“Heart Failure: Causes, Symptoms, and Treatment
Related Articles Heart Failure: Causes, Symptoms, and Treatment
- The Impact Of Chronic Disease On Family Dynamics
- Holistic Approaches To Chronic Disease Prevention – Part 7: Integrating Mind-Body Practices For Enhanced Well-being
- Holistic Wellness Programs For Chronic Disease Patients – Part 4
- Holistic Wellness Programs For Chronic Disease Patients – Part 6
- Integrative Medicine In Chronic Disease Care – Part 6: Personalized Nutrition And The Gut Microbiome
Introduction
On this special occasion, we are happy to review interesting topics related to Heart Failure: Causes, Symptoms, and Treatment. Let’s knit interesting information and provide new insights to readers.
Heart Failure: Causes, Symptoms, and Treatment
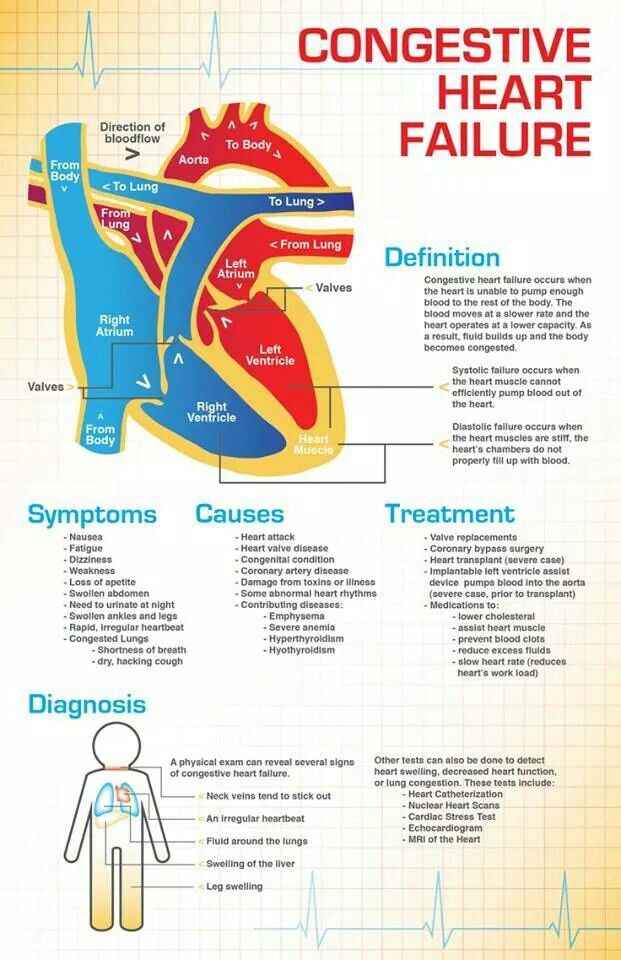
Heart failure, often referred to as congestive heart failure (CHF), is a chronic, progressive condition in which the heart muscle is unable to pump enough blood to meet the body’s needs for oxygen and nutrients. It doesn’t mean the heart has stopped working entirely, but rather that it’s not working as efficiently as it should. This can lead to a variety of symptoms, impacting a person’s quality of life. Understanding the causes, recognizing the symptoms, and exploring the available treatment options are crucial for managing heart failure effectively and improving outcomes.
Causes of Heart Failure
Heart failure can result from a variety of underlying conditions that damage or weaken the heart muscle. These causes can be broadly categorized into:
-
Coronary Artery Disease (CAD): This is the most common cause of heart failure. CAD occurs when the arteries that supply blood to the heart become narrowed or blocked by plaque buildup (atherosclerosis). This reduces blood flow to the heart muscle, leading to angina (chest pain) and, over time, weakening of the heart. A heart attack (myocardial infarction), which is a complete blockage of a coronary artery, can cause significant damage to the heart muscle, leading to heart failure.
-
High Blood Pressure (Hypertension): Over time, high blood pressure forces the heart to work harder to pump blood throughout the body. This increased workload can cause the heart muscle to thicken (hypertrophy). The thickened heart muscle becomes stiff and less efficient at filling with blood, eventually leading to heart failure.
-
Valvular Heart Disease: The heart has four valves that ensure blood flows in the correct direction. Damaged or diseased heart valves can cause the heart to work harder to pump blood. Stenosis (narrowing) of a valve restricts blood flow, while regurgitation (leakage) allows blood to flow backward. Both conditions can strain the heart and lead to heart failure. Common valve problems include aortic stenosis, mitral regurgitation, and aortic regurgitation.
