“Osteogenesis Imperfecta: Causes and Treatment
Related Articles Osteogenesis Imperfecta: Causes and Treatment
- Bone Marrow: Functions And Importance In The Body
- Bone Health In Postmenopausal Women: Challenges And Solutions
- The Role Of Hormones In Bone Growth And Development
- Bone Development In Fetal And Neonatal Periods: A Comprehensive Overview
- The Role Of Nutrition In Supporting Bone Density
Introduction
We will be happy to explore interesting topics related to Osteogenesis Imperfecta: Causes and Treatment. Let’s knit interesting information and provide new insights to readers.
Osteogenesis Imperfecta: Causes and Treatment

Osteogenesis imperfecta (OI), also known as brittle bone disease, is a group of genetic disorders that primarily affect the bones. It is characterized by bones that break easily, often from little or no apparent cause. The severity of OI varies widely, ranging from mild cases with few fractures to severe cases with multiple fractures at birth and significant bone deformities. In addition to bone fragility, OI can also affect other parts of the body, including the teeth, eyes, ears, skin, and heart.
Causes of Osteogenesis Imperfecta
OI is caused by genetic mutations that affect the production of type I collagen, a protein that is essential for the formation of strong and healthy bones. Type I collagen is the most abundant protein in the body and is found in bones, skin, tendons, ligaments, and other connective tissues. Mutations in the genes that encode type I collagen can lead to a variety of problems, including:
- Reduced production of type I collagen
- Abnormal structure of type I collagen
- Increased breakdown of type I collagen
These problems can weaken the bones and make them more susceptible to fractures.
The vast majority of OI cases (around 90%) are caused by mutations in either the COL1A1 or COL1A2 genes. These genes provide instructions for making the alpha-1 and alpha-2 chains of type I collagen, respectively. Mutations in these genes can lead to a variety of OI types, with varying degrees of severity.
In rarer cases, OI can be caused by mutations in other genes that are involved in collagen production or bone development. These genes include BMP1, CRTAP, FKBP10, LEPRE1, PLOD2, PPIB, SERPINH1, and WNT1. Mutations in these genes typically result in more severe forms of OI.
OI is usually inherited in an autosomal dominant pattern, which means that only one copy of the mutated gene is needed to cause the disorder. In these cases, an affected individual typically inherits the mutated gene from one parent who also has OI. However, OI can also occur as a result of a new (de novo) mutation in the COL1A1 or COL1A2 gene. In these cases, the affected individual is the first in their family to have OI.
Autosomal recessive inheritance is less common in OI. In this pattern, two copies of the mutated gene (one from each parent) are needed to cause the disorder. Parents of a child with autosomal recessive OI are typically carriers of the mutated gene, meaning they have one copy of the mutated gene but do not have OI themselves.
Types of Osteogenesis Imperfecta
OI is classified into several types, based on the severity of the symptoms and the underlying genetic mutation. The most common types of OI are:
- Type I: This is the mildest form of OI. People with type I OI typically have bones that break easily, but they may not have any other significant symptoms. They may also have blue sclerae (the whites of the eyes), hearing loss, and dental problems.
- Type II: This is the most severe form of OI. Babies with type II OI are often born with multiple fractures and significant bone deformities. They may also have respiratory problems and other life-threatening complications. Most babies with type II OI do not survive infancy.
