“Environmental Factors and Chronic Disease Risk – Part 6: The Interplay of Environment and Genetics in Disease Etiology
Related Articles Environmental Factors and Chronic Disease Risk – Part 6: The Interplay of Environment and Genetics in Disease Etiology
- Educational Interventions For Chronic Disease Prevention – Part 5: Leveraging Technology And Digital Health Platforms
- Exercise And Physical Activity Guidelines For Chronic Illness Management – Part 4
- Genetic Testing And Personalized Medicine In Chronic Diseases: A New Era Of Healthcare
- The Role Of Stress In Chronic Disease Progression – Part 4: Specific Diseases, Coping Strategies, And Future Directions
- Emerging Therapies For Managing Chronic Conditions: A New Dawn Of Hope
Introduction
With great enthusiasm, let’s explore interesting topics related to Environmental Factors and Chronic Disease Risk – Part 6: The Interplay of Environment and Genetics in Disease Etiology. Let’s knit interesting information and provide new insights to readers.
Table of Content
Environmental Factors and Chronic Disease Risk – Part 6: The Interplay of Environment and Genetics in Disease Etiology
The chronic disease landscape is a complex tapestry woven with threads of genetics, lifestyle, and environmental exposures. While genetics provide the blueprint, the environment acts as the master weaver, shaping the expression of those genes and influencing the trajectory of health or disease. This intricate dance between nature and nurture is particularly evident in the development of chronic diseases, where environmental factors can act as both triggers and modifiers of genetic predispositions. This article, the sixth in our series, delves into the fascinating interplay of environment and genetics in disease etiology, exploring how environmental exposures can influence gene expression, alter disease susceptibility, and ultimately contribute to the development of chronic conditions.
Epigenetics: Bridging the Gap Between Genes and Environment
Epigenetics is a field of study that examines how environmental factors can alter gene expression without changing the underlying DNA sequence. These epigenetic modifications, such as DNA methylation, histone modification, and non-coding RNA regulation, can influence which genes are turned on or off, thereby affecting cellular function and disease susceptibility.
Environmental exposures, including diet, pollutants, stress, and infections, can induce epigenetic changes that persist throughout life and even be passed down to future generations. For instance, studies have shown that exposure to air pollution can lead to DNA methylation changes in genes involved in immune function and inflammation, increasing the risk of respiratory diseases and cardiovascular problems. Similarly, maternal diet during pregnancy can influence the epigenetic landscape of the offspring, affecting their risk of obesity, diabetes, and other metabolic disorders later in life.
Gene-Environment Interactions: A Complex Equation
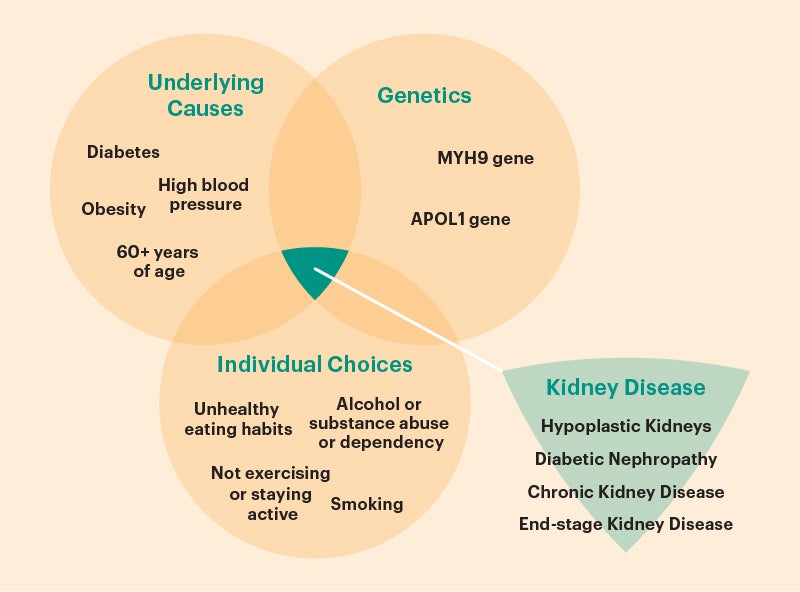
Gene-environment interactions (GxE) occur when the effect of a genetic variant on disease risk differs depending on the level of environmental exposure. In other words, certain genetic predispositions may only manifest as disease in the presence of specific environmental triggers.
For example, individuals with a genetic variant that increases their susceptibility to lung cancer may only develop the disease if they are exposed to cigarette smoke or other air pollutants. Conversely, individuals without the genetic variant may be less likely to develop lung cancer even if they are exposed to the same environmental hazards.
