“Complications Associated with Bone Fractures
Related Articles Complications Associated with Bone Fractures
- First Aid For Bone Fractures: Dos And Don’ts
- Treatment Options For Osteoporosis: Medications And Therapies
- Signs And Symptoms Of Bone Density Loss
- Absolutely! Here’s A Comprehensive Article About Osteoporosis, Covering Its Causes, Symptoms, Prevention, And More.
- The Cornerstone Of Strong Bones: Unveiling The Vital Role Of Calcium
Introduction
On this special occasion, we are happy to review interesting topics related to Complications Associated with Bone Fractures. Let’s knit interesting information and provide new insights to readers.
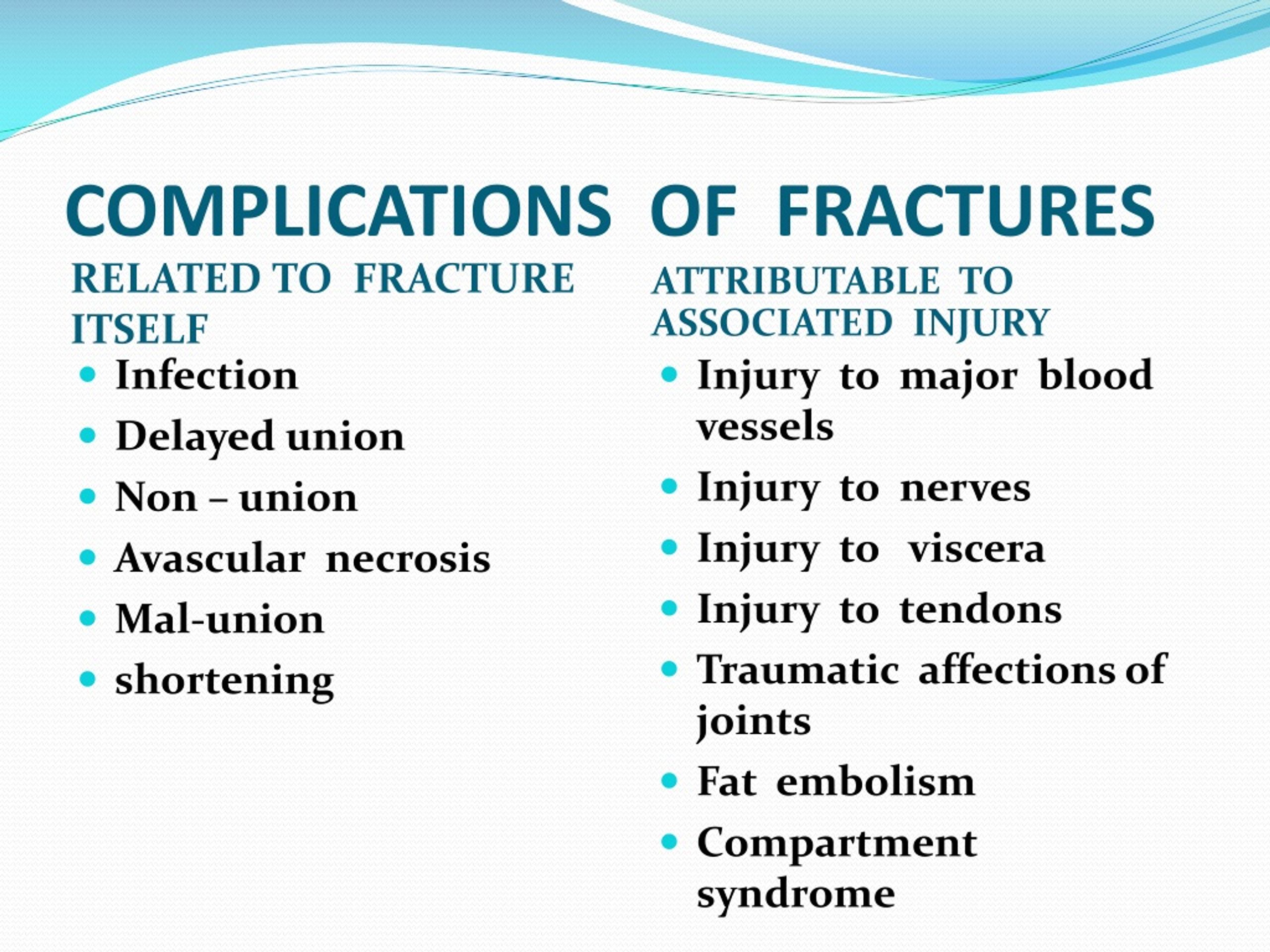
Complications Associated with Bone Fractures

Bone fractures, commonly known as broken bones, are a prevalent injury affecting individuals across all age groups. While many fractures heal without significant issues, complications can arise during the healing process or as a direct consequence of the injury. These complications can range from minor inconveniences to life-threatening conditions, necessitating prompt diagnosis and management. This article aims to provide a comprehensive overview of the various complications associated with bone fractures, encompassing their causes, clinical presentations, diagnostic approaches, and management strategies.
