“Leukemia and Metabolic Syndrome: Exploring the Links
Related Articles Leukemia and Metabolic Syndrome: Exploring the Links
- The Role Of Stress In Chronic Disease Progression – Part 5: Integrative Approaches To Stress Management For Chronic Disease Patients
- Mental Health Interventions For Chronic Disease Patients – Part 6
- The Role Of Stress In Chronic Disease Progression – Part 6
- Social Support Networks For Chronic Disease Patients – Part 4: Leveraging Technology And Future Directions
- Integrative Care Models For Complex Chronic Diseases – Part 7: The Role Of Technology In Enhancing Integrative Care Delivery
Introduction
On this special occasion, we are happy to review interesting topics related to Leukemia and Metabolic Syndrome: Exploring the Links. Come on knit interesting information and provide new insights to readers.
Table of Content
Leukemia and Metabolic Syndrome: Exploring the Links
Introduction
Leukemia, a malignant disorder of the blood and bone marrow, is characterized by the abnormal proliferation of leukocytes, which disrupts the production of normal blood cells. While genetic mutations and exposure to certain environmental factors are well-established risk factors for leukemia, emerging evidence suggests a potential link between metabolic syndrome (MetS) and the development and progression of this hematological malignancy.
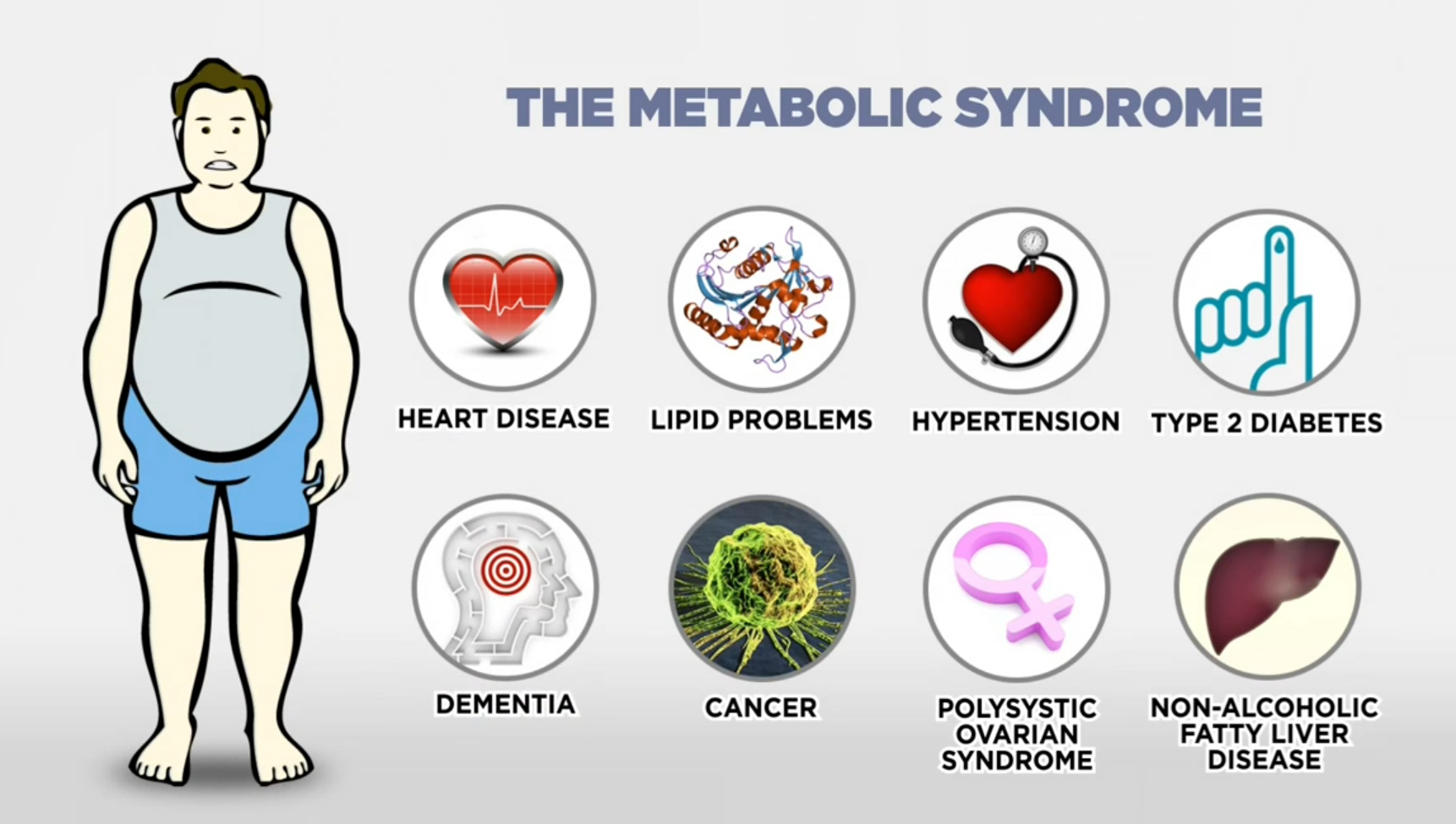
Metabolic syndrome, a cluster of interrelated metabolic abnormalities, including abdominal obesity, insulin resistance, hypertension, and dyslipidemia, has become a global health concern due to its increasing prevalence and association with various chronic diseases, such as cardiovascular disease, type 2 diabetes, and certain cancers. The interplay between leukemia and metabolic syndrome is complex and multifaceted, involving shared pathophysiological mechanisms and potential bidirectional relationships.
