“How to Live a Full Life with Heart Failure
Related Articles How to Live a Full Life with Heart Failure
- Cardiovascular Complications Of COVID-19
- Rare Subtypes Of Leukemia: Diagnostic Dilemmas
- Economic Burden Of Chronic Illnesses: A Global Perspective
- Exercise For Seniors With Heart Disease: A Comprehensive Guide
- Alternative Therapies For Chronic Pain Management – Part 6
Introduction
With great enthusiasm, let’s explore interesting topics related to How to Live a Full Life with Heart Failure. Let’s knit interesting information and provide new insights to readers.
Table of Content
How to Live a Full Life with Heart Failure
Heart failure, a condition where the heart can’t pump enough blood to meet the body’s needs, can be a daunting diagnosis. It’s natural to feel overwhelmed, scared, or even hopeless. However, it’s crucial to remember that a diagnosis of heart failure doesn’t mean the end of a fulfilling life. With the right approach, lifestyle adjustments, and medical care, individuals with heart failure can continue to live rich, meaningful lives.
Understanding Heart Failure: The First Step to Empowerment
Before diving into strategies for living well, it’s essential to understand what heart failure is and how it affects the body. Heart failure doesn’t mean the heart has stopped working entirely. Instead, it signifies that the heart is struggling to pump blood efficiently. This can lead to a variety of symptoms, including:
- Shortness of breath: Especially during exertion or when lying down.
- Fatigue: Feeling tired and weak, even after rest.
- Swelling (edema): In the ankles, legs, and abdomen.
- Rapid or irregular heartbeat: Palpitations or a feeling of fluttering in the chest.
- Persistent cough or wheezing: Often with white or pink phlegm.
- Weight gain: Due to fluid retention.
- Lack of appetite or nausea: Due to fluid buildup in the abdomen.
- Difficulty concentrating or decreased alertness: Due to reduced blood flow to the brain.
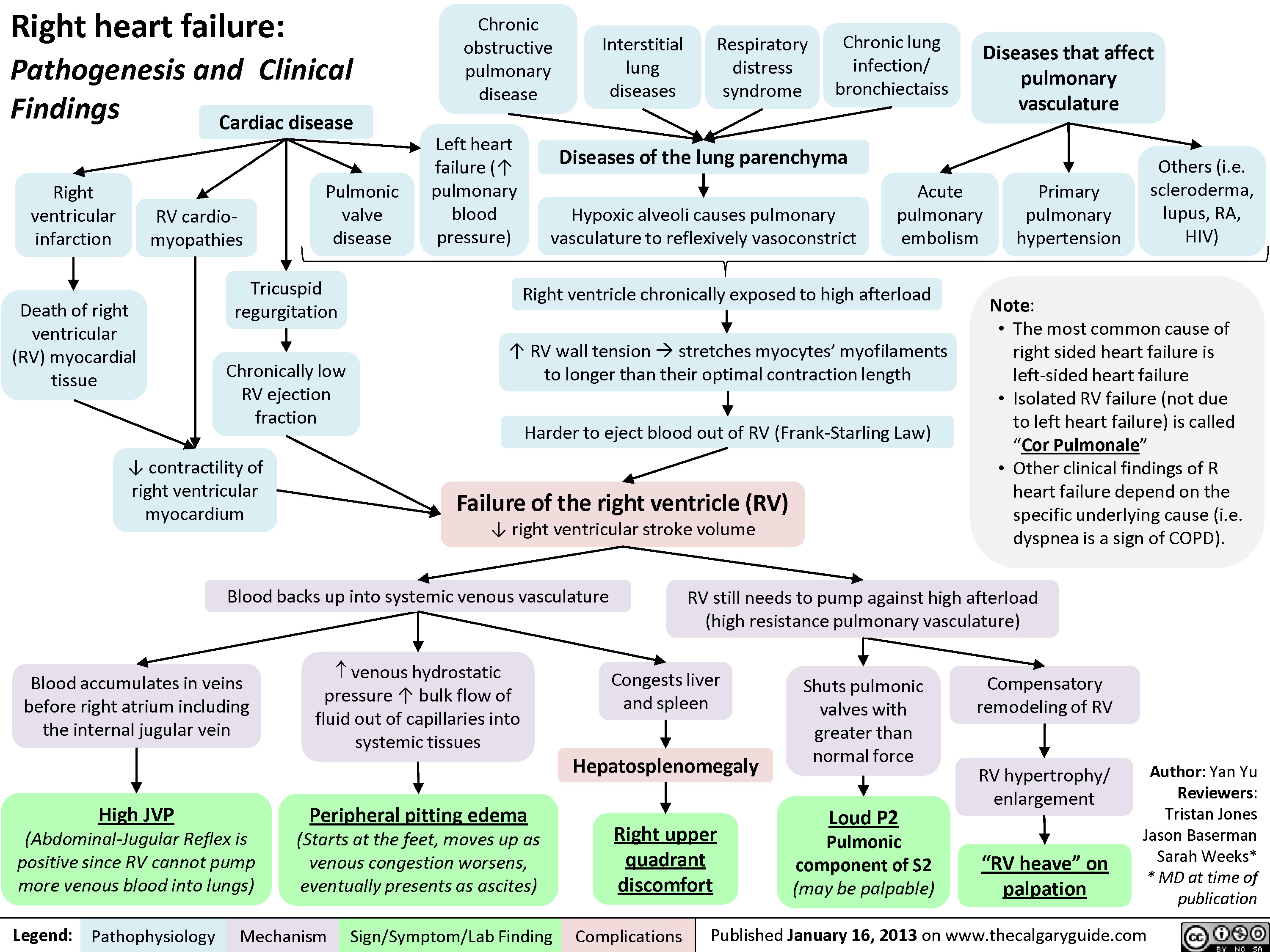
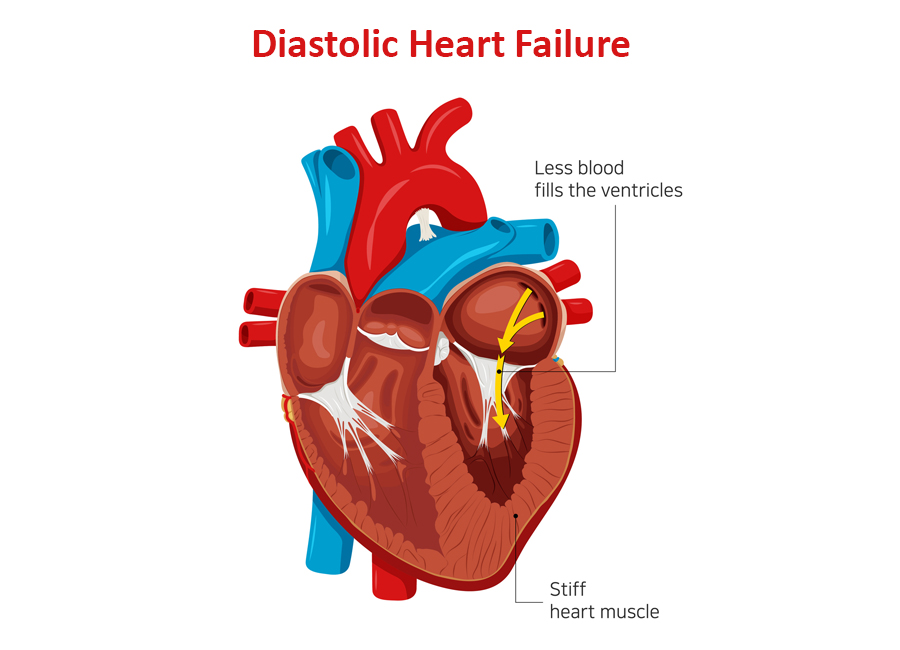
