“Mental Health Interventions for Chronic Disease Patients – Part 2: Targeted Approaches and Emerging Strategies
Related Articles Mental Health Interventions for Chronic Disease Patients – Part 2: Targeted Approaches and Emerging Strategies
- Long-term Effects Of Chronic Illness On Children – Part 2
- Disability Rights And Advocacy For Chronic Disease Patients – Part 2
- The Impact Of Chronic Illness On Mental Health
- Educational Interventions For Chronic Disease Prevention – Part 2: Advanced Strategies And Future Directions
- Public Policy And Chronic Disease Prevention Strategies – Part 2
Introduction
We will be happy to explore interesting topics related to Mental Health Interventions for Chronic Disease Patients – Part 2: Targeted Approaches and Emerging Strategies. Come on knit interesting information and provide new insights to readers.
Table of Content
Mental Health Interventions for Chronic Disease Patients – Part 2: Targeted Approaches and Emerging Strategies
Introduction
Chronic diseases are a significant global health challenge, impacting millions of lives and placing a substantial burden on healthcare systems. While the physical aspects of these conditions are often the primary focus of treatment, the profound impact on mental health cannot be overlooked. Individuals living with chronic diseases such as diabetes, heart disease, cancer, and arthritis are at a significantly higher risk of developing mental health disorders like depression, anxiety, and stress-related conditions.
In Part 1 of this series, we explored the bidirectional relationship between chronic diseases and mental health, emphasizing the importance of integrated care approaches. We examined the prevalence of mental health issues among individuals with chronic conditions and highlighted the benefits of addressing both physical and psychological well-being.
In this second part, we will delve deeper into specific mental health interventions tailored to the unique needs of chronic disease patients. We will explore evidence-based therapies, lifestyle modifications, and emerging strategies that can improve mental health outcomes and overall quality of life.
Targeted Mental Health Interventions
The effectiveness of mental health interventions is greatly enhanced when they are tailored to the specific needs and challenges faced by individuals with chronic diseases. Here are some targeted approaches:
-
Cognitive Behavioral Therapy (CBT):
- Description: CBT is a widely used and highly effective psychotherapy approach that focuses on identifying and modifying negative thought patterns and behaviors that contribute to emotional distress. It is based on the principle that our thoughts, feelings, and behaviors are interconnected, and by changing maladaptive thoughts, we can improve our emotional well-being.
- Application in Chronic Disease: CBT is particularly useful for individuals with chronic diseases who experience depression, anxiety, or chronic pain. It helps patients develop coping strategies to manage symptoms, reduce negative thinking, and improve their ability to engage in self-care activities. For example, in patients with diabetes, CBT can address negative thoughts about managing their condition, improve adherence to medication regimens, and promote healthy lifestyle choices.
- Evidence: Numerous studies have demonstrated the efficacy of CBT in improving mental health outcomes in chronic disease populations. A meta-analysis of studies on CBT for depression in individuals with chronic physical illnesses found that CBT significantly reduced depressive symptoms compared to usual care.
-
Mindfulness-Based Interventions:
- Description: Mindfulness-based interventions involve training individuals to cultivate present moment awareness and acceptance of their thoughts and feelings without judgment. These interventions often incorporate practices such as meditation, body scan exercises, and mindful movement.
- Application in Chronic Disease: Mindfulness-based interventions have shown promise in reducing stress, anxiety, and pain in individuals with chronic diseases. By focusing on the present moment, patients can learn to detach from negative thoughts and emotions, improve their ability to cope with physical symptoms, and enhance their overall sense of well-being. For example, mindfulness-based stress reduction (MBSR) programs have been found to be effective in reducing anxiety and improving quality of life in patients with cancer.
- Evidence: Research has shown that mindfulness-based interventions can lead to significant improvements in mental health outcomes in chronic disease populations. A systematic review of studies on mindfulness-based interventions for chronic pain found that these interventions were associated with significant reductions in pain intensity and improvements in psychological functioning.
-
Acceptance and Commitment Therapy (ACT):
- Description: ACT is a form of psychotherapy that encourages individuals to accept their thoughts and feelings without judgment and to commit to actions that are consistent with their values. It emphasizes psychological flexibility, which is the ability to adapt to changing circumstances and to pursue meaningful goals despite the presence of difficult emotions or thoughts.
- Application in Chronic Disease: ACT is particularly useful for individuals with chronic diseases who experience significant distress related to their condition. It helps patients accept their physical limitations and emotional challenges, focus on what they can control, and engage in activities that are important to them. For example, in patients with chronic fatigue syndrome, ACT can help them accept their fatigue and focus on activities that give them a sense of purpose and meaning.
- Evidence: Studies have shown that ACT can be effective in improving mental health outcomes in chronic disease populations. A randomized controlled trial of ACT for individuals with chronic pain found that ACT was associated with significant reductions in pain interference and improvements in psychological functioning.
