“Leukemia and Inflammatory Responses: Pathophysiological Insights
Related Articles Leukemia and Inflammatory Responses: Pathophysiological Insights
- Long-Term Effects Of Chronic Illness On Children
- Nutritional Therapy For Chronic Disease Prevention – Part 10
- Public Health Initiatives To Combat Chronic Illnesses – Part 8: Leveraging Technology And Innovation For Prevention And Management
- Ketahanan Psikologis Pada Pasien Penyakit Kronis – Bagian 6
- Chronic Disease Management In Low-Income Communities – Part 9: Scaling Up Successful Interventions: Policy, Partnerships, And Sustainability
Introduction
On this special occasion, we are happy to review interesting topics related to Leukemia and Inflammatory Responses: Pathophysiological Insights. Come on knit interesting information and provide new insights to readers.
Table of Content
Leukemia and Inflammatory Responses: Pathophysiological Insights
Abstract
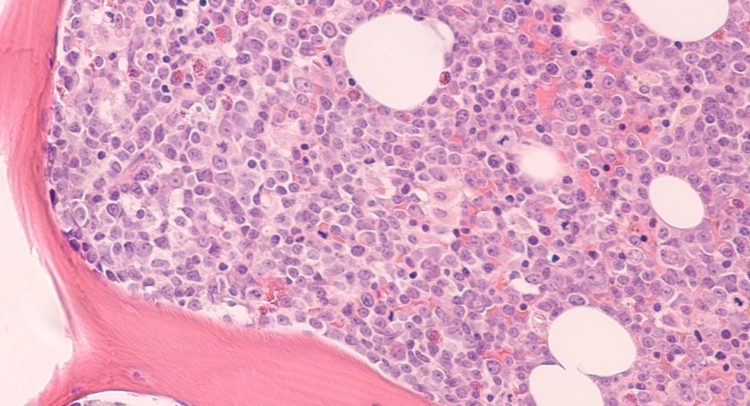
Leukemia, a hematological malignancy characterized by the uncontrolled proliferation of abnormal blood cells, is increasingly recognized for its intricate relationship with inflammatory responses. This article delves into the pathophysiological interplay between leukemia and inflammation, exploring how inflammatory mediators influence disease progression, treatment outcomes, and the development of complications. We examine the roles of various inflammatory pathways, cytokines, and immune cells in the context of different leukemia subtypes, highlighting the potential for targeted therapies that modulate inflammatory responses to improve patient outcomes.
Introduction
Leukemia encompasses a diverse group of cancers affecting the blood and bone marrow, leading to the overproduction of dysfunctional leukocytes. While the genetic and molecular underpinnings of leukemia have been extensively studied, the role of inflammation in its pathogenesis and progression has gained significant attention in recent years. Inflammation, a complex biological response to harmful stimuli, is orchestrated by a network of immune cells, signaling molecules, and inflammatory mediators. In the context of leukemia, inflammation can be both a consequence of the disease and a driver of its progression.
The inflammatory milieu in leukemia is characterized by elevated levels of pro-inflammatory cytokines, such as interleukin-1 (IL-1), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and chemokines. These mediators not only contribute to systemic symptoms like fever, fatigue, and weight loss but also influence the behavior of leukemic cells, promoting their survival, proliferation, and resistance to therapy. Furthermore, inflammation can disrupt normal hematopoiesis, leading to cytopenias and increased susceptibility to infections.
Inflammatory Pathways in Leukemia
Several key inflammatory pathways are implicated in the pathogenesis of leukemia:
-
NF-κB Signaling: The nuclear factor-kappa B (NF-κB) pathway is a central regulator of inflammation and immunity. In leukemia, NF-κB is often constitutively activated, promoting the expression of genes involved in cell survival, proliferation, and angiogenesis. Activation of NF-κB can be triggered by various stimuli, including inflammatory cytokines, toll-like receptor (TLR) ligands, and genetic mutations.
-
JAK-STAT Signaling: The Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway is involved in cytokine signaling and hematopoiesis. Dysregulation of JAK-STAT signaling is frequently observed in leukemia, leading to abnormal proliferation and survival of leukemic cells. Certain leukemia subtypes, such as myeloproliferative neoplasms (MPNs), harbor activating mutations in JAK kinases, driving constitutive activation of the pathway.
-
inflammasome Activation: Inflammasomes are multiprotein complexes that activate caspase-1, leading to the maturation and release of pro-inflammatory cytokines like IL-1β and IL-18. Activation of inflammasomes in leukemia can contribute to systemic inflammation, disease progression, and the development of complications like cytokine release syndrome (CRS).
-
TLR Signaling: Toll-like receptors (TLRs) are pattern recognition receptors that recognize pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). Activation of TLRs in leukemia can stimulate the production of inflammatory cytokines and chemokines, contributing to disease progression and immune dysregulation.
