“Economic Burden of Chronic Illnesses: A Global Perspective
Related Articles Economic Burden of Chronic Illnesses: A Global Perspective
- Innovations In Treating Chronic Diseases
- Lifestyle Changes To Manage Chronic Conditions: A Comprehensive Guide
- Economic Burden Of Chronic Illnesses: A Global Perspective
- Holistic Approaches To Chronic Disease Prevention
- Lifestyle Changes To Manage Chronic Conditions: A Comprehensive Guide
Introduction
We will be happy to explore interesting topics related to Economic Burden of Chronic Illnesses: A Global Perspective. Come on knit interesting information and provide new insights to readers.
Table of Content
Economic Burden of Chronic Illnesses: A Global Perspective
Chronic illnesses, also known as non-communicable diseases (NCDs), are long-lasting health conditions that cannot be cured but can be managed. These conditions, including cardiovascular diseases, cancer, diabetes, chronic respiratory diseases, and mental disorders, pose a significant threat to global health and development. Beyond their impact on individual well-being, chronic illnesses exert a substantial economic burden on individuals, families, healthcare systems, and societies worldwide.
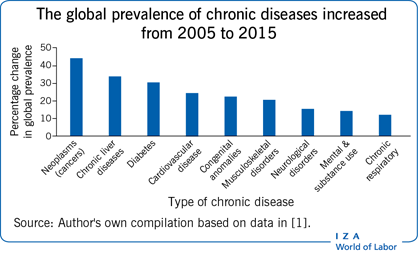
The Global Prevalence of Chronic Illnesses
The prevalence of chronic illnesses is on the rise globally, driven by factors such as aging populations, unhealthy lifestyles, and environmental changes. According to the World Health Organization (WHO), NCDs are responsible for 74% of all deaths worldwide, with the majority occurring in low- and middle-income countries (LMICs). The increasing prevalence of chronic illnesses is placing immense strain on healthcare systems and economies around the world.
Direct Costs of Chronic Illnesses
The direct costs of chronic illnesses encompass the expenses associated with medical care, including doctor visits, hospitalizations, medications, diagnostic tests, and rehabilitation services. These costs can be substantial, especially for individuals with multiple chronic conditions or those requiring long-term care.
- Medical Expenses: Chronic illnesses often necessitate frequent medical consultations, diagnostic procedures, and treatments, leading to significant healthcare expenditures. For instance, individuals with diabetes may require regular blood glucose monitoring, insulin therapy, and foot care, while those with heart disease may need medications, angioplasty, or bypass surgery.
- Hospitalizations: Chronic illnesses are a major driver of hospital admissions, contributing to high healthcare costs. Hospital stays can be prolonged and expensive, particularly for patients with severe complications or those requiring intensive care.
- Medications: Many chronic illnesses require long-term medication management, which can be a significant financial burden for individuals and healthcare systems. The cost of medications can vary widely depending on the specific condition, the type of drug, and the availability of generic alternatives.
- Rehabilitation and Long-Term Care: Chronic illnesses can lead to physical disabilities and functional limitations, requiring rehabilitation services and long-term care. These services can include physical therapy, occupational therapy, speech therapy, and home healthcare, which can be costly and time-consuming.
Indirect Costs of Chronic Illnesses
In addition to direct medical costs, chronic illnesses also incur substantial indirect costs, which include lost productivity, absenteeism, disability, and premature mortality. These costs can have a significant impact on individuals, families, and the economy as a whole.
- Lost Productivity: Chronic illnesses can impair an individual’s ability to work, leading to reduced productivity and lost income. Individuals with chronic conditions may experience fatigue, pain, and other symptoms that interfere with their work performance.
- Absenteeism: Chronic illnesses can cause individuals to miss work due to illness, medical appointments, or hospitalizations. Absenteeism can result in lost wages for employees and reduced productivity for employers.
- Disability: Chronic illnesses can lead to disability, preventing individuals from working altogether. Disability can result in a loss of income, reduced quality of life, and increased reliance on social welfare programs.
- Premature Mortality: Chronic illnesses can shorten an individual’s lifespan, resulting in premature mortality. Premature mortality not only represents a loss of human potential but also has significant economic consequences, including lost productivity and reduced tax revenues.
The Economic Burden on Individuals and Families
Chronic illnesses can place a significant financial burden on individuals and families, especially those with limited resources. The costs of medical care, medications, and long-term care can quickly deplete savings and lead to financial hardship.