GxE interactions are complex and can be difficult to identify, as they require large-scale studies with detailed information on both genetic and environmental factors. However, understanding these interactions is crucial for developing targeted prevention strategies that address the specific needs of individuals with different genetic backgrounds and environmental exposures.
Examples of Gene-Environment Interactions in Chronic Diseases
- Cardiovascular Disease: Genetic factors play a significant role in determining an individual’s risk of cardiovascular disease (CVD). However, environmental factors such as diet, smoking, and physical activity can significantly modify this risk. For example, individuals with a genetic predisposition to high cholesterol may be able to reduce their risk of CVD by adopting a healthy diet and exercise regimen. Conversely, individuals with a lower genetic risk may still develop CVD if they consume a diet high in saturated fat and cholesterol and lead a sedentary lifestyle.
- Type 2 Diabetes: Type 2 diabetes is a complex disease influenced by both genetic and environmental factors. Genetic variants that affect insulin secretion, insulin sensitivity, and glucose metabolism can increase an individual’s risk of developing the disease. However, environmental factors such as obesity, physical inactivity, and a diet high in processed foods and sugary drinks can significantly exacerbate this risk. Studies have shown that individuals with a genetic predisposition to type 2 diabetes can reduce their risk by maintaining a healthy weight, engaging in regular physical activity, and consuming a balanced diet.
- Asthma: Asthma is a chronic respiratory disease characterized by airway inflammation and bronchoconstriction. Genetic factors play a role in determining an individual’s susceptibility to asthma, but environmental factors such as allergens, air pollution, and respiratory infections can trigger asthma attacks and worsen symptoms. For example, individuals with a genetic predisposition to asthma may only develop the disease if they are exposed to high levels of allergens or air pollutants. Conversely, individuals without the genetic predisposition may be less likely to develop asthma even if they are exposed to the same environmental triggers.
- Cancer: Cancer is a complex disease characterized by uncontrolled cell growth and the potential to spread to other parts of the body. Genetic factors play a role in determining an individual’s risk of developing cancer, but environmental factors such as tobacco smoke, radiation, and certain chemicals can significantly increase this risk. For example, individuals with a genetic predisposition to breast cancer may be able to reduce their risk by maintaining a healthy weight, engaging in regular physical activity, and avoiding exposure to environmental toxins.
- Neurodegenerative Diseases: Neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease, are characterized by the progressive loss of neurons in the brain. Genetic factors play a role in determining an individual’s risk of developing these diseases, but environmental factors such as exposure to pesticides, heavy metals, and air pollution may also contribute. Studies have shown that individuals with a genetic predisposition to Alzheimer’s disease may be able to delay the onset of the disease by maintaining a healthy lifestyle, engaging in cognitive activities, and avoiding exposure to environmental toxins.
Implications for Public Health and Prevention
Understanding the interplay of environment and genetics in disease etiology has significant implications for public health and prevention. By identifying specific gene-environment interactions, we can develop targeted interventions that address the unique needs of individuals with different genetic backgrounds and environmental exposures.
For example, individuals with a genetic predisposition to lung cancer may benefit from smoking cessation programs and efforts to reduce air pollution in their communities. Similarly, individuals with a genetic predisposition to type 2 diabetes may benefit from personalized dietary and exercise recommendations.
In addition, public health initiatives can focus on creating healthier environments that reduce the risk of chronic diseases for everyone, regardless of their genetic background. This includes efforts to reduce air and water pollution, promote healthy diets and physical activity, and create safer and more supportive communities.
Challenges and Future Directions
Despite the progress made in understanding the interplay of environment and genetics in disease etiology, there are still many challenges to overcome. One of the biggest challenges is the complexity of GxE interactions, which can be difficult to identify and characterize.
Another challenge is the lack of comprehensive data on both genetic and environmental factors. Large-scale studies are needed to collect detailed information on both genetic variants and environmental exposures in diverse populations.
In the future, advances in genomics, epigenetics, and environmental science will provide new tools and insights for understanding the interplay of environment and genetics in disease etiology. This will lead to the development of more effective prevention strategies and personalized treatments for chronic diseases.
Conclusion
The interplay of environment and genetics is a critical factor in the development of chronic diseases. Environmental exposures can influence gene expression, alter disease susceptibility, and ultimately contribute to the development of chronic conditions. By understanding the complex interactions between genes and the environment, we can develop targeted prevention strategies and personalized treatments that address the unique needs of individuals with different genetic backgrounds and environmental exposures. This knowledge is crucial for improving public health and reducing the burden of chronic diseases.







Leave a Reply