“Gender Disparities in Chronic Disease Diagnosis and Treatment – Part 8: Addressing the Systemic Barriers to Equitable Care
Related Articles Gender Disparities in Chronic Disease Diagnosis and Treatment – Part 8: Addressing the Systemic Barriers to Equitable Care
- Long-Term Effects Of Chronic Illness On Children
- Financial Challenges Of Living With Chronic Illness – Part 4: Navigating The System And Building Resilience
- Social Determinants Of Health And Chronic Disease Outcomes
- Palliative Care And Quality Of Life For Chronic Illness Patients – Part 3
- Integrative Care Models For Complex Chronic Diseases
Introduction
We will be happy to explore interesting topics related to Gender Disparities in Chronic Disease Diagnosis and Treatment – Part 8: Addressing the Systemic Barriers to Equitable Care. Let’s knit interesting information and provide new insights to readers.
Table of Content
Gender Disparities in Chronic Disease Diagnosis and Treatment – Part 8: Addressing the Systemic Barriers to Equitable Care

The preceding installments of this series have illuminated the pervasive and multifaceted nature of gender disparities in the diagnosis and treatment of chronic diseases. We have explored how biological differences, social determinants of health, implicit biases within the healthcare system, and research gaps contribute to these inequities. While recognizing the complexity of these issues is crucial, it is equally important to focus on actionable strategies to dismantle the systemic barriers that perpetuate these disparities and pave the way for more equitable healthcare for all.
This concluding part of the series will delve into potential solutions and policy recommendations aimed at addressing the root causes of gender disparities in chronic disease management. We will examine strategies that target healthcare providers, researchers, policymakers, and the broader community to create a more inclusive and responsive healthcare system.
1. Enhancing Education and Awareness for Healthcare Professionals
A critical step towards mitigating gender disparities is to equip healthcare professionals with the knowledge and tools to recognize and address potential biases in their clinical practice. This involves:
-
Integrating Gender-Specific Medicine into Medical Education: Medical school curricula should incorporate comprehensive training on sex and gender differences in disease presentation, progression, and response to treatment. This will enable future physicians to approach patient care with a more nuanced understanding of how gender influences health outcomes.
-
Continuing Medical Education (CME) on Gender Bias: Regular CME programs should be offered to practicing physicians, nurses, and other healthcare professionals to raise awareness of implicit biases and their impact on clinical decision-making. These programs should provide strategies for identifying and mitigating these biases, such as using standardized assessment tools and engaging in reflective practice.
-
Promoting Gender-Sensitive Communication Skills: Effective communication is essential for building trust and rapport with patients. Healthcare professionals should be trained in gender-sensitive communication techniques that acknowledge and respect patients’ individual experiences and perspectives. This includes actively listening to patients’ concerns, avoiding assumptions based on gender stereotypes, and providing clear and concise explanations of diagnoses and treatment options.
2. Addressing Bias in Clinical Guidelines and Research
Clinical guidelines and research protocols often fail to adequately consider sex and gender differences, leading to suboptimal care for both men and women. To address this, we need to:
-
Incorporate Sex and Gender into Research Design: Researchers should be required to include both men and women in clinical trials and to analyze data separately by sex. This will help to identify potential sex-specific effects of treatments and interventions.
-
Develop Gender-Specific Clinical Guidelines: Clinical guidelines should be developed that take into account sex and gender differences in disease presentation, risk factors, and treatment response. These guidelines should be regularly updated to reflect the latest scientific evidence.
-
Promote Research on Women’s Health: Increased funding should be allocated to research on women’s health issues, particularly those that are understudied or neglected. This includes research on conditions such as endometriosis, polycystic ovary syndrome (PCOS), and menopause.
3. Empowering Patients Through Education and Advocacy
Patients play a crucial role in advocating for their own health and ensuring that they receive appropriate and equitable care. To empower patients, we need to:
-
Provide Access to Reliable Health Information: Patients should have access to accurate and reliable information about chronic diseases, including information on sex and gender differences. This information should be available in multiple languages and formats to ensure that it is accessible to all.