Understanding the specific type of heart failure you have (e.g., systolic, diastolic, or heart failure with preserved ejection fraction) and its causes (e.g., coronary artery disease, high blood pressure, valve disease) is vital for developing an effective management plan.
The Cornerstone of Living Well: Medical Management
The cornerstone of managing heart failure and living a full life is adhering to your medical treatment plan. This typically involves:
-
Medications:
- ACE inhibitors or ARBs: Help relax blood vessels and lower blood pressure.
- Beta-blockers: Slow the heart rate and lower blood pressure.
- Diuretics: Help the body eliminate excess fluid and reduce swelling.
- Digoxin: Helps the heart pump more forcefully.
- Aldosterone antagonists: Help reduce sodium and fluid retention.
- SGLT2 inhibitors: Newer medications that can improve heart failure outcomes.
It’s crucial to take medications as prescribed, understand their potential side effects, and communicate any concerns to your doctor.
-
Regular Check-ups: Frequent visits to your cardiologist or heart failure specialist are essential for monitoring your condition, adjusting medications, and addressing any emerging issues.
-
Cardiac Rehabilitation: If recommended, participate in a cardiac rehabilitation program. These programs provide supervised exercise, education, and support to help improve heart health and overall well-being.
-
Implantable Devices: In some cases, devices like pacemakers, implantable cardioverter-defibrillators (ICDs), or cardiac resynchronization therapy (CRT) devices may be necessary to regulate heart rhythm or improve heart function.
Lifestyle Adjustments: Empowering Yourself for a Better Quality of Life
Alongside medical treatment, lifestyle adjustments play a significant role in managing heart failure and enhancing your quality of life. These adjustments include:
-
Dietary Changes:
- Sodium Restriction: Limiting sodium intake is crucial to prevent fluid retention. Avoid processed foods, canned goods, and restaurant meals, which are often high in sodium. Aim for less than 2,000 milligrams of sodium per day.
- Fluid Restriction: In some cases, your doctor may recommend limiting fluid intake to prevent fluid overload. This may involve reducing your intake of water, juice, and other beverages.
