“Eisenmenger Syndrome: A Rare Heart-Lung Disorder
Related Articles Eisenmenger Syndrome: A Rare Heart-Lung Disorder
- Social Support Networks For Chronic Disease Patients – Part 2
- Innovative Therapies For Acute Lymphoblastic Leukemia (ALL)
- Telemedicine And Remote Monitoring For Chronic Illness Care – Part 6: Future Trends, Challenges, And The Path Forward
- Technology’s Role In Chronic Disease Self-Management – Part 5: The Future Of Connected Care And Personalized Health
- Psychological Resilience In Chronic Disease Patients: Navigating Challenges And Fostering Well-being
Introduction
On this special occasion, we are happy to review interesting topics related to Eisenmenger Syndrome: A Rare Heart-Lung Disorder. Let’s knit interesting information and provide new insights to readers.
Table of Content
Eisenmenger Syndrome: A Rare Heart-Lung Disorder

Eisenmenger syndrome is a severe and complex condition that affects the heart and lungs. It is a rare but life-threatening complication of congenital heart defects that are not corrected early in life. This syndrome leads to irreversible pulmonary hypertension and a reversal of blood flow in the heart, causing deoxygenated blood to circulate throughout the body. Understanding the causes, symptoms, diagnosis, and management of Eisenmenger syndrome is crucial for improving the quality of life and prognosis for affected individuals.
Definition and Background
Eisenmenger syndrome is defined as a condition in which a congenital heart defect, typically a large hole between the heart’s chambers (such as a ventricular septal defect or atrial septal defect), causes increased blood flow to the lungs. Over time, this excessive blood flow leads to pulmonary hypertension, a condition where the blood pressure in the pulmonary arteries becomes abnormally high. As the pulmonary hypertension worsens, it eventually exceeds the systemic blood pressure, causing a reversal of blood flow through the original heart defect. This reversal results in deoxygenated blood entering the systemic circulation, leading to cyanosis (a bluish discoloration of the skin and mucous membranes) and other complications.
The syndrome is named after Dr. Victor Eisenmenger, an Austrian physician who first described the condition in 1897. He observed the characteristic features of the syndrome in a patient with a ventricular septal defect and pulmonary hypertension.
Causes and Risk Factors
Eisenmenger syndrome is primarily caused by uncorrected congenital heart defects that lead to increased pulmonary blood flow. The most common heart defects associated with Eisenmenger syndrome include:
- Ventricular Septal Defect (VSD): A hole in the wall separating the two ventricles of the heart.
- Atrial Septal Defect (ASD): A hole in the wall separating the two atria of the heart.
- Patent Ductus Arteriosus (PDA): A persistent opening between the aorta and the pulmonary artery.
- Atrioventricular Canal Defect (AV Canal Defect): A complex defect involving the atria, ventricles, and valves of the heart.
These defects, if left untreated, result in excessive blood flow to the lungs. The increased blood flow damages the pulmonary blood vessels, causing them to narrow and stiffen. This leads to pulmonary hypertension, which eventually progresses to Eisenmenger syndrome.
Several factors can increase the risk of developing Eisenmenger syndrome:
- Delayed or Lack of Surgical Correction: The primary risk factor is the failure to surgically correct the underlying congenital heart defect in early childhood.
- Size of the Heart Defect: Larger defects are more likely to cause significant pulmonary blood flow and lead to pulmonary hypertension.
- Genetic Predisposition: In some cases, genetic factors may play a role in the development of Eisenmenger syndrome.
- Environmental Factors: Exposure to certain environmental factors during pregnancy may increase the risk of congenital heart defects.
Pathophysiology
The pathophysiology of Eisenmenger syndrome involves a series of progressive changes in the pulmonary vasculature and cardiac function. The key steps in the development of the syndrome include:
- Increased Pulmonary Blood Flow: The congenital heart defect allows a significant amount of blood to flow from the left side of the heart to the right side and into the pulmonary arteries.
- Pulmonary Vascular Remodeling: The increased blood flow causes damage to the endothelial cells lining the pulmonary arteries. This leads to inflammation, proliferation of smooth muscle cells, and deposition of extracellular matrix, resulting in pulmonary vascular remodeling.
- Pulmonary Hypertension: The remodeling of the pulmonary blood vessels causes them to narrow and stiffen, increasing the resistance to blood flow. This leads to pulmonary hypertension, where the blood pressure in the pulmonary arteries becomes abnormally high.
- Reversal of Blood Flow: As the pulmonary hypertension worsens, the pressure in the pulmonary arteries eventually exceeds the pressure in the systemic circulation. This causes a reversal of blood flow through the original heart defect, with deoxygenated blood flowing from the right side of the heart to the left side and into the systemic circulation.