-
Encourage Patient Advocacy: Patients should be encouraged to advocate for themselves and to ask questions about their care. This includes seeking second opinions, participating in clinical trials, and joining patient advocacy groups.
-
Promote Shared Decision-Making: Healthcare professionals should engage in shared decision-making with patients, taking into account their individual preferences and values. This will help to ensure that patients are actively involved in their own care and that their voices are heard.
4. Policy and Systemic Changes
Addressing gender disparities in chronic disease requires policy changes and systemic reforms. Key areas to focus on include:
-
Insurance Coverage: Advocate for insurance coverage that is equitable and comprehensive, covering preventive services, diagnostic tests, and treatments that are specific to the needs of both men and women. Ensure that coverage decisions are based on scientific evidence and not on gender stereotypes.
-
Healthcare Access: Improve access to healthcare services in underserved communities, addressing barriers such as transportation, childcare, and language. Telehealth and mobile health clinics can be valuable tools for reaching patients in remote or underserved areas.
-
Data Collection and Monitoring: Implement standardized data collection and monitoring systems that track health outcomes by sex and gender. This will allow us to identify disparities and to measure the effectiveness of interventions aimed at reducing them.
-
Workplace Policies: Promote workplace policies that support the health and well-being of employees, such as paid sick leave, flexible work arrangements, and access to employee assistance programs. These policies can help to reduce stress and improve overall health.
5. Community Engagement and Partnerships
Addressing gender disparities requires a collaborative approach that involves healthcare providers, researchers, policymakers, community organizations, and patients. Key strategies include:
-
Community-Based Programs: Develop and implement community-based programs that address the social determinants of health and promote healthy behaviors. These programs should be tailored to the specific needs of the community and should involve community members in the planning and implementation process.
-
Partnerships with Community Organizations: Partner with community organizations to reach underserved populations and to provide culturally appropriate health education and services. These partnerships can help to build trust and to overcome barriers to care.