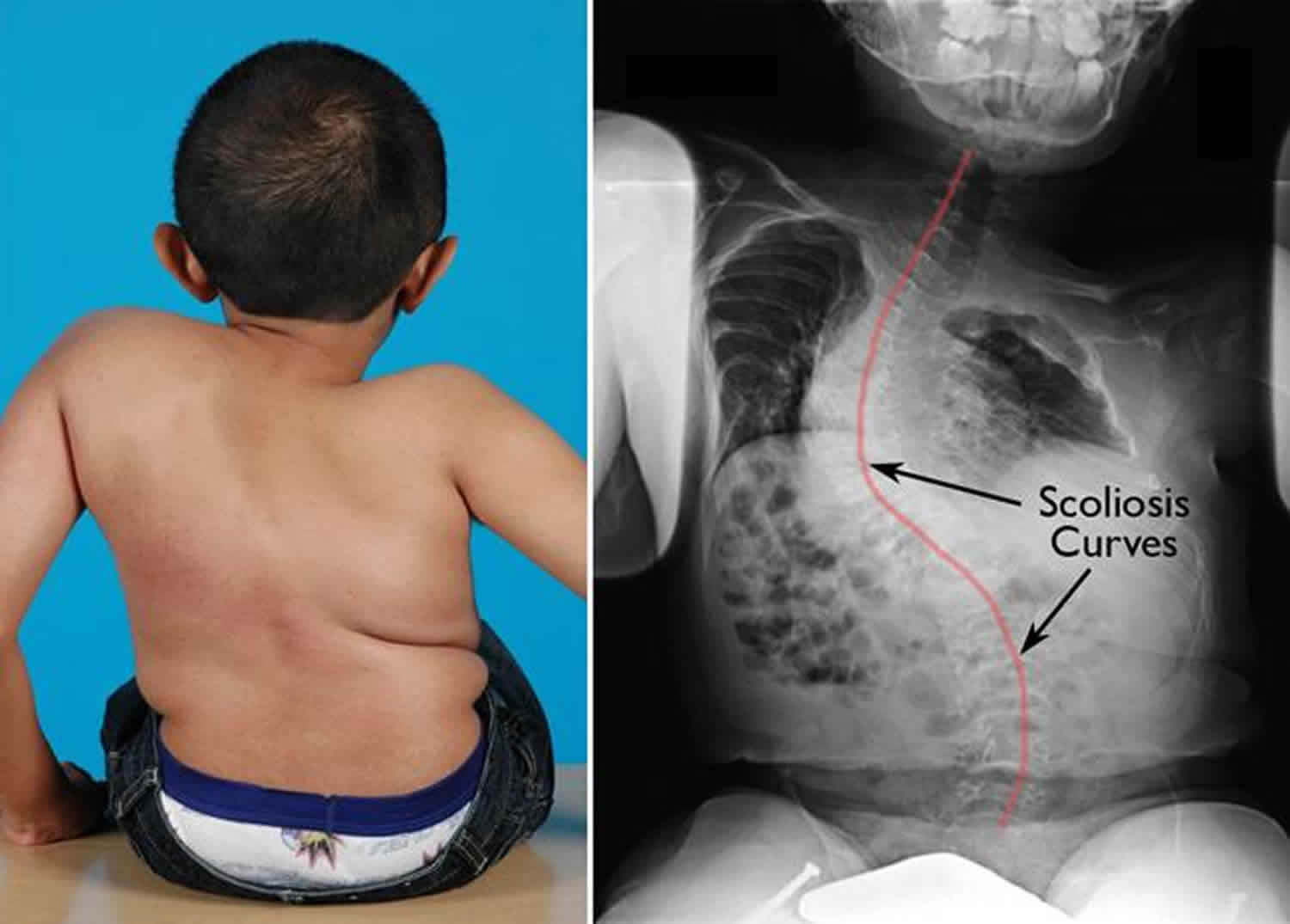
- Type III: People with type III OI have bones that break easily and are often deformed. They may also have short stature, scoliosis (curvature of the spine), and respiratory problems. The severity of type III OI varies widely.
- Type IV: People with type IV OI have bones that break easily, but they may not have any other significant symptoms. They may also have short stature, scoliosis, and dental problems. The severity of type IV OI varies widely.
- Type V: This type is characterized by the formation of hypertrophic callus (excessive bone growth) at fracture sites. People with type V OI may also have calcification of the interosseous membrane between the radius and ulna in the forearm, which can limit forearm rotation.
- Type VI: This type is characterized by a "fish-scale" appearance of bone under a microscope. The cause of type VI OI is not fully understood, but it is thought to be related to problems with bone mineralization.
- Type VII-XIX: These are rarer types of OI that are caused by mutations in genes other than COL1A1 and COL1A2. The symptoms of these types of OI vary depending on the underlying genetic mutation.
