“Endocarditis: Infection of the Heart’s Inner LiningEndocarditis: Infection of the Heart’s Inner Lining
Related Articles Endocarditis: Infection of the Heart’s Inner LiningEndocarditis: Infection of the Heart’s Inner Lining
- The Role Of Genetics In Chronic Disease Development – Part 2
- Swimming And Its Benefits For The Heart
- Medical Advances In Treating Rare Chronic Conditions – Part 7
- Ethical Considerations In Chronic Disease Research
- Integrating Palliative Care Into Leukemia Treatment Plans
Introduction
We will be happy to explore interesting topics related to Endocarditis: Infection of the Heart’s Inner LiningEndocarditis: Infection of the Heart’s Inner Lining. Let’s knit interesting information and provide new insights to readers.
Table of Content
Okay, here’s a comprehensive article on Endocarditis, targeting around 1600 words. I’ve aimed for clarity, accuracy, and a good balance of information for a general audience while still including some more technical details.
Endocarditis: Infection of the Heart’s Inner Lining
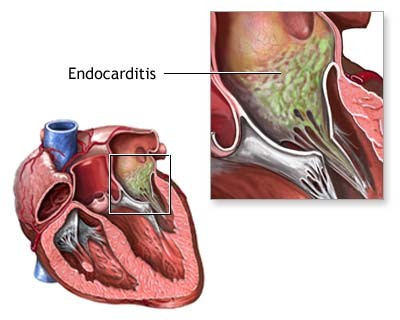
Endocarditis is a relatively rare but serious infection of the endocardium, the inner lining of the heart chambers and heart valves. This lining, normally smooth and protective, can become a target for bacteria, fungi, or other germs that enter the bloodstream and travel to the heart. When these microorganisms colonize the endocardium, they can form vegetations – clumps of infectious material and cellular debris – that damage the heart valves, disrupt normal heart function, and potentially spread infection to other parts of the body.
Understanding the Heart’s Vulnerability
The heart, a vital organ responsible for pumping blood throughout the body, is usually well-protected from infection. However, certain conditions and procedures can increase the risk of developing endocarditis. These factors typically involve creating a pathway for microorganisms to enter the bloodstream and adhere to the endocardium.
Causes and Risk Factors:
-
Bacterial Infections: The most common cause of endocarditis is bacterial infection. Bacteria such as Staphylococcus aureus, Streptococcus viridans, Enterococcus, and others can enter the bloodstream through various routes.
-
Poor Dental Hygiene: Bacteria in the mouth can enter the bloodstream during routine activities like brushing or flossing, especially if gum disease is present. Dental procedures, such as extractions or deep cleanings, can also temporarily increase the risk.
-
Intravenous (IV) Drug Use: Injecting drugs directly into the veins bypasses the body’s natural defenses, significantly increasing the risk of introducing bacteria into the bloodstream. Staphylococcus aureus is a particularly common culprit in these cases.
-
Central Venous Catheters: These catheters, used for delivering medications or fluids directly into a large vein, can become a source of infection if not properly inserted and maintained.
-
Heart Valve Abnormalities: Damaged or artificial heart valves are more susceptible to infection than healthy valves. Conditions like rheumatic heart disease, congenital heart defects, and valve stenosis or regurgitation create turbulent blood flow, making it easier for bacteria to adhere to the endocardium.
-
Prosthetic Heart Valves: Artificial valves, while life-saving, are foreign materials that can provide a surface for bacteria to attach and form vegetations. The risk of endocarditis is highest in the first year after valve replacement.
-
Pacemakers and Implantable Defibrillators: Similar to prosthetic valves, these devices can also serve as a site for infection.
-
Certain Medical Procedures: Invasive procedures, such as colonoscopies or cystoscopies, can sometimes introduce bacteria into the bloodstream, although the risk is generally low.
-
Weakened Immune System: Conditions like HIV/AIDS, cancer, or immunosuppressant medications can weaken the body’s defenses, making it harder to fight off infections.
Symptoms of Endocarditis:
The symptoms of endocarditis can vary depending on the severity of the infection, the specific microorganism involved, and the individual’s overall health. Symptoms can develop gradually over weeks or months (subacute endocarditis) or appear suddenly and severely (acute endocarditis).
Common symptoms include:
- Fever: A persistent fever, often accompanied by chills, is one of the most common signs.
- Fatigue and Weakness: Feeling unusually tired and weak is a frequent complaint.
- Night Sweats: Excessive sweating during the night.
- Muscle and Joint Pain: Aches and pains in the muscles and joints.
- Shortness of Breath: Difficulty breathing, especially during exertion.
- Cough: A persistent cough, sometimes producing blood-tinged sputum.
- New or Changed Heart Murmur: A heart murmur is an abnormal sound heard during a heartbeat. Endocarditis can damage the heart valves, leading to a new murmur or a change in an existing one.
- Skin Changes:
- Petechiae: Small, pinpoint-sized red or purple spots on the skin, whites of the eyes, or inside the mouth.
- Splinter Hemorrhages: Thin, dark lines under the fingernails or toenails.
- Osler’s Nodes: Small, painful, red or purple bumps on the fingers or toes.
- Janeway Lesions: Flat, painless, red spots on the palms of the hands or soles of the feet.
- Swelling in the Legs, Ankles, or Feet: Fluid retention due to heart failure.