- Heart-Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean protein. Limit saturated and trans fats, cholesterol, and added sugars.
- Potassium Intake: Some diuretics can deplete potassium levels. Your doctor may recommend increasing your potassium intake through foods like bananas, oranges, and potatoes, or through potassium supplements.
-
Regular Exercise:
- Consult Your Doctor: Before starting any exercise program, consult your doctor to determine a safe and appropriate level of activity.
- Start Slowly: Begin with gentle exercises like walking, swimming, or cycling, and gradually increase the intensity and duration as tolerated.
- Listen to Your Body: Pay attention to your body’s signals and stop if you experience shortness of breath, chest pain, dizziness, or fatigue.
- Cardiac Rehabilitation: Consider participating in a cardiac rehabilitation program, which provides supervised exercise and education.
-
Weight Management: Maintaining a healthy weight can reduce the strain on your heart. If you are overweight or obese, work with your doctor or a registered dietitian to develop a weight loss plan.
-
Smoking Cessation: If you smoke, quitting is one of the most important things you can do for your heart health. Smoking damages blood vessels and increases the risk of heart failure complications.
-
Alcohol Consumption: Limit alcohol consumption or avoid it altogether. Alcohol can weaken the heart muscle and worsen heart failure symptoms.
-
Stress Management:
- Identify Stressors: Identify the sources of stress in your life and develop strategies for managing them.
- Relaxation Techniques: Practice relaxation techniques like deep breathing, meditation, yoga, or tai chi.
- Hobbies and Interests: Engage in hobbies and activities that you enjoy and find relaxing.
- Social Support: Spend time with friends and family, and seek support from a therapist or counselor if needed.
-
Sleep Hygiene: Aim for 7-8 hours of quality sleep each night. Establish a regular sleep schedule, create a relaxing bedtime routine, and avoid caffeine and alcohol before bed.
-
Vaccinations: Get vaccinated against the flu and pneumonia, as these infections can worsen heart failure symptoms.
Emotional Well-being: Nurturing Your Mental Health
Living with heart failure can take a toll on your emotional well-being. It’s important to acknowledge and address your feelings of anxiety, depression, or fear.
- Seek Support: Talk to your doctor, a therapist, or a support group about your feelings. Sharing your experiences with others who understand can be incredibly helpful.
- Stay Connected: Maintain social connections with friends and family. Isolation can worsen feelings of depression and anxiety.
- Focus on the Positive: Focus on the things you can control and celebrate your successes, no matter how small.
- Practice Gratitude: Take time each day to appreciate the good things in your life.
- Set Realistic Goals: Set achievable goals for yourself and break them down into smaller steps.
- Engage in Activities You Enjoy: Make time for hobbies and activities that bring you joy and fulfillment.
Practical Considerations: Planning for the Future
Living with heart failure requires careful planning and preparation.
- Know Your Numbers: Keep track of your weight, blood pressure, heart rate, and other vital signs. Share this information with your doctor.
- Medication Management: Organize your medications and refill them on time. Use a pill organizer to help you keep track of your medications.
- Emergency Preparedness:
- Know the Signs of Worsening Heart Failure: Be aware of the signs of worsening heart failure, such as increased shortness of breath, swelling, or chest pain.
- Develop an Emergency Plan: Have a plan in place for what to do if you experience these symptoms. This may involve calling your doctor, going to the emergency room, or calling 911.
- Carry a Medical ID: Wear a medical ID bracelet or necklace that identifies you as having heart failure and lists your medications.
- Financial Planning: Heart failure can be expensive to manage. Explore resources for financial assistance, such as government programs, charitable organizations, and pharmaceutical assistance programs.
- Advance Care Planning: Discuss your wishes for end-of-life care with your doctor and family members. Consider creating an advance directive, such as a living will or durable power of attorney for healthcare.
Advocating for Yourself: Taking an Active Role in Your Care
You are the most important member of your healthcare team. Take an active role in your care by:
- Asking Questions: Don’t be afraid to ask your doctor questions about your condition, medications, and treatment plan.
- Seeking Second Opinions: If you are unsure about your diagnosis or treatment plan, seek a second opinion from another cardiologist or heart failure specialist.
- Staying Informed: Stay up-to-date on the latest research and treatments for heart failure.
- Participating in Clinical Trials: Consider participating in clinical trials to help advance the understanding and treatment of heart failure.
Living a Full Life: Embracing the Present
Living with heart failure can be challenging, but it doesn’t have to define you. By understanding your condition, adhering to your medical treatment plan, making lifestyle adjustments, and prioritizing your emotional well-being, you can live a full and meaningful life. Focus on the present, embrace the things you enjoy, and cherish the moments you have with loved ones. Remember, you are not alone, and there is hope for a brighter future.
Disclaimer: This article provides general information and should not be considered medical advice. Consult with your doctor or other qualified healthcare professional for any questions you have about your health or treatment.







Leave a Reply