“Angioplasty Explained: What to Expect
Related Articles Angioplasty Explained: What to Expect
- Patient Empowerment In Chronic Disease Management – Part 9: Leveraging Technology For Enhanced Self-Management And Engagement
- Financial Challenges Of Living With Chronic Illness – Part 2
- Clinical Trials In Leukemia Treatment: Patient Considerations
- Leukemia Epidemiology: Global Trends And Regional Variances
- Palliative Care And Quality Of Life For Chronic Illness Patients – Part 5: Navigating Ethical Dilemmas And Future Directions
Introduction
With great enthusiasm, let’s explore interesting topics related to Angioplasty Explained: What to Expect. Come on knit interesting information and provide new insights to readers.
Table of Content
Angioplasty Explained: What to Expect

Angioplasty, also known as percutaneous transluminal coronary angioplasty (PTCA), is a minimally invasive procedure used to open blocked or narrowed coronary arteries. These arteries supply blood to the heart muscle, and when they become clogged with plaque, it can lead to chest pain (angina) and an increased risk of heart attack. Angioplasty is a common and effective treatment option for individuals with coronary artery disease (CAD).
Understanding Coronary Artery Disease (CAD)
Before delving into the specifics of angioplasty, it’s crucial to understand the underlying condition it addresses: coronary artery disease. CAD is a condition in which plaque, composed of cholesterol, fat, and other substances, accumulates inside the coronary arteries. This buildup, known as atherosclerosis, narrows the arteries and restricts blood flow to the heart.
The consequences of CAD can be significant. Reduced blood flow to the heart muscle can cause:
- Angina: Chest pain or discomfort that occurs when the heart muscle doesn’t receive enough oxygen-rich blood.
- Shortness of Breath: Difficulty breathing, especially during physical activity.
- Fatigue: Feeling unusually tired or weak.
- Heart Attack: A life-threatening event that occurs when blood flow to a portion of the heart is completely blocked, causing damage to the heart muscle.
When is Angioplasty Recommended?
Angioplasty is typically recommended for individuals who:
- Have significant narrowing or blockages in their coronary arteries.
- Experience angina that is not adequately controlled with medication.
- Have had a heart attack and require immediate restoration of blood flow to the heart.
- Have undergone stress tests or other diagnostic procedures that indicate reduced blood flow to the heart.
The Angioplasty Procedure: A Step-by-Step Guide
Angioplasty is performed in a hospital’s cardiac catheterization laboratory (cath lab). Here’s a detailed overview of what to expect during the procedure:
-
Preparation:
- You’ll be asked to avoid eating or drinking for several hours before the procedure.
- Your doctor will review your medical history, current medications, and allergies.
- You’ll be given a local anesthetic to numb the insertion site, usually in the groin or wrist.
- An intravenous (IV) line will be inserted to administer medications and fluids.
- Your heart rate, blood pressure, and oxygen levels will be monitored throughout the procedure.
-
Catheter Insertion:
- A small incision is made at the insertion site.
- A thin, flexible tube called a catheter is inserted into an artery, typically the femoral artery in the groin or the radial artery in the wrist.
- The catheter is carefully guided through the artery to the blocked or narrowed coronary artery.
-
Angiography:
- Once the catheter is in place, a contrast dye is injected into the coronary arteries.
- X-ray images are taken to visualize the location and extent of the blockage. This process is called angiography.
