“Heart Disease and Kidney Health: Intersections and Implications
Related Articles Heart Disease and Kidney Health: Intersections and Implications
- Understanding Chronic Diseases: Causes And Management – Part 8
- Integrative Medicine In Chronic Disease Care – Part 10: The Role Of Mind-Body Therapies In Managing Chronic Pain
- Leukemia Epidemiology: Global Trends And Regional Variances
- The Impact Of Chronic Illness On Mental Health – Part 2: Coping, Support, And Thriving
- The Role Of Stress In Chronic Disease Progression – Part 3
Introduction
On this special occasion, we are happy to review interesting topics related to Heart Disease and Kidney Health: Intersections and Implications. Come on knit interesting information and provide new insights to readers.
Table of Content
Heart Disease and Kidney Health: Intersections and Implications
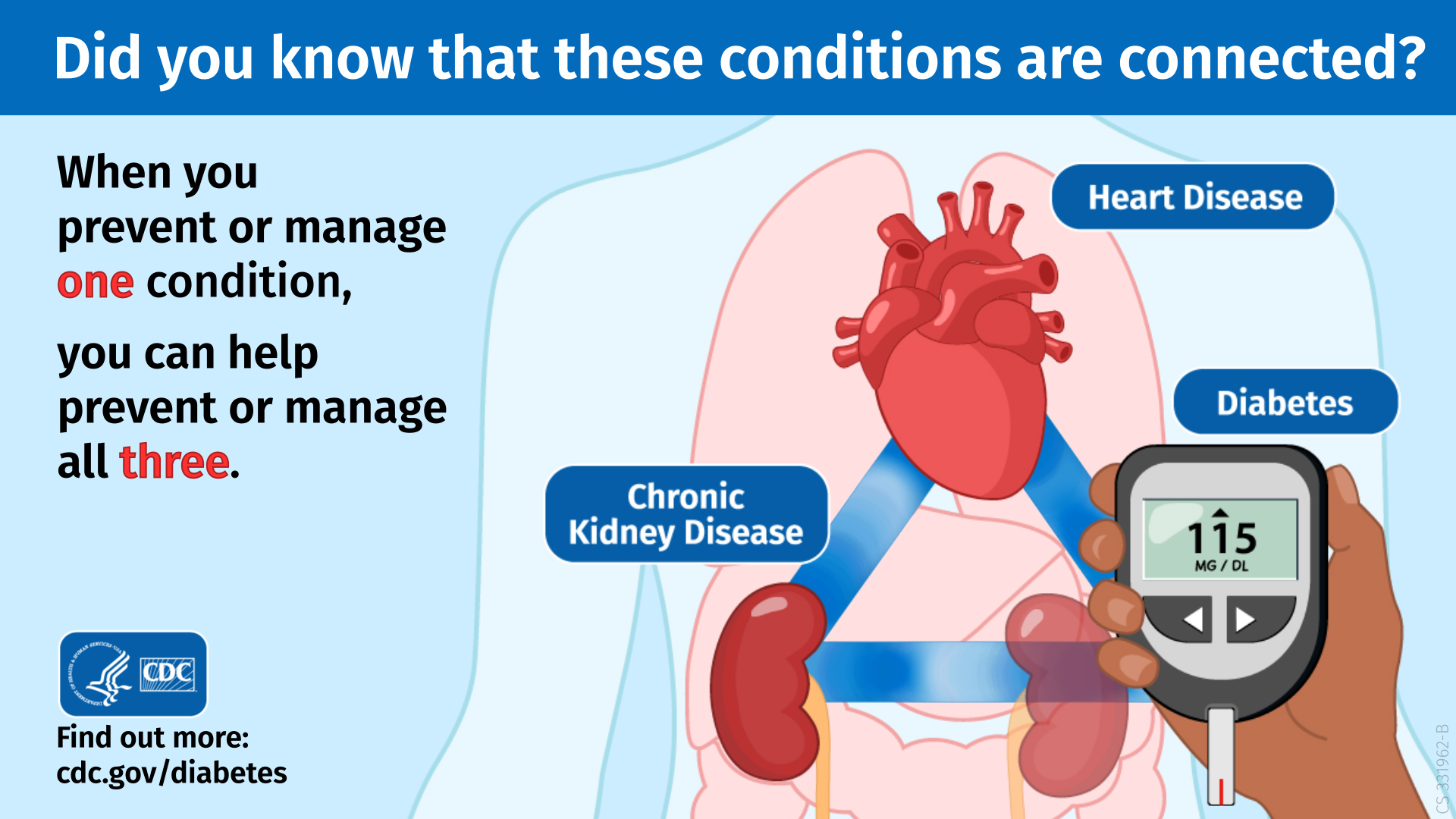
Heart disease and kidney disease are two major global health challenges, often coexisting and exacerbating each other. The intricate relationship between these two conditions has significant implications for individuals and healthcare systems. This article explores the complex intersections between heart disease and kidney health, shedding light on the underlying mechanisms, risk factors, diagnostic approaches, and management strategies.