-
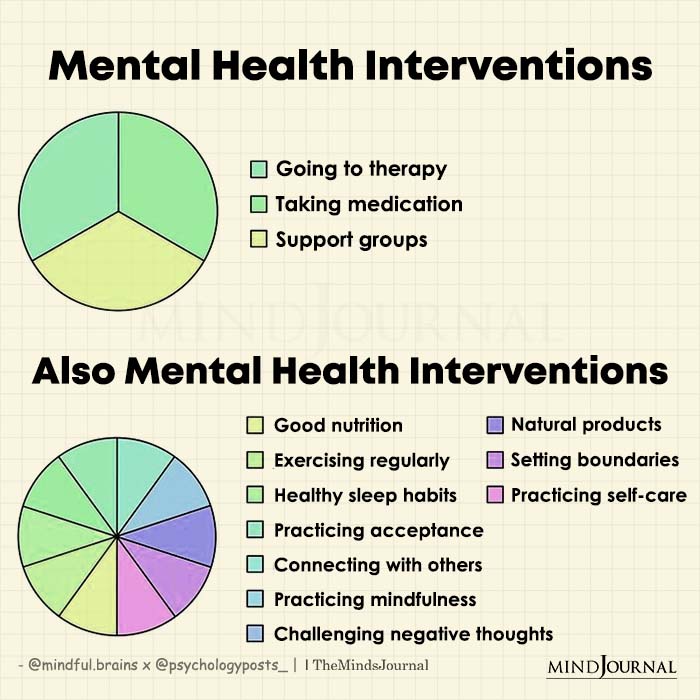
Support Groups and Peer Support:
- Description: Support groups and peer support programs provide individuals with chronic diseases the opportunity to connect with others who share similar experiences. These groups offer a safe and supportive environment for individuals to share their feelings, learn coping strategies, and receive encouragement from their peers.
- Application in Chronic Disease: Support groups and peer support programs can be particularly beneficial for individuals who feel isolated or stigmatized due to their chronic condition. They provide a sense of community and belonging, reduce feelings of loneliness, and offer practical advice and emotional support. For example, cancer support groups can help patients cope with the emotional challenges of diagnosis, treatment, and survivorship.
- Evidence: Research has shown that support groups and peer support programs can improve mental health outcomes in chronic disease populations. A meta-analysis of studies on support groups for individuals with cancer found that these groups were associated with significant reductions in anxiety and depression.
-
Lifestyle Modifications:
- Description: Lifestyle modifications, such as regular exercise, a healthy diet, and sufficient sleep, can have a profound impact on both physical and mental health. These modifications can improve mood, reduce stress, and enhance overall well-being.
- Application in Chronic Disease: Lifestyle modifications are an integral part of managing chronic diseases and can also play a significant role in improving mental health. For example, regular exercise has been shown to reduce symptoms of depression and anxiety in individuals with heart disease. A healthy diet can improve mood and energy levels in patients with diabetes.
- Evidence: Numerous studies have demonstrated the benefits of lifestyle modifications for both physical and mental health in chronic disease populations. A systematic review of studies on exercise for depression found that exercise was as effective as antidepressant medication in reducing depressive symptoms.
Emerging Strategies
In addition to the established interventions discussed above, several emerging strategies are showing promise in improving mental health outcomes in chronic disease patients:
-
Technology-Based Interventions:
- Description: Technology-based interventions, such as mobile apps, online support groups, and telehealth services, are becoming increasingly popular for delivering mental health care. These interventions offer convenience, accessibility, and affordability, making them particularly appealing to individuals with chronic diseases who may face barriers to traditional in-person care.
- Application in Chronic Disease: Technology-based interventions can be used to deliver a wide range of mental health services, including CBT, mindfulness training, and peer support. They can also be used to monitor symptoms, track progress, and provide personalized feedback. For example, mobile apps can help patients with diabetes manage their blood sugar levels, track their medication adherence, and receive reminders to engage in healthy behaviors.
- Evidence: Research on technology-based interventions for mental health in chronic disease populations is growing. A systematic review of studies on mobile apps for depression found that these apps were associated with significant reductions in depressive symptoms.
-
Integrated Care Models:
- Description: Integrated care models involve the coordination of physical and mental health care services within a single setting. These models aim to provide comprehensive, patient-centered care that addresses the interconnectedness of physical and mental health.
- Application in Chronic Disease: Integrated care models can improve access to mental health services for individuals with chronic diseases by reducing stigma, improving communication between providers, and streamlining the referral process. For example, a primary care clinic that integrates mental health services can provide on-site counseling and medication management for patients with depression or anxiety.
- Evidence: Studies have shown that integrated care models can improve both physical and mental health outcomes in chronic disease populations. A randomized controlled trial of an integrated care model for depression in individuals with diabetes found that the integrated care model was associated with significant reductions in depressive symptoms and improvements in glycemic control.
-
Personalized Medicine Approaches:
- Description: Personalized medicine approaches involve tailoring treatment to the individual characteristics of each patient, including their genetic makeup, lifestyle, and preferences. These approaches aim to maximize treatment effectiveness and minimize side effects.
- Application in Chronic Disease: Personalized medicine approaches can be used to identify individuals with chronic diseases who are at high risk of developing mental health disorders and to tailor interventions to their specific needs. For example, genetic testing can identify individuals who are more likely to respond to certain antidepressant medications.
- Evidence: Research on personalized medicine approaches for mental health in chronic disease populations is still in its early stages, but there is growing evidence that these approaches can improve treatment outcomes.
Conclusion
Mental health interventions are an essential component of comprehensive care for individuals with chronic diseases. Targeted approaches such as CBT, mindfulness-based interventions, ACT, support groups, and lifestyle modifications can significantly improve mental health outcomes and overall quality of life. Emerging strategies like technology-based interventions, integrated care models, and personalized medicine approaches hold promise for further enhancing mental health care for this vulnerable population.
By prioritizing mental health alongside physical health, we can empower individuals with chronic diseases to live fuller, more meaningful lives. It is crucial for healthcare providers, policymakers, and researchers to continue to invest in and promote these interventions to ensure that all individuals with chronic diseases have access to the mental health support they need.








Leave a Reply