-
Cardiomyopathy: This refers to diseases of the heart muscle itself. There are several types of cardiomyopathy:
- Dilated Cardiomyopathy: The heart chambers enlarge and the heart muscle becomes weak and thin. This is the most common type of cardiomyopathy and can be caused by genetic factors, viral infections, alcohol abuse, drug use, or certain medical conditions.
- Hypertrophic Cardiomyopathy: The heart muscle becomes abnormally thick, making it harder for the heart to pump blood. This is often caused by genetic mutations.
- Restrictive Cardiomyopathy: The heart muscle becomes stiff and less elastic, making it difficult for the heart to fill with blood. This is the least common type of cardiomyopathy and can be caused by conditions such as amyloidosis, sarcoidosis, or hemochromatosis.
-
Congenital Heart Defects: These are structural abnormalities of the heart that are present at birth. They can range from minor to severe and may require surgery to correct. Some congenital heart defects can lead to heart failure later in life.
-
Arrhythmias: Irregular heart rhythms (arrhythmias) can either cause the heart to beat too fast (tachycardia) or too slow (bradycardia). Both can impair the heart’s ability to pump blood effectively and lead to heart failure. Atrial fibrillation is a common arrhythmia that can contribute to heart failure.
-
Myocarditis: This is inflammation of the heart muscle, usually caused by a viral infection. Myocarditis can weaken the heart muscle and lead to heart failure.
-
Other Medical Conditions: Certain medical conditions can increase the risk of heart failure, including:
- Diabetes: High blood sugar levels can damage the heart muscle and blood vessels.
- Obesity: Excess weight puts extra strain on the heart.
- Chronic Kidney Disease: Kidney disease can lead to fluid retention and high blood pressure, both of which can contribute to heart failure.
- Thyroid Disorders: Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can affect heart function.
- Sleep Apnea: This condition, in which breathing repeatedly stops and starts during sleep, can put strain on the heart.
-
Substance Abuse: Excessive alcohol consumption and the use of illicit drugs, such as cocaine and methamphetamine, can damage the heart muscle and lead to heart failure.
-
Certain Medications: Some medications, such as certain chemotherapy drugs, can have toxic effects on the heart and increase the risk of heart failure.
Symptoms of Heart Failure
The symptoms of heart failure can vary depending on the severity of the condition, the underlying cause, and the individual’s overall health. Common symptoms include:
-
Shortness of Breath (Dyspnea): This is one of the most common symptoms of heart failure. It can occur during exertion, such as walking or climbing stairs, or even at rest, especially when lying down (orthopnea). Shortness of breath is caused by fluid buildup in the lungs (pulmonary congestion).
-
Fatigue: Feeling tired and weak is another common symptom. The heart’s inability to pump enough blood to meet the body’s needs can lead to fatigue, even with minimal activity.
-
Swelling (Edema): Fluid retention can cause swelling in the ankles, legs, feet, and abdomen (ascites). This is caused by the kidneys retaining more sodium and water due to reduced blood flow.
-
Persistent Coughing or Wheezing: Fluid buildup in the lungs can cause a persistent cough, which may produce white or pink-tinged phlegm. Wheezing may also occur.
-
Rapid or Irregular Heartbeat: The heart may beat faster or irregularly in an attempt to compensate for its reduced pumping ability. This can lead to palpitations (feeling like the heart is racing or fluttering).
-
Weight Gain: Fluid retention can lead to rapid weight gain.
-
Lack of Appetite or Nausea: Fluid buildup in the abdomen can put pressure on the digestive system, leading to a loss of appetite or nausea.
-
Difficulty Concentrating or Reduced Alertness: Reduced blood flow to the brain can cause difficulty concentrating, memory problems, or reduced alertness.
-
Increased Urination at Night (Nocturia): When lying down, fluid that has accumulated in the legs and ankles during the day is reabsorbed into the bloodstream, leading to increased urination at night.
Diagnosis of Heart Failure
Diagnosing heart failure typically involves a combination of:
-
Medical History and Physical Exam: The doctor will ask about your symptoms, medical history, and risk factors for heart disease. They will also perform a physical exam to check for signs of heart failure, such as swelling, abnormal heart sounds, and fluid in the lungs.
-
Echocardiogram: This is an ultrasound of the heart that provides information about the size, shape, and function of the heart chambers and valves. It can help determine the ejection fraction, which is the percentage of blood pumped out of the heart with each beat. A low ejection fraction is a sign of heart failure.
-
Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can help identify arrhythmias, heart attacks, and other heart problems.
-
Chest X-Ray: This can show whether the heart is enlarged or if there is fluid in the lungs.