-
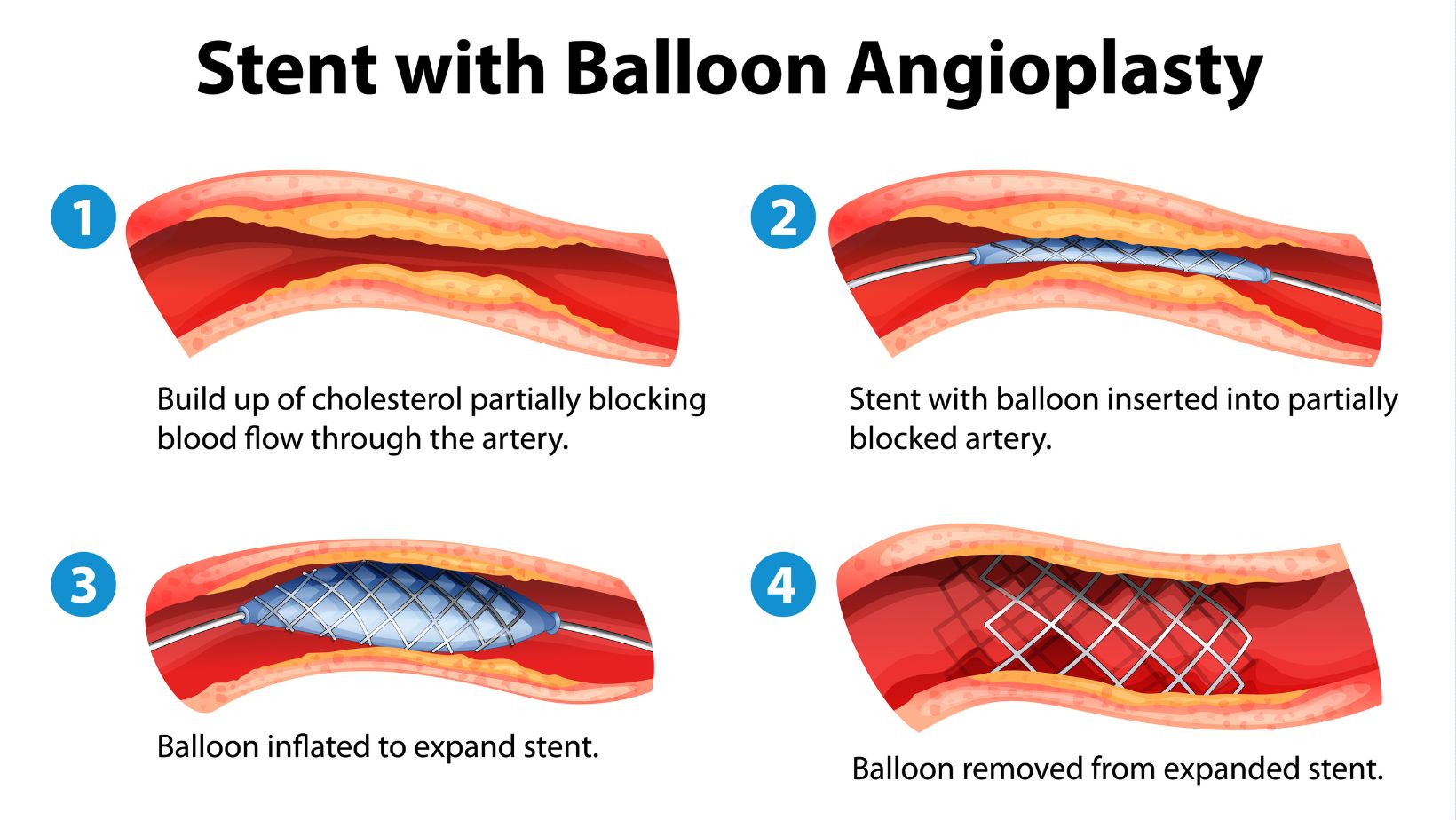
Balloon Angioplasty:
- A deflated balloon catheter is advanced through the guide catheter to the site of the blockage.
- The balloon is inflated, compressing the plaque against the artery walls and widening the artery.
- The balloon is then deflated and removed.
-
Stent Placement (Optional but Common):
- In most cases, a stent is placed in the artery after balloon angioplasty to help keep the artery open.
- A stent is a small, expandable mesh tube that is mounted on the balloon catheter.
- When the balloon is inflated, the stent expands and presses against the artery walls.
- The balloon is deflated and removed, leaving the stent in place to provide structural support.
- There are two main types of stents:
- Bare-metal stents (BMS): These stents are made of metal and do not have a drug coating.
- Drug-eluting stents (DES): These stents are coated with medication that helps prevent the artery from narrowing again (restenosis).
-
Final Angiography:
- After the balloon angioplasty and stent placement (if applicable), another angiography is performed to ensure that the artery is open and blood flow has been restored.