The Cardio-Renal Connection: A Complex Interplay
The heart and kidneys are vital organs that work in synergy to maintain overall health. The heart pumps blood throughout the body, delivering oxygen and nutrients to organs and tissues. The kidneys filter waste products and excess fluid from the blood, regulating blood pressure, electrolyte balance, and red blood cell production. When either organ malfunctions, it can have cascading effects on the other, leading to a vicious cycle of dysfunction.
Several mechanisms contribute to the cardio-renal connection:
-
Hemodynamic Factors:
- Heart Failure: Heart failure, a condition in which the heart cannot pump enough blood to meet the body’s needs, can lead to reduced blood flow to the kidneys. This reduced perfusion can impair kidney function and contribute to the development or progression of chronic kidney disease (CKD).
- Hypertension: Hypertension, or high blood pressure, is a major risk factor for both heart disease and kidney disease. Sustained high blood pressure can damage the blood vessels in both organs, leading to heart attacks, strokes, and kidney failure.
- Atherosclerosis: Atherosclerosis, the buildup of plaque in the arteries, can affect blood flow to both the heart and kidneys. Reduced blood flow to the heart can cause chest pain (angina) or heart attack, while reduced blood flow to the kidneys can lead to kidney damage and CKD.
-
Inflammation and Oxidative Stress:
- Both heart disease and kidney disease are associated with chronic inflammation and oxidative stress. These processes can damage the blood vessels and tissues in both organs, contributing to the progression of both conditions.
-
Hormonal Imbalances:
- The kidneys produce hormones that regulate blood pressure, red blood cell production, and calcium metabolism. Kidney disease can disrupt these hormonal balances, leading to high blood pressure, anemia, and bone disease, all of which can negatively impact heart health.
- The heart also produces hormones, such as atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP), which help regulate fluid balance and blood pressure. Heart failure can lead to increased production of these hormones, which can have both beneficial and detrimental effects on kidney function.
-
Shared Risk Factors:
- Several risk factors are common to both heart disease and kidney disease, including diabetes, hypertension, obesity, smoking, and a family history of either condition. These shared risk factors highlight the importance of addressing lifestyle factors to prevent or manage both conditions.
Clinical Implications: Cardio-Renal Syndrome
The complex interplay between heart disease and kidney disease has led to the concept of cardio-renal syndrome (CRS). CRS encompasses a spectrum of disorders in which acute or chronic dysfunction in one organ leads to acute or chronic dysfunction in the other. There are five main types of CRS:
- Type 1 CRS: Acute heart failure leading to acute kidney injury.
- Type 2 CRS: Chronic heart failure leading to chronic kidney disease.
- Type 3 CRS: Acute kidney injury leading to acute heart dysfunction.
- Type 4 CRS: Chronic kidney disease leading to chronic heart dysfunction.
- Type 5 CRS: Systemic conditions (e.g., sepsis) leading to both heart and kidney dysfunction.
