“How to Read Your Lipid Panel: A Comprehensive Guide to Understanding Your Heart Health
Related Articles How to Read Your Lipid Panel: A Comprehensive Guide to Understanding Your Heart Health
- Mental Health Interventions For Chronic Disease Patients – Part 2: Targeted Approaches And Emerging Strategies
- Understanding Chronic Diseases: Causes And Management
- Swimming And Its Benefits For The Heart
- Alternative Therapies For Chronic Pain Management – Part 8
- Long-term Effects Of Chronic Illness On Children – Part 3
Introduction
We will be happy to explore interesting topics related to How to Read Your Lipid Panel: A Comprehensive Guide to Understanding Your Heart Health. Let’s knit interesting information and provide new insights to readers.
Table of Content
How to Read Your Lipid Panel: A Comprehensive Guide to Understanding Your Heart Health
Your lipid panel, also known as a lipid profile, is a blood test that measures the levels of specific fats (lipids) in your blood. This test is a crucial tool for assessing your risk of developing heart disease and other cardiovascular problems. Understanding the numbers on your lipid panel empowers you to take control of your health and make informed decisions about your lifestyle and treatment options.
Why is a Lipid Panel Important?
Lipids, primarily cholesterol and triglycerides, play essential roles in the body. Cholesterol is vital for building cell membranes and producing hormones, while triglycerides store energy. However, when these lipids are present in excessive amounts or in the wrong proportions, they can contribute to the buildup of plaque in your arteries, a condition called atherosclerosis. Atherosclerosis narrows the arteries, restricting blood flow and increasing the risk of:
- Heart attack: Blockage of blood flow to the heart muscle.
- Stroke: Blockage of blood flow to the brain.
- Peripheral artery disease (PAD): Narrowing of arteries in the limbs, leading to pain and reduced mobility.
Who Needs a Lipid Panel?
The American Heart Association (AHA) recommends that adults have their cholesterol checked every 4 to 6 years, starting at age 20. However, your healthcare provider may recommend more frequent testing if you have:
- A family history of heart disease
- High blood pressure
- Diabetes
- Overweight or obesity
- An unhealthy lifestyle (e.g., smoking, poor diet, lack of exercise)
- Existing heart disease or other risk factors
Children and adolescents may also need a lipid panel if they have risk factors for heart disease, such as a family history of early heart disease or obesity.
Preparing for Your Lipid Panel
To ensure accurate results, it’s essential to follow your healthcare provider’s instructions before your lipid panel. Typically, you’ll need to:
- Fast for 9-12 hours: This means no food or beverages (except water) before the test. Fasting helps ensure that triglyceride levels are not artificially elevated due to recent food intake.
- Inform your doctor about medications: Certain medications, such as birth control pills, diuretics, and some blood pressure medications, can affect lipid levels.
- Avoid alcohol: Alcohol can raise triglyceride levels, so it’s best to avoid it for at least 24 hours before the test.
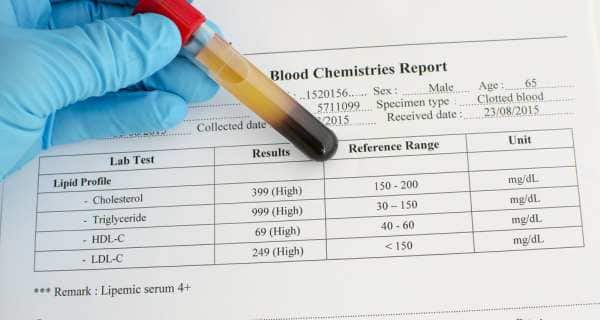
Understanding the Numbers on Your Lipid Panel
Your lipid panel typically includes the following measurements:
-
Total Cholesterol: This is the sum of all cholesterol in your blood, including LDL, HDL, and other lipoproteins.
- Desirable: Less than 200 mg/dL
- Borderline High: 200-239 mg/dL
- High: 240 mg/dL or higher
-
LDL Cholesterol (Low-Density Lipoprotein): Often referred to as "bad" cholesterol, LDL carries cholesterol from the liver to the rest of the body. High levels of LDL can contribute to plaque buildup in the arteries.
- Optimal: Less than 100 mg/dL (For people with heart disease or diabetes, even lower levels may be recommended.)
- Near Optimal/Above Optimal: 100-129 mg/dL
- Borderline High: 130-159 mg/dL
- High: 160-189 mg/dL
- Very High: 190 mg/dL or higher
-
HDL Cholesterol (High-Density Lipoprotein): Known as "good" cholesterol, HDL helps remove cholesterol from the arteries and transport it back to the liver for processing. Higher levels of HDL are associated with a lower risk of heart disease.
- Desirable: 60 mg/dL or higher
- Acceptable: 40-59 mg/dL
- Undesirable: Less than 40 mg/dL
-
Triglycerides: These are a type of fat in your blood that stores excess calories. High triglyceride levels can contribute to heart disease, especially when combined with high LDL and low HDL.