Diagnosis of Osteogenesis Imperfecta
OI can be diagnosed based on a physical exam, X-rays, and genetic testing.
- Physical exam: A doctor may suspect OI if a person has a history of frequent fractures, especially if the fractures occur with little or no apparent cause. Other signs of OI that can be detected during a physical exam include blue sclerae, short stature, scoliosis, and dental problems.
- X-rays: X-rays can be used to detect fractures and bone deformities. In some cases, X-rays can also reveal characteristic features of OI, such as thin bones and multiple healed fractures.
- Genetic testing: Genetic testing can be used to confirm the diagnosis of OI and to identify the specific genetic mutation that is causing the disorder. This information can be helpful in determining the severity of OI and in predicting the risk of future fractures. Genetic testing can be performed on a blood sample or a skin biopsy.
Prenatal testing for OI is available for families who have a history of the disorder. This testing can be performed using chorionic villus sampling (CVS) or amniocentesis.
Treatment of Osteogenesis Imperfecta
There is no cure for OI, but there are treatments that can help to reduce the number of fractures, improve bone strength, and manage other symptoms. Treatment for OI typically involves a combination of:
- Medications: Bisphosphonates are medications that can help to increase bone density and reduce the risk of fractures. Bisphosphonates are typically administered intravenously (through a vein) or orally (by mouth). Other medications that may be used to treat OI include vitamin D, calcium, and growth hormone.
- Physical therapy: Physical therapy can help to improve muscle strength, balance, and coordination. This can help to reduce the risk of falls and fractures. Physical therapy can also help to maintain or improve range of motion in the joints.
- Occupational therapy: Occupational therapy can help people with OI to learn how to perform daily activities in a safe and efficient manner. Occupational therapists can also recommend assistive devices, such as braces, walkers, and wheelchairs, to help people with OI to maintain their independence.
- Surgery: Surgery may be necessary to correct bone deformities, stabilize fractures, or relieve pressure on nerves. Common surgical procedures for people with OI include rodding (insertion of metal rods into the long bones to provide support), osteotomy (cutting and reshaping of bone), and spinal fusion (joining together two or more vertebrae to stabilize the spine).
- Fracture Care: Fractures are a common occurrence in people with OI. Proper fracture care is essential to ensure that the bones heal properly and to prevent further complications. Fracture care may involve casting, splinting, or surgery.
- Dental care: People with OI are at increased risk of dental problems, such as tooth decay and enamel defects. Regular dental care is essential to maintain good oral health.
- Hearing care: Hearing loss is a common complication of OI. People with OI should have their hearing checked regularly. Hearing aids or other assistive devices may be necessary to improve hearing.
- Psychological support: Living with OI can be challenging. Psychological support can help people with OI to cope with the emotional and social challenges of the disorder. Support groups can also provide a valuable source of information and support.
The specific treatment plan for OI will vary depending on the type and severity of the disorder, as well as the individual’s age and overall health.
Prognosis of Osteogenesis Imperfecta
The prognosis for people with OI varies depending on the type and severity of the disorder. People with mild OI may have a normal lifespan and be able to live relatively normal lives. People with severe OI may have a shortened lifespan and experience significant disability.
With proper treatment and care, people with OI can live longer, healthier, and more fulfilling lives. Early diagnosis and intervention are essential to optimize outcomes.
Living with Osteogenesis Imperfecta
Living with OI can be challenging, but there are many things that people with OI can do to improve their quality of life. These include:
- Maintaining a healthy lifestyle: Eating a healthy diet, getting regular exercise, and avoiding smoking can help to improve bone health and overall health.
- Taking precautions to prevent fractures: This includes avoiding activities that are likely to cause falls, using assistive devices, and modifying the home environment to make it safer.
- Seeking support from others: Connecting with other people with OI can provide a valuable source of information and support.
- Advocating for themselves: People with OI need to be their own advocates to ensure that they receive the best possible care and support.
OI is a complex disorder that can have a significant impact on a person’s life. However, with proper treatment and support, people with OI can live full and meaningful lives.







Leave a Reply