“Integrative Medicine in Chronic Disease Care – Part 6: Personalized Nutrition and the Gut Microbiome
Related Articles Integrative Medicine in Chronic Disease Care – Part 6: Personalized Nutrition and the Gut Microbiome
- Emerging Therapies For Managing Chronic Conditions – Part 3
- Dietary Strategies For Coping With Chronic Diseases – Part 4
- Long-term Effects Of Chronic Illness On Children – Part 4
- The Impact Of Chronic Disease On Family Dynamics – Part 3: Coping Strategies, Resilience, And Seeking Support
- Sleep Disorders And Chronic Disease Relationships – Part 2
Introduction
With great enthusiasm, let’s explore interesting topics related to Integrative Medicine in Chronic Disease Care – Part 6: Personalized Nutrition and the Gut Microbiome. Come on knit interesting information and provide new insights to readers.
Table of Content
Integrative Medicine in Chronic Disease Care – Part 6: Personalized Nutrition and the Gut Microbiome
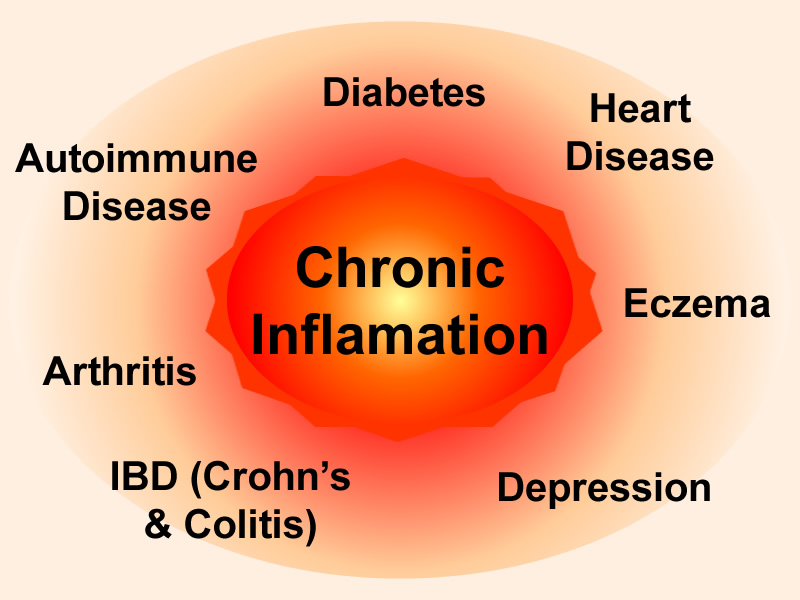
Chronic diseases, such as cardiovascular disease, diabetes, autoimmune disorders, and certain cancers, pose a significant global health challenge. These conditions are often characterized by long-term inflammation, immune dysfunction, and metabolic imbalances. While conventional medical treatments play a crucial role in managing chronic diseases, integrative medicine offers a complementary approach that addresses the root causes of illness and promotes overall well-being.
One of the cornerstones of integrative medicine is personalized nutrition. Recognizing that each individual has unique dietary needs and responses, personalized nutrition aims to optimize health by tailoring dietary recommendations to an individual’s specific genetic makeup, lifestyle, and health status. In recent years, the gut microbiome has emerged as a key player in personalized nutrition, as it significantly influences nutrient absorption, immune function, and overall health.
The Gut Microbiome: A Complex Ecosystem
The gut microbiome is a complex community of trillions of microorganisms, including bacteria, viruses, fungi, and archaea, that reside in the human digestive tract. This intricate ecosystem plays a vital role in various physiological processes, including:
- Nutrient Metabolism: Gut microbes aid in the digestion of complex carbohydrates, fibers, and other nutrients that the human body cannot break down on its own. They also synthesize essential vitamins, such as vitamin K and certain B vitamins.
- Immune System Regulation: The gut microbiome interacts closely with the immune system, helping to train and regulate immune responses. It promotes the development of immune cells and helps maintain a balance between pro-inflammatory and anti-inflammatory responses.
- Gut Barrier Function: The gut microbiome contributes to the integrity of the gut barrier, a protective layer that prevents harmful substances from entering the bloodstream. A compromised gut barrier, often referred to as "leaky gut," can lead to systemic inflammation and immune activation.