- Weight Loss: Unexplained weight loss.
- Neurological Symptoms: In some cases, endocarditis can cause neurological symptoms such as headache, stroke, seizures, or changes in mental status if vegetations break off and travel to the brain.
Diagnosis of Endocarditis:
Diagnosing endocarditis typically involves a combination of physical examination, blood tests, and imaging studies.
-
Physical Examination: A doctor will listen to the heart for murmurs, check for skin changes, and assess the patient’s overall condition.
-
Blood Cultures: Blood samples are taken to identify the specific microorganism causing the infection. Multiple blood cultures are usually performed to increase the chances of detecting the bacteria.
-
Echocardiogram: This ultrasound of the heart provides detailed images of the heart valves and chambers. It can help detect vegetations, assess valve function, and identify any structural abnormalities. There are two main types:
- Transthoracic Echocardiogram (TTE): The ultrasound probe is placed on the chest.
- Transesophageal Echocardiogram (TEE): The probe is inserted into the esophagus, providing a clearer image of the heart, especially the valves. TEE is more sensitive for detecting vegetations, particularly on prosthetic valves.
-
Electrocardiogram (ECG or EKG): This test measures the electrical activity of the heart and can help detect arrhythmias or other heart problems.
-
Chest X-ray: This can help assess the size and shape of the heart and lungs and identify any signs of heart failure or pneumonia.
-
Complete Blood Count (CBC): This blood test can reveal signs of infection, such as an elevated white blood cell count.
-
Inflammatory Markers: Tests like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) can measure inflammation in the body.
Treatment of Endocarditis:
The primary treatment for endocarditis is a prolonged course of antibiotics or antifungals, administered intravenously (IV) for several weeks. In some cases, surgery may be necessary to repair or replace damaged heart valves or to remove large vegetations.
-
Antibiotics or Antifungals: The specific medication used depends on the type of microorganism identified in the blood cultures. Treatment typically lasts for 4-6 weeks or longer. Patients usually require hospitalization for IV antibiotic administration.
-
Surgery: Surgery may be recommended in the following situations:
- Severe Valve Damage: If the heart valves are severely damaged and causing heart failure.
- Large Vegetations: Large vegetations that are at risk of breaking off and causing emboli (blood clots that travel to other parts of the body).
- Persistent Infection: If the infection does not respond to antibiotics alone.
- Abscess Formation: If an abscess (a collection of pus) has formed in the heart.
- Prosthetic Valve Endocarditis: Prosthetic valve endocarditis often requires surgery, especially if the infection is difficult to control with antibiotics.
Complications of Endocarditis:
Endocarditis can lead to a number of serious complications, including:
- Heart Failure: Damage to the heart valves can lead to heart failure, a condition in which the heart cannot pump enough blood to meet the body’s needs.
- Stroke: Vegetations can break off and travel to the brain, causing a stroke.
- Emboli to Other Organs: Emboli can also travel to other organs, such as the lungs, kidneys, or spleen, causing damage or infection.
- Valve Stenosis or Regurgitation: Endocarditis can cause the heart valves to become narrowed (stenosis) or leaky (regurgitation).
- Myocardial Abscess: A collection of pus can form in the heart muscle.
- Arrhythmias: Irregular heart rhythms.
- Kidney Damage: Inflammation and immune complex deposition can damage the kidneys.
- Death: If left untreated, endocarditis can be fatal.
Prevention of Endocarditis:
Preventing endocarditis involves reducing the risk of bacteria entering the bloodstream and adhering to the heart valves.
-
Good Oral Hygiene: Regular brushing, flossing, and dental checkups are essential for preventing gum disease.
-
Antibiotic Prophylaxis: Antibiotics are recommended before certain dental or medical procedures for individuals at high risk of endocarditis, such as those with prosthetic heart valves, a history of endocarditis, certain congenital heart defects, or a heart transplant with valve abnormalities. The guidelines for antibiotic prophylaxis have become more restrictive in recent years, so it’s important to discuss your individual risk with your doctor or dentist.
-
Avoiding IV Drug Use: Avoiding the injection of illicit drugs is crucial.
-
Proper Catheter Care: Ensuring proper insertion and maintenance of central venous catheters.
-
Prompt Treatment of Infections: Treating any infections promptly to prevent them from spreading to the bloodstream.
-
Patient Education: Educating patients at risk about the signs and symptoms of endocarditis and the importance of seeking prompt medical attention.
Living with Endocarditis:
After treatment for endocarditis, regular follow-up appointments with a cardiologist are essential to monitor heart function and detect any complications. Patients may need to take lifelong antibiotics to prevent recurrent infections. Maintaining good oral hygiene and avoiding risk factors are also crucial for preventing future episodes of endocarditis.
Conclusion:
Endocarditis is a serious infection that can have devastating consequences if left untreated. Early diagnosis and prompt treatment with antibiotics or surgery are essential for improving outcomes. Individuals at high risk should take preventive measures, such as maintaining good oral hygiene and discussing antibiotic prophylaxis with their doctor or dentist. Increased awareness of the signs and symptoms of endocarditis can help ensure timely medical intervention and improve the chances of a full recovery. By understanding the causes, symptoms, and prevention strategies, we can work towards reducing the incidence and impact of this life-threatening condition.








Leave a Reply