-
Blood Tests: Blood tests can help assess kidney function, liver function, thyroid function, and levels of certain hormones that are elevated in heart failure, such as B-type natriuretic peptide (BNP).
-
Stress Test: This test involves monitoring the heart’s electrical activity and blood pressure while you exercise on a treadmill or stationary bike. It can help determine if there is reduced blood flow to the heart muscle.
-
Cardiac Catheterization: This is an invasive procedure in which a thin tube (catheter) is inserted into a blood vessel in the arm or leg and guided to the heart. It can be used to measure pressures in the heart chambers and coronary arteries and to take biopsies of the heart muscle.
Treatment of Heart Failure
The goals of heart failure treatment are to relieve symptoms, improve quality of life, slow the progression of the disease, and prolong survival. Treatment typically involves a combination of:
-
Lifestyle Changes:
- Dietary Modifications: Limiting sodium intake, reducing fluid intake, and eating a heart-healthy diet that is low in saturated fat, cholesterol, and trans fat.
- Regular Exercise: Engaging in regular aerobic exercise, such as walking, swimming, or cycling, can improve heart function and overall health.
- Weight Management: Maintaining a healthy weight can reduce the strain on the heart.
- Smoking Cessation: Quitting smoking is essential for improving heart health.
- Alcohol Moderation: Limiting alcohol consumption or avoiding it altogether.
- Stress Management: Practicing stress-reducing techniques, such as yoga, meditation, or deep breathing.
-
Medications:
- Angiotensin-Converting Enzyme (ACE) Inhibitors: These medications help relax blood vessels and lower blood pressure, making it easier for the heart to pump blood.
- Angiotensin II Receptor Blockers (ARBs): These medications work similarly to ACE inhibitors and are often used in people who cannot tolerate ACE inhibitors.
- Beta-Blockers: These medications slow the heart rate and lower blood pressure, reducing the workload on the heart.
- Diuretics: These medications help the body eliminate excess fluid, reducing swelling and shortness of breath.
- Digoxin: This medication helps the heart beat more strongly and efficiently.
- Aldosterone Antagonists: These medications block the effects of aldosterone, a hormone that can cause sodium and water retention.
- Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors: These medications were initially developed for diabetes, but have been shown to improve outcomes in people with heart failure, even those without diabetes.
- Angiotensin Receptor-Neprilysin Inhibitor (ARNI): These medications combine an ARB with a neprilysin inhibitor, which helps to increase levels of natriuretic peptides, hormones that promote sodium and water excretion and relax blood vessels.
-
Devices:
- Implantable Cardioverter-Defibrillator (ICD): This device is implanted in the chest and monitors the heart rhythm. If it detects a life-threatening arrhythmia, it delivers an electrical shock to restore a normal heart rhythm.
- Cardiac Resynchronization Therapy (CRT): This device is similar to a pacemaker and helps to coordinate the contractions of the heart chambers, improving the heart’s pumping efficiency.
- Left Ventricular Assist Device (LVAD): This is a mechanical pump that is implanted in the chest to help the heart pump blood. It is typically used in people with severe heart failure who are waiting for a heart transplant or who are not candidates for a transplant.
-
Surgery:
- Coronary Artery Bypass Grafting (CABG): This surgery involves bypassing blocked coronary arteries with healthy blood vessels taken from other parts of the body.
- Valve Repair or Replacement: Damaged or diseased heart valves can be repaired or replaced with artificial valves.
- Heart Transplant: This is a last-resort option for people with severe heart failure who have not responded to other treatments.
Prognosis and Management
Heart failure is a chronic condition that requires ongoing management. With proper treatment and lifestyle changes, many people with heart failure can live active and fulfilling lives. However, heart failure can worsen over time, leading to complications such as:
- Kidney Damage: Reduced blood flow to the kidneys can lead to kidney damage.
- Liver Damage: Fluid buildup in the liver can lead to liver damage.
- Pulmonary Hypertension: High blood pressure in the arteries of the lungs.
- Arrhythmias: Irregular heart rhythms.
- Sudden Cardiac Arrest: A sudden loss of heart function.
Regular follow-up appointments with a cardiologist are essential for monitoring heart function, adjusting medications as needed, and managing any complications that may arise. It’s also important to be aware of the signs and symptoms of worsening heart failure and to seek medical attention promptly if they occur.
Conclusion
Heart failure is a complex and challenging condition, but with a comprehensive approach to diagnosis, treatment, and lifestyle management, individuals can effectively manage their symptoms, improve their quality of life, and potentially prolong their survival. Understanding the causes, recognizing the symptoms, and adhering to the recommended treatment plan are crucial for achieving the best possible outcomes.







Leave a Reply