-
Catheter Removal and Closure:
- The catheter is carefully removed from the artery.
- The insertion site is closed using a closure device, such as a suture, clip, or collagen plug, to prevent bleeding.
- A pressure dressing is applied to the insertion site.
Duration of the Procedure
Angioplasty typically takes between 30 minutes to an hour to complete, but the duration can vary depending on the complexity of the case and the number of blockages being treated.
Recovery After Angioplasty
Following angioplasty, you’ll be closely monitored in the hospital for a few hours or overnight. Here’s what to expect during the recovery period:
- Monitoring: Your heart rate, blood pressure, and oxygen levels will be continuously monitored.
- Bed Rest: You’ll need to lie flat for several hours to allow the insertion site to heal and prevent bleeding.
- Pain Management: You may experience some discomfort or pain at the insertion site, which can be managed with pain medication.
- Hydration: You’ll be encouraged to drink plenty of fluids to help flush the contrast dye from your system.
- Discharge Instructions: Before you leave the hospital, your doctor will provide you with detailed discharge instructions, including:
- Medication instructions (especially antiplatelet medications like aspirin and clopidogrel)
- Wound care instructions
- Activity restrictions
- Follow-up appointment schedule
- Warning signs to watch out for
Medications After Angioplasty
After angioplasty, you’ll likely need to take medications to prevent blood clots and reduce the risk of future heart problems. These medications may include:
- Antiplatelet Medications: Aspirin and clopidogrel (Plavix) are commonly prescribed to prevent blood clots from forming in the stent. It’s crucial to take these medications as directed, as stopping them prematurely can increase the risk of stent thrombosis (blood clot formation within the stent).
- Statins: These medications help lower cholesterol levels and reduce the risk of further plaque buildup in the arteries.
- Beta-Blockers: These medications help slow down the heart rate and lower blood pressure, reducing the workload on the heart.
- ACE Inhibitors or ARBs: These medications help lower blood pressure and protect the heart from damage.
Lifestyle Changes After Angioplasty
In addition to medications, lifestyle changes are essential for maintaining long-term heart health after angioplasty. These changes include:
- Heart-Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean protein. Limit saturated and trans fats, cholesterol, sodium, and added sugars.
- Regular Exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Talk to your doctor about what types of exercise are safe and appropriate for you.
- Weight Management: Maintain a healthy weight to reduce the strain on your heart.
- Smoking Cessation: If you smoke, quitting is the single most important thing you can do for your heart health.
- Stress Management: Find healthy ways to manage stress, such as yoga, meditation, or spending time in nature.
- Regular Checkups: Attend regular follow-up appointments with your doctor to monitor your heart health and make any necessary adjustments to your treatment plan.
Potential Risks and Complications
Angioplasty is generally a safe procedure, but like any medical intervention, it carries some potential risks and complications. These may include:
- Bleeding: Bleeding at the insertion site.
- Infection: Infection at the insertion site.
- Allergic Reaction: Allergic reaction to the contrast dye.
- Arrhythmia: Irregular heart rhythm.
- Artery Damage: Damage to the artery during catheter insertion or balloon inflation.
- Stent Thrombosis: Blood clot formation within the stent.
- Restenosis: Narrowing of the artery again after angioplasty.
- Heart Attack: Heart attack during or after the procedure (rare).
- Stroke: Stroke during or after the procedure (rare).
When to Seek Medical Attention
It’s important to seek immediate medical attention if you experience any of the following symptoms after angioplasty:
- Chest pain or discomfort
- Shortness of breath
- Dizziness or lightheadedness
- Swelling, redness, or drainage at the insertion site
- Fever
- Numbness or weakness in your arm or leg
Conclusion
Angioplasty is a valuable treatment option for individuals with coronary artery disease. By opening blocked or narrowed arteries, it can relieve angina symptoms, improve blood flow to the heart, and reduce the risk of heart attack. Understanding the procedure, recovery process, and necessary lifestyle changes can empower patients to take control of their heart health and live longer, healthier lives. Always discuss any concerns or questions you have with your doctor to make informed decisions about your treatment.







Leave a Reply