-
Public Awareness Campaigns: Launch public awareness campaigns to educate the public about gender disparities in chronic disease and to promote healthy behaviors. These campaigns should be targeted to specific populations and should use a variety of communication channels.
6. Addressing the Intersectionality of Gender with Other Social Determinants of Health
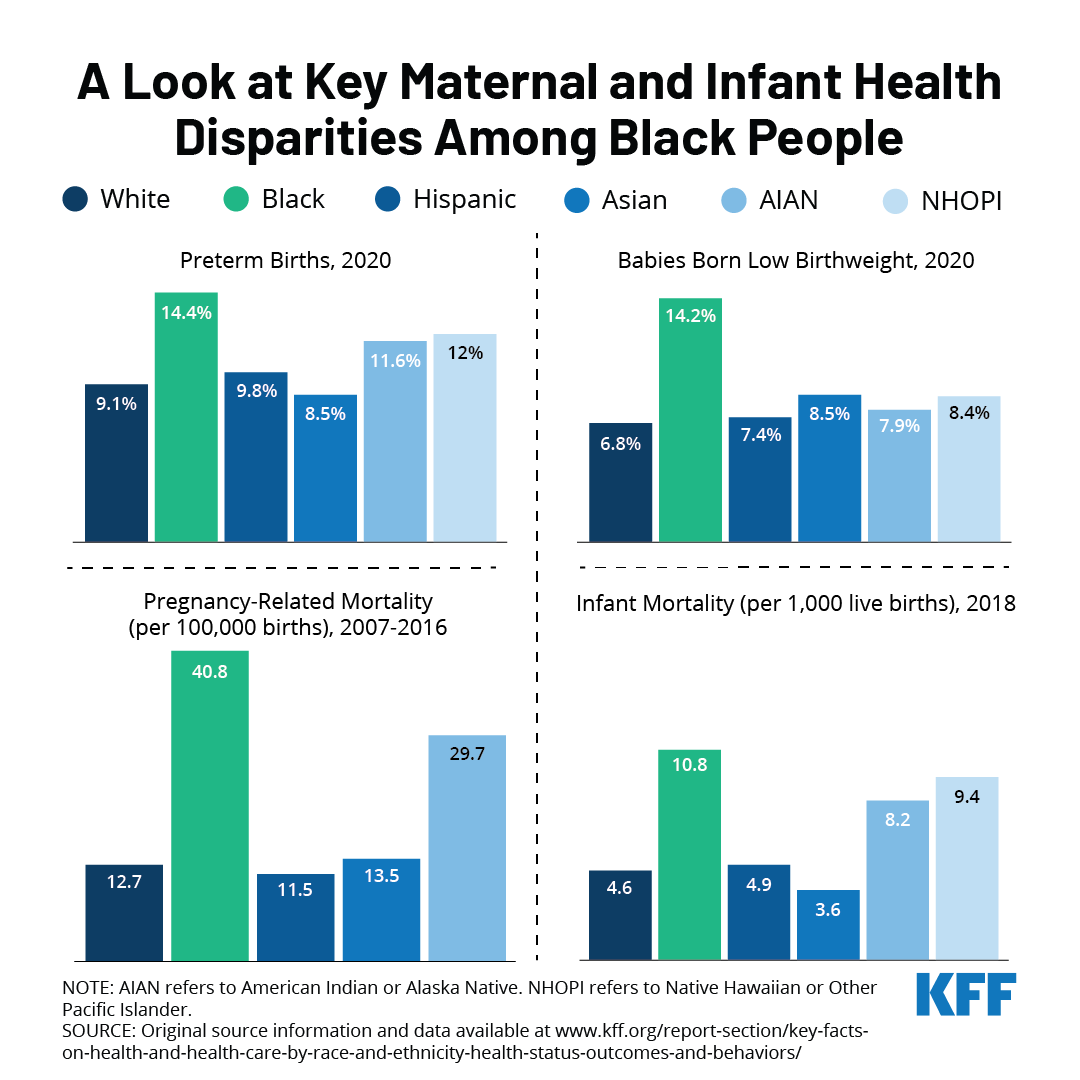
It’s crucial to recognize that gender disparities often intersect with other social determinants of health, such as race, ethnicity, socioeconomic status, sexual orientation, and disability. Women from marginalized communities may face multiple layers of discrimination and disadvantage, leading to even greater health disparities.
-
Targeted Interventions: Develop targeted interventions that address the specific needs of women from marginalized communities. These interventions should be culturally appropriate and should take into account the unique challenges faced by these women.
-
Addressing Systemic Racism and Discrimination: Actively work to dismantle systemic racism and discrimination within the healthcare system and in society as a whole. This includes addressing bias in hiring and promotion practices, promoting diversity in leadership positions, and advocating for policies that promote racial and social justice.
Conclusion
Addressing gender disparities in chronic disease diagnosis and treatment is a complex and multifaceted challenge, but it is one that we must address if we are to achieve health equity for all. By implementing the strategies outlined in this series, we can create a healthcare system that is more responsive to the needs of both men and women and that provides equitable care for all. This requires a concerted effort from healthcare providers, researchers, policymakers, and the broader community. It demands a commitment to challenging ingrained biases, promoting gender-sensitive research and clinical practice, empowering patients, and advocating for policy changes that support equitable access to care.
Ultimately, addressing gender disparities in chronic disease is not just about improving the health of women; it is about creating a more just and equitable society for all. It’s about recognizing that health is a fundamental human right and that everyone deserves the opportunity to live a healthy and fulfilling life, regardless of their gender. By working together, we can create a future where gender is no longer a barrier to optimal health and well-being.







Leave a Reply