- Cyanosis and Hypoxemia: The mixing of deoxygenated blood into the systemic circulation leads to cyanosis, a bluish discoloration of the skin and mucous membranes. It also results in hypoxemia, a condition where the blood has a low level of oxygen.
- Compensatory Mechanisms: The body attempts to compensate for the hypoxemia by increasing red blood cell production (polycythemia) and increasing cardiac output. However, these compensatory mechanisms eventually fail, leading to further complications.
Symptoms
The symptoms of Eisenmenger syndrome can vary depending on the severity of the condition and the individual’s overall health. Common symptoms include:
- Cyanosis: Bluish discoloration of the skin, lips, and nail beds due to low oxygen levels in the blood.
- Shortness of Breath (Dyspnea): Difficulty breathing, especially during exertion.
- Fatigue: Feeling tired and weak, even after rest.
- Chest Pain: Discomfort or pain in the chest, often associated with exertion.
- Dizziness or Fainting (Syncope): Lightheadedness or loss of consciousness due to decreased blood flow to the brain.
- Palpitations: Awareness of rapid or irregular heartbeats.
- Edema: Swelling in the ankles, legs, or abdomen due to fluid retention.
- Cough: Persistent cough, sometimes with blood (hemoptysis).
- Clubbing of Fingers and Toes: Enlargement and rounding of the fingertips and toes due to chronic hypoxemia.
- Stroke: Blood clot in the brain due to thick blood.
- Arrhythmias: Irregular heart rhythms.
Diagnosis
Diagnosing Eisenmenger syndrome involves a comprehensive evaluation of the patient’s medical history, physical examination, and diagnostic tests. Key diagnostic procedures include:
- Medical History and Physical Examination: The doctor will ask about the patient’s symptoms, medical history, and any known congenital heart defects. A physical examination will assess the patient’s vital signs, heart sounds, lung sounds, and signs of cyanosis or edema.
- Echocardiography: This non-invasive imaging test uses sound waves to create detailed pictures of the heart’s structure and function. Echocardiography can identify heart defects, assess the severity of pulmonary hypertension, and evaluate the direction of blood flow in the heart.
- Electrocardiogram (ECG): This test records the electrical activity of the heart and can detect arrhythmias or signs of heart enlargement.
- Chest X-Ray: This imaging test can reveal enlargement of the heart and pulmonary arteries.
- Cardiac Catheterization: This invasive procedure involves inserting a catheter into a blood vessel and guiding it to the heart. Cardiac catheterization allows direct measurement of blood pressures in the heart and pulmonary arteries. It is often used to confirm the diagnosis of Eisenmenger syndrome and assess the severity of pulmonary hypertension.
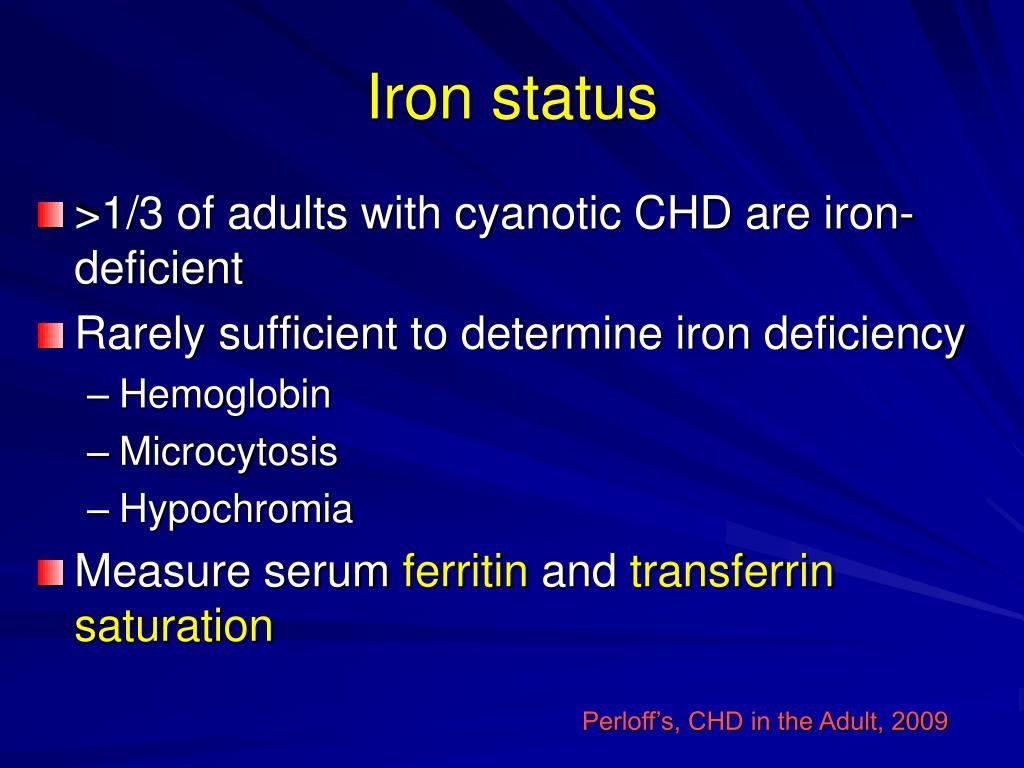
- Blood Tests: Blood tests can assess oxygen levels, red blood cell count (to detect polycythemia), and kidney and liver function.
