“Sleep Disorders and Chronic Disease Relationships – Part 9
Related Articles Sleep Disorders and Chronic Disease Relationships – Part 9
- Challenges In Diagnosing Rare Chronic Illnesses – Part 6
- Disability Rights And Advocacy For Chronic Disease Patients – Part 8
- Chronic Disease Trends In Aging Populations – Part 5: Navigating The Complexities Of Multimorbidity And Integrated Care Models
- Integrative Care Models For Complex Chronic Diseases – Part 8
- Chronic Disease Surveillance And Epidemiology – Part 7: Data Linkage In Chronic Disease Surveillance
Introduction
With great enthusiasm, let’s explore interesting topics related to Sleep Disorders and Chronic Disease Relationships – Part 9. Let’s knit interesting information and provide new insights to readers.
Table of Content
Sleep Disorders and Chronic Disease Relationships – Part 9

Sleep is a fundamental human need, akin to eating, drinking, and breathing. It plays a pivotal role in maintaining physical and mental health, and its disruption can lead to a cascade of adverse health outcomes. Sleep disorders, characterized by abnormal sleep patterns or behaviors, are increasingly recognized as significant contributors to the development and progression of various chronic diseases. This article delves into the intricate relationships between sleep disorders and chronic diseases, exploring the underlying mechanisms, clinical implications, and potential therapeutic strategies.
The Interplay Between Sleep and Health
Sleep is not merely a period of rest; it is an active process that involves a complex interplay of physiological and neurological events. During sleep, the body repairs tissues, consolidates memories, and regulates hormones. Sleep deprivation or disruption can disrupt these processes, leading to a wide range of health problems.
Chronic diseases, on the other hand, are long-lasting health conditions that cannot be cured but can be controlled. These diseases are often associated with significant morbidity, disability, and mortality. The relationship between sleep disorders and chronic diseases is bidirectional, meaning that sleep disorders can increase the risk of developing chronic diseases, and chronic diseases can exacerbate sleep disorders.
Common Sleep Disorders
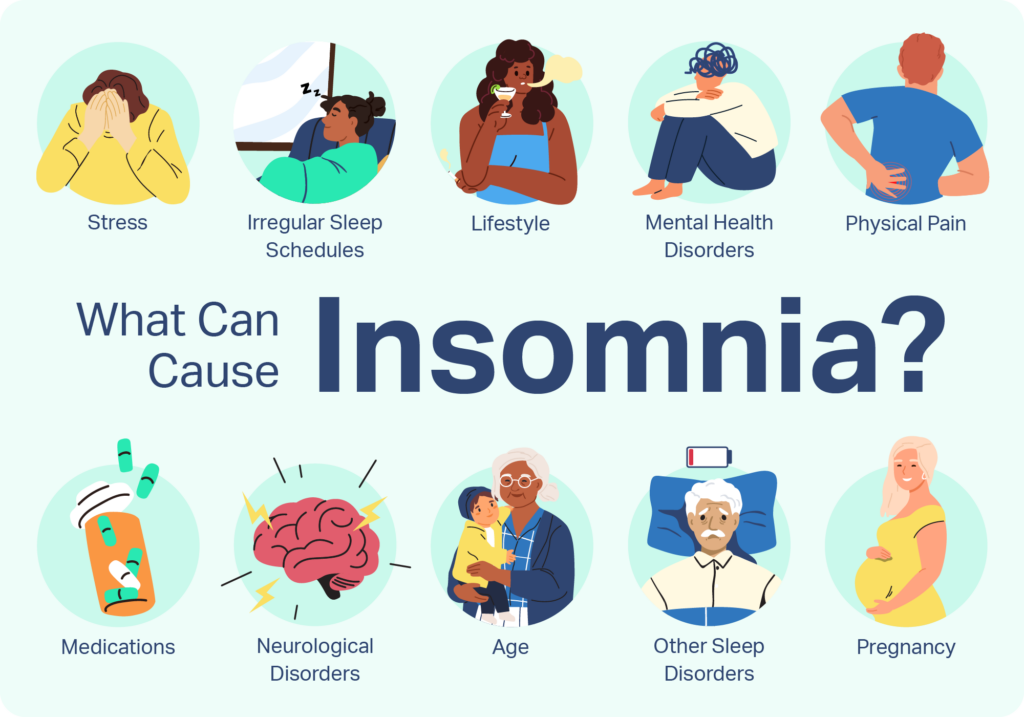
Several sleep disorders can disrupt sleep patterns and negatively impact health. Some of the most common sleep disorders include:
- Insomnia: Difficulty falling asleep, staying asleep, or experiencing non-restorative sleep.
