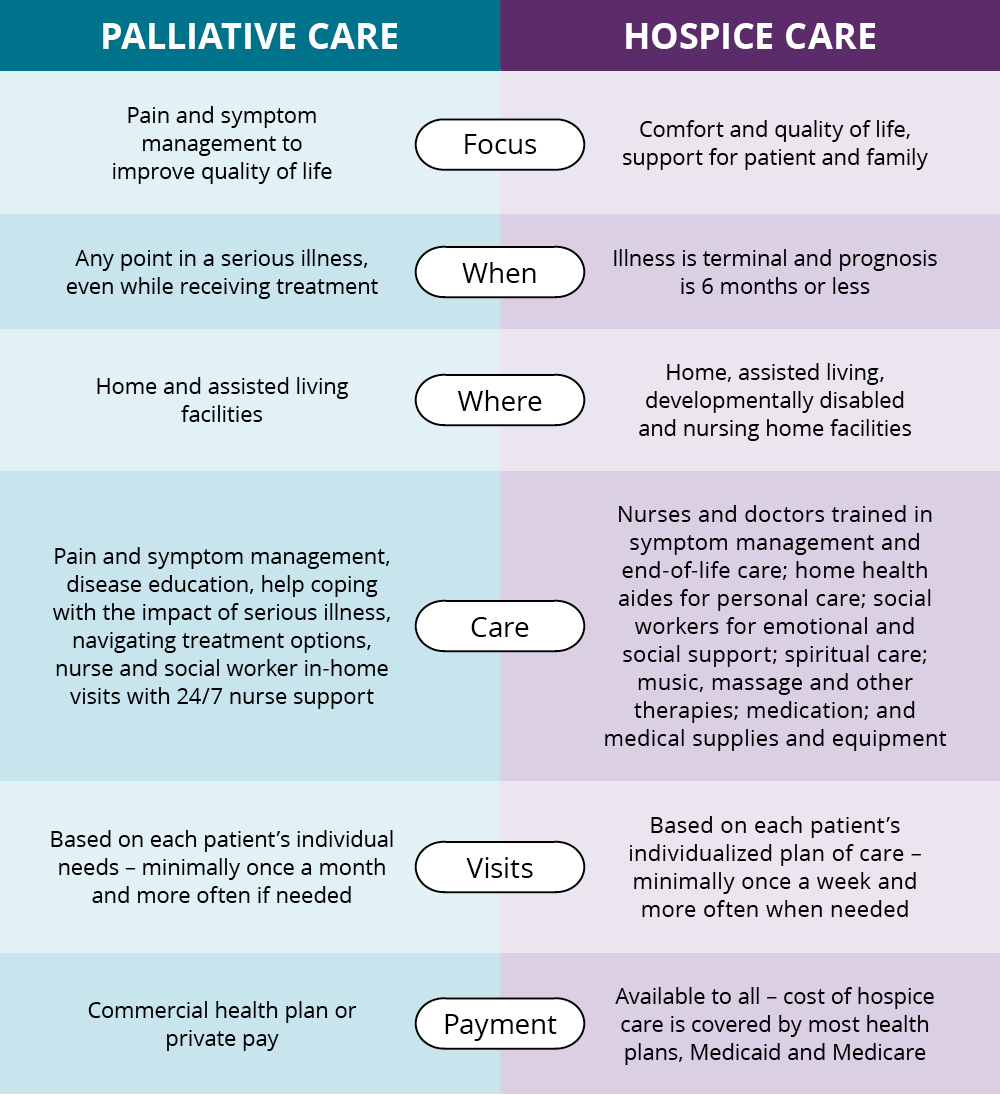
As the integration of palliative care into the management of chronic illnesses continues to expand, it is imperative to address the ethical dilemmas that frequently arise and to explore the future directions of this evolving field. This final part of our series delves into the complex ethical considerations encountered in palliative care and examines the innovative approaches and research needed to further enhance the quality of life for patients living with chronic conditions.
Ethical Dilemmas in Palliative Care
Palliative care, by its very nature, often involves navigating challenging ethical dilemmas. These dilemmas can arise from conflicting values, differing perspectives, and the complexities of end-of-life decision-making. Some of the most common ethical dilemmas in palliative care include:
-
Autonomy vs. Beneficence: Balancing the patient’s right to self-determination with the healthcare provider’s duty to act in the patient’s best interest can be challenging. This dilemma often arises when patients refuse treatments that healthcare providers believe are necessary or when patients request interventions that are not medically appropriate.
-
Truth-telling and Disclosure: Determining how much information to disclose to patients about their condition and prognosis can be ethically complex. While transparency is generally valued, healthcare providers must also consider the potential impact of information on the patient’s emotional well-being and ability to cope.
-
Withholding and Withdrawing Treatment: Decisions about withholding or withdrawing life-sustaining treatment are among the most difficult ethical dilemmas in palliative care. These decisions require careful consideration of the patient’s wishes, the potential benefits and burdens of treatment, and the ethical principles of non-maleficence and respect for autonomy.