- Pulmonary Function Tests: These tests measure lung capacity and airflow to assess the impact of pulmonary hypertension on lung function.
- Ventilation-Perfusion Scan (V/Q Scan): This nuclear medicine test assesses blood flow and air flow in the lungs to detect blood clots or other abnormalities.
Treatment and Management
Eisenmenger syndrome is a chronic and progressive condition that requires lifelong management. The primary goals of treatment are to improve symptoms, prevent complications, and prolong survival. Treatment strategies include:
- Medical Management:
- Pulmonary Vasodilators: Medications that relax the blood vessels in the lungs, reducing pulmonary hypertension and improving blood flow. Common pulmonary vasodilators include:
- Endothelin Receptor Antagonists (ERAs): Such as bosentan, ambrisentan, and macitentan.
- Phosphodiesterase-5 (PDE-5) Inhibitors: Such as sildenafil and tadalafil.
- Prostacyclin Analogs: Such as epoprostenol, treprostinil, and iloprost.
- Oxygen Therapy: Supplemental oxygen can help improve blood oxygen levels and reduce symptoms of hypoxemia.
- Diuretics: Medications that help reduce fluid retention and edema.
- Anticoagulants: Blood thinners, such as warfarin, may be used to prevent blood clots and stroke.
- Iron Supplementation: Iron supplements may be needed to treat iron deficiency anemia, which can occur due to chronic blood loss.
- Antibiotics: Prompt treatment of infections is important to prevent complications.
- Pulmonary Vasodilators: Medications that relax the blood vessels in the lungs, reducing pulmonary hypertension and improving blood flow. Common pulmonary vasodilators include:
- Lifestyle Modifications:
- Avoid Strenuous Exercise: Limit physical activity to avoid overexertion and worsening of symptoms.
- Maintain Hydration: Drink plenty of fluids to prevent dehydration and reduce the risk of blood clots.
- Avoid High Altitudes: High altitudes can worsen hypoxemia due to lower oxygen levels in the air.
- Smoking Cessation: Smoking can worsen pulmonary hypertension and should be avoided.
- Vaccinations: Stay up-to-date on vaccinations to prevent infections.
- Surgical Interventions:
- Lung Transplantation: Lung transplantation may be considered for patients with severe Eisenmenger syndrome who are not responding to medical therapy.
- Heart-Lung Transplantation: In rare cases, a combined heart-lung transplant may be necessary.
- Supportive Care:
- Regular Monitoring: Regular follow-up appointments with a cardiologist and pulmonologist are essential to monitor the patient’s condition and adjust treatment as needed.
- Psychological Support: Living with Eisenmenger syndrome can be challenging, and psychological support may be helpful for managing stress, anxiety, and depression.
- Genetic Counseling: Genetic counseling may be recommended for individuals with Eisenmenger syndrome and their families to assess the risk of congenital heart defects in future generations.
Prognosis
The prognosis for individuals with Eisenmenger syndrome varies depending on the severity of the condition, the presence of complications, and the effectiveness of treatment. Without treatment, the median survival is around 30-40 years. However, with advances in medical management, many individuals with Eisenmenger syndrome can live longer and enjoy a better quality of life.
Factors that can affect the prognosis include:
- Severity of Pulmonary Hypertension: More severe pulmonary hypertension is associated with a poorer prognosis.
- Presence of Complications: Complications such as heart failure, arrhythmias, and blood clots can worsen the prognosis.
- Response to Treatment: Individuals who respond well to medical therapy tend to have a better prognosis.
- Adherence to Treatment: Following the recommended treatment plan is crucial for improving outcomes.
Conclusion
Eisenmenger syndrome is a rare but serious heart-lung disorder that results from uncorrected congenital heart defects. Early diagnosis and appropriate management are essential to improve symptoms, prevent complications, and prolong survival. With advances in medical therapy and supportive care, individuals with Eisenmenger syndrome can live longer and enjoy a better quality of life. Regular monitoring, adherence to treatment, and lifestyle modifications are crucial for managing this chronic condition.







Leave a Reply