I. Early Complications
Early complications manifest shortly after the fracture occurs and require immediate attention to prevent long-term sequelae.
A. Neurovascular Injury
Fractures can inflict damage on nearby nerves and blood vessels, leading to neurovascular injury. The risk is heightened in fractures involving bones in close proximity to major neurovascular structures, such as the humerus, femur, and tibia.
- Nerve Injury: Nerve damage can result in sensory deficits (numbness, tingling), motor weakness, or paralysis in the affected limb. The specific symptoms depend on the nerve involved and the extent of the injury.
- Vascular Injury: Damage to blood vessels can compromise blood supply to the fractured bone and surrounding tissues, potentially leading to ischemia (lack of blood flow) and tissue necrosis (tissue death). In severe cases, vascular injury can necessitate amputation.
Diagnosis and Management: Prompt assessment of neurovascular function is crucial in all fracture patients. Physical examination should include evaluation of pulses, capillary refill, sensation, and motor function. If neurovascular compromise is suspected, imaging studies such as angiography or nerve conduction studies may be necessary. Management may involve fracture reduction, immobilization, or surgical intervention to repair damaged vessels or nerves.
B. Compartment Syndrome
Compartment syndrome is a condition characterized by increased pressure within a closed fascial compartment, which compromises blood flow to the muscles and nerves within that compartment. It most commonly occurs in the lower leg and forearm after fractures.
- Causes: Compartment syndrome can arise from swelling and bleeding within the compartment, which can be exacerbated by tight casts or dressings.
- Clinical Presentation: The classic symptoms of compartment syndrome include pain out of proportion to the injury, pallor (pale skin), paresthesia (numbness or tingling), pulselessness (weak or absent pulse), and paralysis.
- Diagnosis and Management: Early diagnosis is critical to prevent irreversible muscle and nerve damage. Compartment pressure measurements can confirm the diagnosis. Treatment involves immediate fasciotomy, a surgical procedure to release the pressure within the compartment.
C. Fat Embolism Syndrome (FES)
Fat embolism syndrome (FES) is a rare but potentially life-threatening complication that can occur after long bone fractures, particularly those involving the femur or tibia.
- Pathophysiology: Fat globules released from the bone marrow enter the bloodstream and travel to the lungs, where they can cause inflammation and impaired gas exchange.
- Clinical Presentation: FES typically presents 24-72 hours after the fracture with a triad of symptoms: respiratory distress, neurological dysfunction, and petechial rash (small, pinpoint-sized red spots on the skin).
- Diagnosis and Management: Diagnosis is based on clinical findings and supporting laboratory tests. Management is primarily supportive and includes oxygen therapy, mechanical ventilation, and fluid resuscitation.
D. Acute Respiratory Distress Syndrome (ARDS)
ARDS is a severe form of lung injury characterized by widespread inflammation and fluid accumulation in the lungs. It can occur as a complication of FES or as a result of other factors such as trauma, infection, or aspiration.
- Clinical Presentation: ARDS presents with severe shortness of breath, rapid breathing, and low blood oxygen levels.
- Diagnosis and Management: Diagnosis is based on clinical findings, chest X-ray, and blood gas analysis. Management involves mechanical ventilation, fluid management, and treatment of the underlying cause.
E. Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)
Fractures, particularly those involving the lower extremities, increase the risk of deep vein thrombosis (DVT), a blood clot that forms in a deep vein, usually in the leg. DVT can lead to pulmonary embolism (PE), a life-threatening condition in which a blood clot travels to the lungs and blocks blood flow.
- Risk Factors: Risk factors for DVT/PE after fracture include immobilization, surgery, and underlying medical conditions.
- Clinical Presentation: DVT may present with pain, swelling, and redness in the affected leg. PE may present with sudden shortness of breath, chest pain, and coughing up blood.
- Diagnosis and Management: Diagnosis of DVT is typically made with ultrasound. PE is diagnosed with CT angiography. Management involves anticoagulation therapy to prevent further clot formation and prevent existing clots from growing.
II. Delayed Complications
Delayed complications manifest weeks, months, or even years after the initial fracture.
A. Delayed Union and Nonunion
Delayed union refers to a fracture that is healing more slowly than expected. Nonunion refers to a fracture that has completely failed to heal.
- Causes: Factors that can contribute to delayed union or nonunion include inadequate blood supply, infection, instability of the fracture site, and certain medical conditions.
- Clinical Presentation: Delayed union may present with persistent pain and tenderness at the fracture site. Nonunion may present with pain, instability, and abnormal movement at the fracture site.
- Diagnosis and Management: Diagnosis is based on clinical examination and imaging studies, such as X-rays or CT scans. Management may involve bone grafting, internal fixation, or electrical stimulation to promote healing.
B. Malunion
Malunion refers to a fracture that has healed in an unsatisfactory position, leading to deformity or impaired function.
- Causes: Malunion can result from inadequate fracture reduction, instability of the fracture site, or failure to follow post-operative instructions.
- Clinical Presentation: Malunion may present with pain, deformity, limited range of motion, and difficulty with weight-bearing.
- Diagnosis and Management: Diagnosis is based on clinical examination and imaging studies. Management may involve corrective osteotomy (surgical cutting and repositioning of the bone) to restore proper alignment.
C. Avascular Necrosis (AVN)
Avascular necrosis (AVN), also known as osteonecrosis, is a condition in which bone tissue dies due to lack of blood supply. It can occur after fractures that disrupt the blood supply to the bone, such as fractures of the femoral neck or scaphoid.
- Clinical Presentation: AVN may present with pain, stiffness, and limited range of motion in the affected joint.
- Diagnosis and Management: Diagnosis is based on imaging studies, such as MRI or bone scan. Management may involve pain management, physical therapy, or surgical procedures such as core decompression, bone grafting, or joint replacement.
D. Post-traumatic Arthritis
Post-traumatic arthritis is a form of arthritis that develops after a fracture, even if the fracture heals properly. It is caused by damage to the cartilage within the joint.
- Clinical Presentation: Post-traumatic arthritis presents with pain, stiffness, swelling, and decreased range of motion in the affected joint.
- Diagnosis and Management: Diagnosis is based on clinical examination and imaging studies. Management may involve pain management, physical therapy, joint injections, or joint replacement.
E. Infection (Osteomyelitis)
Infection can occur after an open fracture (a fracture that breaks through the skin) or after surgical fixation of a fracture. Osteomyelitis is an infection of the bone.
- Clinical Presentation: Osteomyelitis may present with pain, redness, swelling, warmth, and drainage from the wound. Systemic symptoms such as fever and chills may also be present.
- Diagnosis and Management: Diagnosis is based on clinical examination, blood tests, and imaging studies. Management involves antibiotics and surgical debridement (removal of infected tissue).
III. Conclusion
Bone fractures can be associated with a wide range of complications, both early and delayed. Prompt diagnosis and management of these complications are essential to prevent long-term sequelae and optimize patient outcomes. Healthcare professionals should be vigilant in monitoring fracture patients for signs and symptoms of complications and should implement appropriate treatment strategies as needed. By understanding the potential complications associated with bone fractures, clinicians can provide comprehensive care and improve the overall well-being of their patients.







Leave a Reply