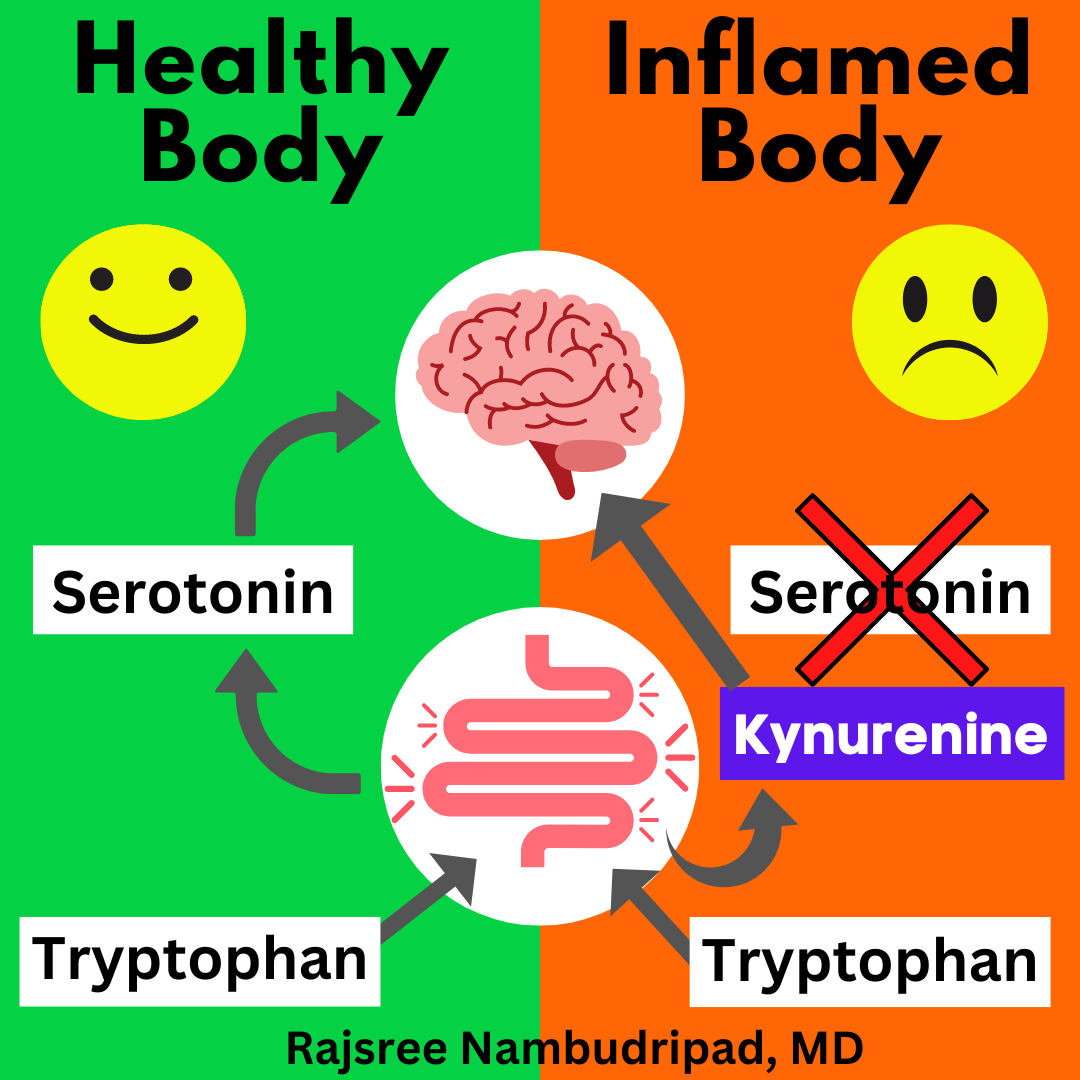
- Neurotransmitter Production: Gut microbes produce neurotransmitters, such as serotonin, dopamine, and GABA, which play a crucial role in mood regulation, sleep, and cognitive function.
- Protection Against Pathogens: The gut microbiome competes with pathogenic microorganisms for nutrients and space, preventing them from colonizing the gut and causing infections.
The Gut Microbiome and Chronic Diseases
Dysbiosis, an imbalance in the composition and function of the gut microbiome, has been linked to the development and progression of various chronic diseases. Several factors can contribute to dysbiosis, including:
- Diet: A diet high in processed foods, sugar, and unhealthy fats can negatively impact the gut microbiome, promoting the growth of harmful bacteria and reducing the diversity of beneficial microbes.