This article aims to explore the current understanding of the links between leukemia and metabolic syndrome, examining the epidemiological evidence, underlying mechanisms, and clinical implications. By elucidating the potential connections between these two conditions, we can gain insights into novel strategies for prevention, early detection, and improved management of leukemia patients with metabolic syndrome.
Epidemiological Evidence
Several epidemiological studies have investigated the association between metabolic syndrome and the risk of developing leukemia. While the evidence is not entirely consistent, some studies have reported a positive correlation between MetS and increased leukemia risk, particularly for certain subtypes.
A meta-analysis of observational studies published in Blood Cancer Journal found that individuals with metabolic syndrome had a significantly higher risk of developing leukemia compared to those without MetS. The pooled relative risk (RR) was 1.32 (95% confidence interval [CI]: 1.15-1.52), indicating a 32% increased risk of leukemia among individuals with metabolic syndrome. Subgroup analyses revealed that the association was more pronounced for acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
A cohort study conducted in Sweden, involving over 300,000 individuals, reported that metabolic syndrome was associated with an increased risk of AML. The hazard ratio (HR) for AML was 1.45 (95% CI: 1.12-1.87) for individuals with metabolic syndrome compared to those without MetS. The study also found that each component of metabolic syndrome, including obesity, hypertension, and dyslipidemia, was independently associated with an increased risk of AML.
However, other studies have not found a significant association between metabolic syndrome and leukemia risk. A large prospective study conducted in the United States, involving over 1.2 million participants, found no significant association between metabolic syndrome and overall leukemia risk. The study did find a modest association between MetS and increased risk of acute promyelocytic leukemia (APL), a subtype of AML.
The conflicting findings in epidemiological studies may be attributed to several factors, including differences in study design, population characteristics, diagnostic criteria for metabolic syndrome and leukemia, and statistical power. Further large-scale prospective studies are needed to clarify the association between metabolic syndrome and leukemia risk, considering specific leukemia subtypes and potential confounding factors.
Underlying Mechanisms
The potential mechanisms underlying the link between metabolic syndrome and leukemia are complex and multifactorial, involving shared pathophysiological pathways and potential bidirectional relationships. Several mechanisms have been proposed, including:
- Chronic Inflammation: Metabolic syndrome is characterized by chronic low-grade inflammation, which is mediated by the activation of inflammatory signaling pathways and the production of pro-inflammatory cytokines, such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP). Chronic inflammation can promote the development and progression of leukemia by creating a microenvironment that supports the survival, proliferation, and drug resistance of leukemic cells.
- Insulin Resistance and Hyperinsulinemia: Insulin resistance, a hallmark of metabolic syndrome, leads to compensatory hyperinsulinemia, which can stimulate the growth and proliferation of leukemic cells. Insulin and insulin-like growth factor-1 (IGF-1) receptors are often overexpressed in leukemic cells, and activation of these receptors can promote cell survival, proliferation, and angiogenesis.
- Adipokines: Adipose tissue, which is expanded in metabolic syndrome, secretes a variety of adipokines, such as leptin, adiponectin, and resistin, which can influence the development and progression of leukemia. Leptin, which is elevated in obesity, can promote the proliferation and survival of leukemic cells, while adiponectin, which is decreased in obesity, has anti-inflammatory and anti-proliferative effects.