The presence of CRS significantly worsens the prognosis for patients with either heart disease or kidney disease. Patients with CRS have a higher risk of hospitalization, cardiovascular events, and death.
Diagnosis and Evaluation
Early diagnosis and evaluation are crucial for managing patients with both heart disease and kidney disease. Diagnostic approaches include:
-
Medical History and Physical Examination:
- A thorough medical history should include information about risk factors for both heart disease and kidney disease, such as diabetes, hypertension, family history, and smoking.
- A physical examination should assess blood pressure, heart rate, and signs of fluid overload, such as edema.
-
Laboratory Tests:
- Blood Tests: Blood tests can assess kidney function (e.g., creatinine, blood urea nitrogen), electrolyte balance, and red blood cell count. They can also measure cardiac biomarkers (e.g., troponin, BNP) to assess heart function.
- Urine Tests: Urine tests can detect protein in the urine (proteinuria), which is a sign of kidney damage.
-
Imaging Studies:
- Echocardiography: Echocardiography uses sound waves to create images of the heart, allowing doctors to assess heart function and structure.
- Electrocardiography (ECG): An ECG records the electrical activity of the heart and can detect abnormalities in heart rhythm or signs of heart damage.
- Kidney Ultrasound: A kidney ultrasound can assess the size and structure of the kidneys and detect any abnormalities, such as cysts or tumors.
Management Strategies
Managing patients with both heart disease and kidney disease requires a multidisciplinary approach that addresses both conditions simultaneously. Management strategies include:
-
Lifestyle Modifications:
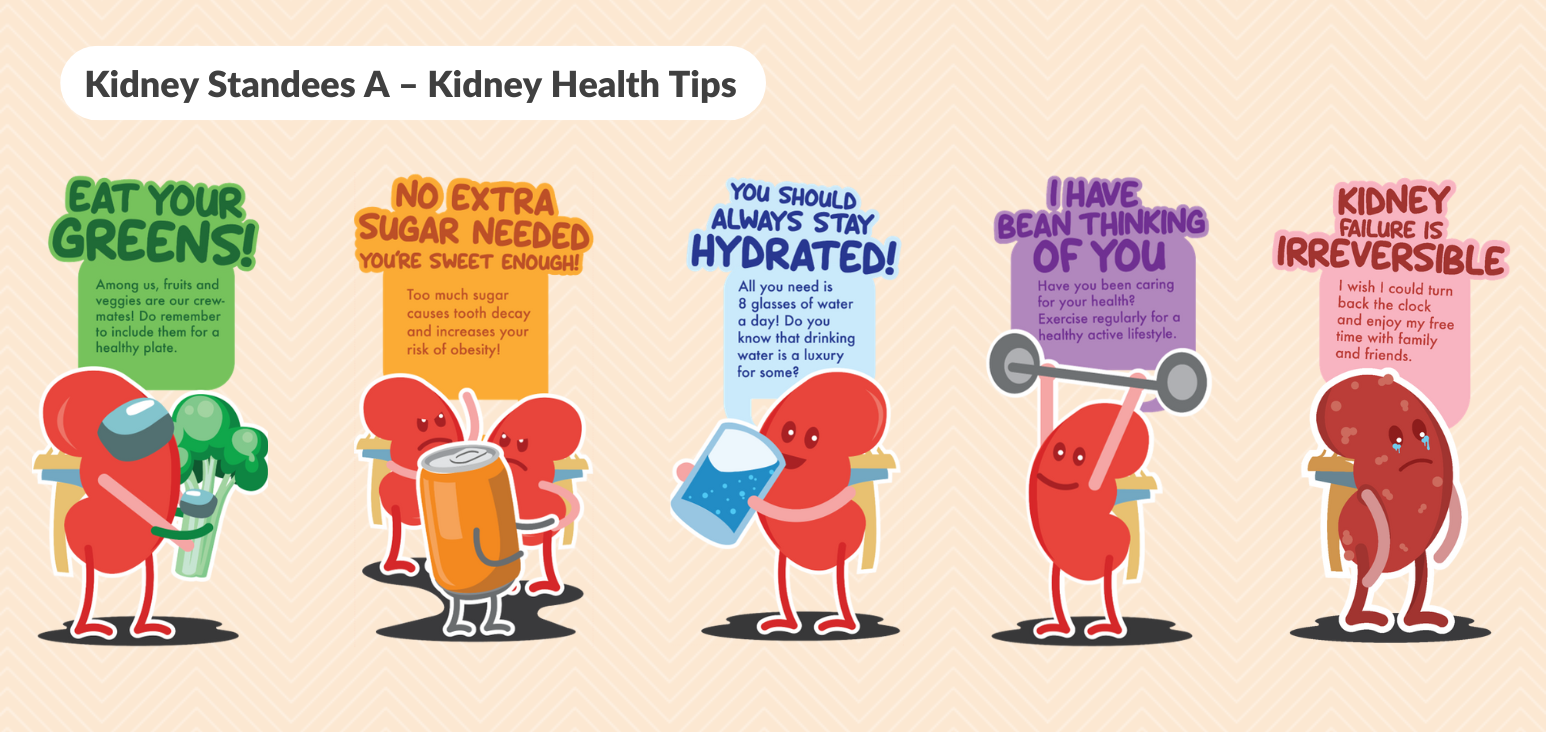
- Diet: A heart-healthy diet low in sodium, saturated fat, and cholesterol is important for both heart and kidney health. Patients with kidney disease may also need to limit their intake of potassium and phosphorus.
- Exercise: Regular physical activity can improve cardiovascular health and help control blood pressure and blood sugar levels.
- Smoking Cessation: Smoking is a major risk factor for both heart disease and kidney disease, so quitting smoking is essential.
- Weight Management: Maintaining a healthy weight can reduce the risk of both heart disease and kidney disease.
-
Medications:
- Blood Pressure Medications: Medications to lower blood pressure, such as ACE inhibitors, ARBs, and beta-blockers, are important for both heart and kidney health.
- Cholesterol-Lowering Medications: Statins can lower cholesterol levels and reduce the risk of heart attacks and strokes.
- Diuretics: Diuretics can help reduce fluid overload in patients with heart failure or kidney disease.
- Antiplatelet Medications: Aspirin or other antiplatelet medications can help prevent blood clots and reduce the risk of heart attacks and strokes.
- Erythropoiesis-Stimulating Agents (ESAs): ESAs can help treat anemia in patients with kidney disease.
-
Renal Replacement Therapy:
- Patients with end-stage kidney disease may require renal replacement therapy, such as dialysis or kidney transplantation. Dialysis filters the blood to remove waste products and excess fluid, while kidney transplantation replaces the damaged kidney with a healthy one.
-
Cardiac Interventions:
- Patients with heart disease may require cardiac interventions, such as angioplasty or bypass surgery, to improve blood flow to the heart.
Prevention Strategies
Preventing both heart disease and kidney disease is crucial for improving overall health and reducing the burden on healthcare systems. Prevention strategies include:
-
Controlling Risk Factors:
- Managing diabetes, hypertension, and high cholesterol levels can reduce the risk of both heart disease and kidney disease.
-
Promoting Healthy Lifestyle:
- Encouraging a heart-healthy diet, regular physical activity, smoking cessation, and weight management can help prevent both conditions.
-
Early Detection:
- Screening for kidney disease in high-risk individuals, such as those with diabetes or hypertension, can help detect kidney damage early and allow for timely intervention.
Conclusion
The intersection between heart disease and kidney health is complex and multifaceted. The cardio-renal connection highlights the importance of considering the health of both organs when managing patients with either condition. Early diagnosis, comprehensive management strategies, and a focus on prevention are essential for improving outcomes and reducing the burden of these two major global health challenges. By addressing shared risk factors and promoting a healthy lifestyle, we can work towards preventing both heart disease and kidney disease and improving the overall health and well-being of individuals worldwide.







Leave a Reply