Role of Cytokines in Leukemia
Cytokines play a crucial role in mediating the inflammatory response in leukemia. Some of the key cytokines involved include:
-
IL-1: IL-1 is a potent pro-inflammatory cytokine that promotes the production of other cytokines, such as IL-6 and TNF-α. In leukemia, IL-1 can stimulate the proliferation and survival of leukemic cells, as well as contribute to systemic symptoms like fever and fatigue.
-
IL-6: IL-6 is a pleiotropic cytokine that plays a role in inflammation, immunity, and hematopoiesis. Elevated levels of IL-6 are often observed in leukemia, and IL-6 can promote the proliferation, survival, and drug resistance of leukemic cells.
-
TNF-α: TNF-α is a pro-inflammatory cytokine that can induce apoptosis, promote inflammation, and stimulate the production of other cytokines. In leukemia, TNF-α can contribute to systemic symptoms like cachexia and fatigue, as well as promote the survival and proliferation of leukemic cells.
-
Chemokines: Chemokines are a family of chemoattractant cytokines that regulate the migration of immune cells. In leukemia, chemokines can promote the recruitment of inflammatory cells to the bone marrow and other tissues, contributing to disease progression and immune dysregulation.
Immune Cell Involvement in Leukemia-Associated Inflammation
Several types of immune cells contribute to the inflammatory response in leukemia:
-
Macrophages: Macrophages are phagocytic cells that play a key role in innate immunity and inflammation. In leukemia, macrophages can be activated by leukemic cells and inflammatory mediators, leading to the production of pro-inflammatory cytokines and chemokines. Macrophages can also contribute to the development of drug resistance in leukemic cells.
-
Neutrophils: Neutrophils are the most abundant type of white blood cell and play a critical role in fighting infections. In leukemia, neutrophils can be dysregulated, leading to impaired function and increased production of inflammatory mediators.
-
T Cells: T cells are lymphocytes that play a central role in adaptive immunity. In leukemia, T cells can be activated by leukemic cells and inflammatory mediators, leading to the production of cytokines and the killing of leukemic cells. However, T cells can also become exhausted or suppressed in the context of leukemia, contributing to immune evasion.
-
Natural Killer (NK) Cells: NK cells are cytotoxic lymphocytes that play a role in innate immunity. In leukemia, NK cells can recognize and kill leukemic cells, but their function can be impaired by inflammatory mediators and immune suppressive mechanisms.
Inflammation in Different Leukemia Subtypes
The role of inflammation can vary depending on the specific subtype of leukemia:
-
Acute Myeloid Leukemia (AML): AML is characterized by the rapid proliferation of immature myeloid cells. Inflammation is a prominent feature of AML, with elevated levels of pro-inflammatory cytokines and chemokines. Inflammation can contribute to disease progression, drug resistance, and the development of complications like sepsis.
-
Acute Lymphoblastic Leukemia (ALL): ALL is characterized by the rapid proliferation of immature lymphoid cells. Inflammation is also implicated in the pathogenesis of ALL, with elevated levels of pro-inflammatory cytokines and chemokines. Inflammation can contribute to disease progression, drug resistance, and the development of complications like CRS.
-
Chronic Myeloid Leukemia (CML): CML is characterized by the overproduction of mature myeloid cells. Inflammation is less prominent in CML compared to AML and ALL, but elevated levels of inflammatory mediators can still be observed. Inflammation can contribute to disease progression and the development of complications like blast crisis.
-
Myelodysplastic Syndromes (MDS): MDS are a group of clonal hematopoietic disorders characterized by ineffective hematopoiesis and an increased risk of developing AML. Inflammation is a key feature of MDS, with elevated levels of pro-inflammatory cytokines and chemokines. Inflammation can contribute to disease progression, cytopenias, and the development of complications like infections.
Therapeutic Implications
Targeting inflammatory pathways and mediators represents a promising strategy for improving outcomes in leukemia:
-
Cytokine Inhibitors: Monoclonal antibodies or small molecule inhibitors that target specific cytokines, such as IL-1, IL-6, or TNF-α, can reduce inflammation and improve systemic symptoms.
-
JAK Inhibitors: JAK inhibitors, such as ruxolitinib, can block the activation of the JAK-STAT pathway, reducing inflammation and improving hematopoiesis in certain leukemia subtypes.
-
NF-κB Inhibitors: Inhibitors of NF-κB signaling can reduce inflammation and promote apoptosis of leukemic cells.
-
Anti-inflammatory Drugs: Non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids can reduce inflammation and alleviate systemic symptoms in leukemia patients.
Conclusion
Inflammation plays a complex and multifaceted role in the pathogenesis and progression of leukemia. Understanding the intricate interplay between inflammatory pathways, cytokines, and immune cells is crucial for developing effective therapeutic strategies that target inflammation and improve outcomes in leukemia patients. Further research is needed to fully elucidate the role of inflammation in different leukemia subtypes and to identify novel therapeutic targets that can modulate inflammatory responses and enhance the efficacy of conventional therapies.







Leave a Reply