- Antibiotics: Antibiotics can disrupt the gut microbiome, killing both harmful and beneficial bacteria. This can lead to a decrease in microbial diversity and an increased risk of opportunistic infections.
- Stress: Chronic stress can alter the gut microbiome, increasing the abundance of stress-related bacteria and reducing the levels of beneficial microbes.
- Environmental Factors: Exposure to environmental toxins, such as pesticides and pollutants, can also negatively affect the gut microbiome.
Personalized Nutrition Strategies for Optimizing the Gut Microbiome
Personalized nutrition strategies that target the gut microbiome can be highly effective in managing chronic diseases. These strategies include:
-
Dietary Modifications:
- Increase Fiber Intake: Fiber-rich foods, such as fruits, vegetables, whole grains, and legumes, provide fuel for beneficial gut bacteria. Different types of fiber promote the growth of different microbial species, so it is important to consume a variety of fiber-rich foods.
- Limit Processed Foods, Sugar, and Unhealthy Fats: These foods can promote the growth of harmful bacteria and contribute to inflammation.
- Incorporate Fermented Foods: Fermented foods, such as yogurt, kefir, sauerkraut, kimchi, and kombucha, contain live microorganisms that can help replenish and diversify the gut microbiome.
- Consider a Plant-Based Diet: Plant-based diets are generally high in fiber and antioxidants, which can promote a healthy gut microbiome.
-
Probiotic Supplementation:
- Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. Probiotic supplements can help restore balance to the gut microbiome, improve digestion, and enhance immune function.
- It is important to choose a probiotic supplement that contains strains of bacteria that have been shown to be effective for specific health conditions.
- It is also important to consider the dosage and duration of probiotic supplementation.
-
Prebiotic Supplementation:
- Prebiotics are non-digestible food ingredients that promote the growth and activity of beneficial gut bacteria. Prebiotic supplements can help nourish and support the gut microbiome, improving its overall function.
- Common prebiotics include inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS).
-
Fecal Microbiota Transplantation (FMT):
- FMT involves transferring fecal matter from a healthy donor to a recipient in order to restore a healthy gut microbiome.
- FMT has shown promising results in the treatment of certain chronic diseases, such as recurrent Clostridium difficile infection and inflammatory bowel disease.
- FMT is typically performed in a clinical setting under the supervision of a healthcare professional.
The Role of Integrative Medicine Practitioners
Integrative medicine practitioners play a crucial role in helping individuals optimize their gut microbiome and manage chronic diseases through personalized nutrition strategies. These practitioners can:
- Assess the Gut Microbiome: Integrative medicine practitioners may use stool testing to assess the composition and function of an individual’s gut microbiome. This information can help identify imbalances and guide personalized nutrition recommendations.
- Develop Personalized Nutrition Plans: Integrative medicine practitioners can develop individualized dietary plans that take into account an individual’s specific needs, preferences, and health goals.
- Recommend Probiotic and Prebiotic Supplements: Integrative medicine practitioners can recommend appropriate probiotic and prebiotic supplements based on an individual’s gut microbiome profile and health condition.
- Provide Education and Support: Integrative medicine practitioners can provide education and support to help individuals make sustainable dietary changes and maintain a healthy gut microbiome.
Conclusion
Personalized nutrition, guided by an understanding of the gut microbiome, holds immense potential for managing chronic diseases. By tailoring dietary recommendations to an individual’s unique needs and promoting a healthy gut microbiome, integrative medicine can help address the root causes of illness, reduce inflammation, and improve overall well-being. Working with an integrative medicine practitioner can empower individuals to take control of their health and optimize their gut microbiome for a healthier, more vibrant life.
Future Directions
Research on the gut microbiome is rapidly evolving, and new discoveries are constantly being made. Future research will likely focus on:
- Identifying specific microbial signatures associated with different chronic diseases.
- Developing more targeted and effective probiotic and prebiotic therapies.
- Understanding the complex interactions between the gut microbiome, diet, and the immune system.
- Developing personalized nutrition strategies based on an individual’s genetic makeup and gut microbiome profile.
As our understanding of the gut microbiome continues to grow, personalized nutrition will play an increasingly important role in the prevention and management of chronic diseases.
Semoga artikel ini membantu!







Leave a Reply