- Out-of-Pocket Expenses: Individuals with chronic illnesses often face substantial out-of-pocket expenses for medical care, medications, and other healthcare services. These expenses can be particularly burdensome for those with inadequate health insurance coverage or those living in countries with limited access to healthcare.
- Reduced Income: Chronic illnesses can lead to reduced income due to lost productivity, absenteeism, and disability. This can make it difficult for individuals and families to meet their basic needs, such as housing, food, and transportation.
- Caregiving Costs: Caring for a loved one with a chronic illness can be time-consuming and expensive. Caregivers may need to reduce their work hours or quit their jobs altogether to provide care, resulting in lost income and increased financial strain.
The Economic Burden on Healthcare Systems
Chronic illnesses place a significant strain on healthcare systems worldwide, consuming a large proportion of healthcare resources. The increasing prevalence of chronic illnesses is challenging the capacity of healthcare systems to provide timely and effective care.
- Increased Healthcare Expenditures: Chronic illnesses are a major driver of healthcare expenditures, accounting for a significant portion of national healthcare budgets. The costs of treating chronic illnesses are expected to continue to rise as the population ages and the prevalence of these conditions increases.
- Strain on Healthcare Infrastructure: Chronic illnesses can overwhelm healthcare infrastructure, leading to long wait times, overcrowded hospitals, and shortages of healthcare professionals. This can compromise the quality of care and make it difficult for individuals to access the services they need.
- Need for Integrated Care: Managing chronic illnesses effectively requires integrated care that involves multiple healthcare providers and settings. However, many healthcare systems are fragmented, making it difficult to coordinate care and ensure continuity of treatment.
The Economic Burden on Society
Chronic illnesses have far-reaching economic consequences for society as a whole, affecting economic growth, productivity, and social welfare.
- Reduced Economic Growth: Chronic illnesses can reduce economic growth by lowering productivity, increasing healthcare costs, and reducing labor force participation.
- Increased Social Welfare Costs: Chronic illnesses can increase social welfare costs by increasing the demand for disability benefits, unemployment insurance, and other social safety net programs.
- Inequality: Chronic illnesses can exacerbate existing inequalities, as individuals from disadvantaged backgrounds are more likely to develop chronic conditions and less likely to have access to quality healthcare.
Strategies to Mitigate the Economic Burden of Chronic Illnesses
Addressing the economic burden of chronic illnesses requires a multi-faceted approach that involves prevention, early detection, effective management, and supportive policies.
- Prevention: Preventing chronic illnesses is the most cost-effective way to reduce their economic burden. Prevention strategies include promoting healthy lifestyles, such as regular physical activity, healthy diets, and smoking cessation, as well as addressing environmental risk factors, such as air pollution and exposure to toxins.
- Early Detection: Early detection of chronic illnesses can improve treatment outcomes and reduce healthcare costs. Screening programs can help identify individuals at risk for chronic conditions, allowing for early intervention and management.
- Effective Management: Effective management of chronic illnesses can improve quality of life, reduce complications, and lower healthcare costs. This includes providing access to evidence-based treatments, promoting self-management skills, and coordinating care across different healthcare settings.
- Supportive Policies: Supportive policies can create an environment that promotes health and well-being, reduces health disparities, and supports individuals with chronic illnesses. These policies include:
- Health Insurance Coverage: Ensuring access to affordable health insurance coverage can help individuals afford the medical care they need and prevent financial hardship.
- Access to Healthcare: Expanding access to healthcare services, particularly in underserved communities, can improve health outcomes and reduce healthcare costs.
- Social Support Programs: Providing social support programs, such as disability benefits, unemployment insurance, and caregiver support, can help individuals and families cope with the challenges of chronic illness.
- Public Health Campaigns: Implementing public health campaigns to raise awareness about chronic illnesses and promote healthy behaviors can help prevent these conditions and improve health outcomes.
Conclusion
Chronic illnesses pose a significant economic burden on individuals, families, healthcare systems, and societies worldwide. Addressing this burden requires a comprehensive approach that involves prevention, early detection, effective management, and supportive policies. By investing in these strategies, we can reduce the prevalence of chronic illnesses, improve health outcomes, and promote economic growth and social well-being.







Leave a Reply