- Oxidative Stress: Metabolic syndrome is associated with increased oxidative stress, which is caused by an imbalance between the production of reactive oxygen species (ROS) and the antioxidant defense mechanisms. Oxidative stress can damage DNA, proteins, and lipids, leading to genomic instability and increased risk of mutations, which can contribute to the development of leukemia.
- Gut Microbiota Dysbiosis: Metabolic syndrome is often accompanied by gut microbiota dysbiosis, which is characterized by alterations in the composition and function of the gut microbial community. Gut microbiota dysbiosis can promote chronic inflammation, insulin resistance, and oxidative stress, which can contribute to the development and progression of leukemia.
- Epigenetic Modifications: Metabolic syndrome can induce epigenetic modifications, such as DNA methylation and histone modifications, which can alter gene expression and contribute to the development and progression of leukemia. Epigenetic modifications can affect the expression of genes involved in cell proliferation, differentiation, and apoptosis, leading to the malignant transformation of hematopoietic cells.
Clinical Implications
The potential link between metabolic syndrome and leukemia has several clinical implications for the prevention, early detection, and management of leukemia patients with metabolic syndrome.
- Prevention: Lifestyle modifications, such as weight loss, regular exercise, and a healthy diet, can prevent or reverse metabolic syndrome and potentially reduce the risk of developing leukemia. Public health interventions aimed at promoting healthy lifestyles and preventing metabolic syndrome may have a beneficial impact on leukemia incidence.
- Early Detection: Screening for metabolic syndrome in individuals at high risk of leukemia, such as those with a family history of leukemia or exposure to certain environmental factors, may facilitate early detection and intervention. Early diagnosis and treatment of leukemia can improve outcomes and survival rates.
- Treatment Strategies: Leukemia patients with metabolic syndrome may require modified treatment strategies to address the metabolic abnormalities and improve treatment outcomes. For example, metformin, a commonly used drug for type 2 diabetes, has been shown to have anti-leukemic effects in preclinical studies and may be a useful adjunct therapy for leukemia patients with insulin resistance.
- Supportive Care: Metabolic syndrome can exacerbate the side effects of leukemia treatment, such as chemotherapy-induced nausea, fatigue, and infections. Supportive care measures, such as nutritional support, exercise programs, and psychological counseling, can help improve the quality of life and tolerance to treatment in leukemia patients with metabolic syndrome.
- Monitoring and Follow-up: Leukemia patients with metabolic syndrome should be closely monitored for the development of cardiovascular disease, type 2 diabetes, and other complications associated with metabolic syndrome. Regular follow-up visits and appropriate medical management can help prevent or mitigate these complications and improve overall health outcomes.
Future Directions
Further research is needed to fully elucidate the complex interplay between metabolic syndrome and leukemia. Future studies should focus on:
- Investigating the specific mechanisms by which metabolic syndrome contributes to the development and progression of different leukemia subtypes.
- Conducting large-scale prospective studies to confirm the association between metabolic syndrome and leukemia risk, considering potential confounding factors and effect modifiers.
- Evaluating the impact of lifestyle interventions and pharmacological treatments for metabolic syndrome on leukemia outcomes.
- Developing personalized treatment strategies for leukemia patients with metabolic syndrome, based on their individual metabolic profiles and disease characteristics.
- Exploring the role of gut microbiota in the pathogenesis of leukemia and metabolic syndrome, and developing targeted interventions to modulate the gut microbiota and improve outcomes.
Conclusion
Emerging evidence suggests a potential link between metabolic syndrome and leukemia, with some studies reporting a positive association between MetS and increased leukemia risk, particularly for certain subtypes. The underlying mechanisms are complex and multifactorial, involving shared pathophysiological pathways, such as chronic inflammation, insulin resistance, adipokine dysregulation, oxidative stress, gut microbiota dysbiosis, and epigenetic modifications.
The potential link between metabolic syndrome and leukemia has several clinical implications for the prevention, early detection, and management of leukemia patients with metabolic syndrome. Lifestyle modifications, early screening, modified treatment strategies, supportive care, and close monitoring may improve outcomes and quality of life in leukemia patients with metabolic syndrome.
Further research is needed to fully elucidate the complex interplay between metabolic syndrome and leukemia and to develop targeted interventions to prevent and manage these conditions. By addressing the metabolic abnormalities associated with metabolic syndrome, we may be able to reduce the risk of developing leukemia and improve the outcomes of leukemia patients with metabolic syndrome.








Leave a Reply