-
Medical Aid in Dying: The debate surrounding medical aid in dying, also known as physician-assisted suicide, raises profound ethical questions about the role of healthcare providers in end-of-life care. While some argue that patients have a right to choose the timing and manner of their death, others believe that medical aid in dying violates the ethical principles of non-maleficence and the sanctity of life.
-
Resource Allocation: Limited resources can create ethical dilemmas in palliative care, particularly when making decisions about which patients receive access to specialized services or treatments. Healthcare providers must strive to allocate resources fairly and equitably while considering the unique needs and circumstances of each patient.
Strategies for Addressing Ethical Dilemmas
Navigating ethical dilemmas in palliative care requires a systematic and collaborative approach. Some strategies for addressing these dilemmas include:
-
Ethics Consultation: Ethics consultation services provide a forum for healthcare providers, patients, and families to discuss ethical concerns and explore potential solutions. Ethics consultants can help clarify ethical principles, facilitate communication, and promote shared decision-making.
-
Advance Care Planning: Advance care planning involves discussing and documenting a patient’s wishes regarding future medical care. This process can help ensure that the patient’s values and preferences are respected, even if they become unable to make decisions for themselves.
-
Interdisciplinary Collaboration: Ethical dilemmas often benefit from the perspectives of multiple disciplines, including physicians, nurses, social workers, chaplains, and ethicists. Interdisciplinary collaboration can help ensure that all relevant factors are considered and that decisions are made in the best interest of the patient.
-
Education and Training: Healthcare providers need ongoing education and training in ethical principles and decision-making. This education should include opportunities to discuss and analyze real-world case studies and to develop skills in communication, conflict resolution, and ethical reasoning.
-
Institutional Policies and Guidelines: Healthcare organizations should develop clear policies and guidelines for addressing common ethical dilemmas in palliative care. These policies should be based on ethical principles, legal requirements, and best practices.
Future Directions in Palliative Care
The field of palliative care is constantly evolving, with ongoing research and innovation aimed at improving the quality of life for patients living with chronic illnesses. Some of the key future directions in palliative care include:
-
Expanding Access to Palliative Care: Despite the growing recognition of the benefits of palliative care, access to these services remains limited for many patients, particularly those in underserved communities. Future efforts should focus on expanding access to palliative care through increased funding, workforce development, and innovative models of care delivery.
-
Integrating Palliative Care Earlier in the Disease Trajectory: Traditionally, palliative care has been offered primarily to patients in the late stages of their illness. However, research suggests that integrating palliative care earlier in the disease trajectory can improve outcomes and quality of life. Future models of care should focus on providing palliative care alongside disease-modifying treatments from the time of diagnosis.
-
Personalizing Palliative Care: Patients with chronic illnesses have diverse needs and preferences. Future palliative care approaches should be tailored to the individual patient’s unique circumstances, values, and goals. This may involve using advanced technologies, such as artificial intelligence, to personalize care plans and predict patient needs.
-
Leveraging Technology to Enhance Palliative Care: Technology has the potential to transform palliative care by improving communication, monitoring symptoms, and delivering remote support. Future research should explore the use of telehealth, mobile apps, and wearable devices to enhance palliative care services and improve patient outcomes.
-
Addressing Social Determinants of Health: Social determinants of health, such as poverty, food insecurity, and lack of access to transportation, can significantly impact the quality of life for patients with chronic illnesses. Future palliative care efforts should address these social determinants by connecting patients with community resources and advocating for policies that promote health equity.
-
Enhancing Palliative Care Education and Training: To meet the growing demand for palliative care services, it is essential to enhance education and training for healthcare professionals across all disciplines. This includes increasing the number of palliative care fellowship programs, integrating palliative care content into medical and nursing school curricula, and providing ongoing continuing education opportunities.
-
Promoting Research in Palliative Care: More research is needed to understand the effectiveness of different palliative care interventions, to identify best practices, and to develop new approaches to improve the quality of life for patients with chronic illnesses. Future research should focus on areas such as symptom management, psychosocial support, advance care planning, and end-of-life care.
Conclusion
Palliative care plays a vital role in improving the quality of life for patients living with chronic illnesses. By addressing physical, emotional, social, and spiritual needs, palliative care can help patients live as fully and comfortably as possible. As the field of palliative care continues to evolve, it is essential to address the ethical dilemmas that arise and to explore innovative approaches to enhance care delivery. By expanding access to palliative care, integrating it earlier in the disease trajectory, personalizing care, leveraging technology, addressing social determinants of health, enhancing education and training, and promoting research, we can ensure that all patients with chronic illnesses have access to the compassionate and comprehensive care they deserve.
References
- National Consensus Project for Quality Palliative Care. (2018). Clinical practice guidelines for quality palliative care (4th ed.). Richmond, VA: National Consensus Project.
- World Health Organization. (2020). Palliative care. Retrieved from https://www.who.int/news-room/fact-sheets/detail/palliative-care
- Meier, D. E., & Morrison, R. S. (2013). Palliative care. Annals of Internal Medicine, 158(2), ITC1-1-ITC1-16.
Semoga artikel ini bermanfaat. Beri tahu saya jika Anda ingin saya membuat perubahan atau penambahan apa pun.







Leave a Reply