- Normal: Less than 150 mg/dL
- Borderline High: 150-199 mg/dL
- High: 200-499 mg/dL
- Very High: 500 mg/dL or higher
Beyond the Numbers: Factors Influencing Your Lipid Profile
While the numbers on your lipid panel provide valuable information, it’s important to remember that they are just one piece of the puzzle. Several factors can influence your lipid profile, including:
- Genetics: Your genes play a significant role in determining your cholesterol and triglyceride levels.
- Age and Gender: Cholesterol levels tend to increase with age, and men generally have lower HDL levels than women.
- Diet: A diet high in saturated and trans fats can raise LDL cholesterol, while a diet rich in fiber and healthy fats can improve your lipid profile.
- Weight: Being overweight or obese can increase LDL cholesterol and triglycerides while lowering HDL cholesterol.
- Physical Activity: Regular exercise can lower LDL cholesterol and triglycerides while raising HDL cholesterol.
- Smoking: Smoking lowers HDL cholesterol and increases LDL cholesterol.
- Medical Conditions: Certain medical conditions, such as diabetes, kidney disease, and hypothyroidism, can affect lipid levels.
- Medications: Some medications, such as beta-blockers and diuretics, can raise cholesterol and triglyceride levels.
Interpreting Your Results and Taking Action
Your healthcare provider will consider your lipid panel results in conjunction with your other risk factors to determine your overall risk of heart disease. Based on this assessment, they may recommend:
- Lifestyle modifications: This includes adopting a heart-healthy diet, engaging in regular physical activity, maintaining a healthy weight, and quitting smoking.
- Medications: If lifestyle changes are not enough to lower your cholesterol or triglycerides, your doctor may prescribe medications such as statins, fibrates, or niacin.
- Regular monitoring: Your doctor will likely recommend regular lipid panel testing to monitor your progress and adjust your treatment plan as needed.
Lifestyle Changes to Improve Your Lipid Profile
Even if your cholesterol levels are within the normal range, adopting a heart-healthy lifestyle can help maintain optimal lipid levels and reduce your risk of heart disease. Here are some key lifestyle changes to consider:
-
Eat a Heart-Healthy Diet:
- Limit saturated and trans fats: These fats are found in red meat, processed foods, and fried foods.
- Choose healthy fats: Include sources of monounsaturated and polyunsaturated fats, such as olive oil, avocados, nuts, seeds, and fatty fish (salmon, tuna, mackerel).
- Increase fiber intake: Fiber helps lower LDL cholesterol. Good sources of fiber include fruits, vegetables, whole grains, and legumes.
- Reduce sugar intake: Excessive sugar consumption can raise triglyceride levels.
-
Engage in Regular Physical Activity:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week.
- Include strength training exercises at least twice a week.
-
Maintain a Healthy Weight:
- If you are overweight or obese, losing even a small amount of weight (5-10%) can significantly improve your lipid profile.
-
Quit Smoking:
- Smoking lowers HDL cholesterol and increases LDL cholesterol. Quitting smoking is one of the best things you can do for your heart health.
-
Limit Alcohol Consumption:
- Excessive alcohol consumption can raise triglyceride levels. If you drink alcohol, do so in moderation (up to one drink per day for women and up to two drinks per day for men).
When Medication is Necessary
In some cases, lifestyle changes alone may not be enough to lower your cholesterol or triglycerides to the desired levels. Your healthcare provider may then recommend medication, such as:
- Statins: These are the most commonly prescribed cholesterol-lowering drugs. They work by blocking an enzyme in the liver that produces cholesterol.
- Fibrates: These medications primarily lower triglyceride levels and can also raise HDL cholesterol.
- Niacin: Also known as vitamin B3, niacin can lower LDL cholesterol and triglycerides while raising HDL cholesterol.
- Bile Acid Sequestrants: These medications bind to bile acids in the intestine, preventing them from being reabsorbed and forcing the liver to use more cholesterol to produce bile.
- Cholesterol Absorption Inhibitors: These medications block the absorption of cholesterol from the small intestine.
- PCSK9 Inhibitors: These are newer injectable medications that can significantly lower LDL cholesterol, especially in people with familial hypercholesterolemia or those who have not responded well to other treatments.
The Importance of Regular Monitoring
Even if you are taking medication to lower your cholesterol, it’s essential to continue monitoring your lipid levels regularly. This allows your healthcare provider to assess the effectiveness of your treatment plan and make adjustments as needed. Regular monitoring also helps ensure that you are adhering to your lifestyle recommendations and taking your medication as prescribed.
In Conclusion
Understanding your lipid panel is a critical step in taking control of your heart health. By knowing your cholesterol and triglyceride levels and understanding the factors that influence them, you can work with your healthcare provider to develop a personalized plan to reduce your risk of heart disease. Remember, a heart-healthy lifestyle is the foundation of good cardiovascular health, and regular monitoring is essential for maintaining optimal lipid levels and preventing heart disease.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Always consult with your healthcare provider for diagnosis and treatment of any medical condition.








Leave a Reply