- Sleep Apnea: Repeated pauses in breathing during sleep, leading to oxygen desaturation and sleep fragmentation.
- Restless Legs Syndrome (RLS): An irresistible urge to move the legs, often accompanied by uncomfortable sensations.
- Narcolepsy: Excessive daytime sleepiness, often accompanied by cataplexy (sudden muscle weakness).
- Circadian Rhythm Disorders: Disruptions in the body’s natural sleep-wake cycle.
Sleep Disorders and Cardiovascular Disease
Cardiovascular disease (CVD) is a leading cause of death worldwide, and sleep disorders are increasingly recognized as significant risk factors. Several studies have demonstrated a strong association between sleep disorders and various CVD outcomes, including hypertension, coronary artery disease, stroke, and heart failure.
- Hypertension: Sleep apnea, in particular, is strongly associated with hypertension. The intermittent hypoxia and sleep fragmentation associated with sleep apnea can activate the sympathetic nervous system, leading to increased blood pressure.
- Coronary Artery Disease: Sleep deprivation and sleep fragmentation can increase inflammation and oxidative stress, which are key contributors to the development of coronary artery disease.
- Stroke: Sleep apnea has been linked to an increased risk of stroke. The intermittent hypoxia and sleep fragmentation associated with sleep apnea can damage blood vessels and increase the risk of blood clots.
- Heart Failure: Sleep apnea can worsen heart failure by increasing the workload on the heart and reducing oxygen supply.
Sleep Disorders and Metabolic Disorders
Metabolic disorders, such as diabetes and obesity, are characterized by abnormal metabolism of glucose, lipids, and proteins. Sleep disorders can disrupt metabolic processes and increase the risk of developing these disorders.
- Diabetes: Sleep deprivation and sleep fragmentation can impair glucose metabolism and insulin sensitivity, leading to an increased risk of type 2 diabetes.
- Obesity: Sleep deprivation can disrupt appetite-regulating hormones, leading to increased food intake and weight gain.
- Metabolic Syndrome: Sleep disorders have been linked to an increased risk of metabolic syndrome, a cluster of conditions that increase the risk of CVD, diabetes, and stroke.
Sleep Disorders and Neurological Disorders
Neurological disorders, such as Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis, can significantly impact sleep quality and quantity. Conversely, sleep disorders can exacerbate neurological symptoms and accelerate disease progression.
- Alzheimer’s Disease: Sleep disturbances are common in Alzheimer’s disease and may contribute to cognitive decline.
- Parkinson’s Disease: Sleep disorders, such as REM sleep behavior disorder, are common in Parkinson’s disease and may precede the onset of motor symptoms.
- Multiple Sclerosis: Sleep disorders, such as insomnia and restless legs syndrome, are common in multiple sclerosis and can worsen fatigue and other symptoms.
Sleep Disorders and Mental Health Disorders
Mental health disorders, such as depression, anxiety, and post-traumatic stress disorder (PTSD), are often associated with sleep disturbances. Sleep disorders can exacerbate mental health symptoms and increase the risk of relapse.
- Depression: Insomnia is a common symptom of depression, and sleep deprivation can worsen depressive symptoms.
- Anxiety: Sleep disturbances are common in anxiety disorders, and sleep deprivation can increase anxiety levels.
- Post-Traumatic Stress Disorder (PTSD): Nightmares and insomnia are common symptoms of PTSD, and sleep deprivation can worsen PTSD symptoms.
Underlying Mechanisms
The relationships between sleep disorders and chronic diseases are complex and multifaceted. Several underlying mechanisms may contribute to these associations, including:
- Inflammation: Sleep deprivation and sleep fragmentation can increase inflammation, which is a key contributor to many chronic diseases.
- Oxidative Stress: Sleep deprivation can increase oxidative stress, which can damage cells and tissues.
- Hormonal Imbalances: Sleep deprivation can disrupt hormone regulation, leading to imbalances in cortisol, insulin, and other hormones.
- Sympathetic Nervous System Activation: Sleep apnea can activate the sympathetic nervous system, leading to increased blood pressure and heart rate.
Clinical Implications
The strong associations between sleep disorders and chronic diseases have significant clinical implications. Healthcare professionals should routinely screen patients for sleep disorders, particularly those with chronic diseases. Early diagnosis and treatment of sleep disorders can improve sleep quality, reduce the risk of chronic disease complications, and improve overall health outcomes.
Therapeutic Strategies
Several therapeutic strategies can be used to manage sleep disorders and mitigate their impact on chronic diseases. These strategies include:
- Lifestyle Modifications: Improving sleep hygiene, such as establishing a regular sleep schedule, creating a relaxing bedtime routine, and avoiding caffeine and alcohol before bed.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): A structured therapy that helps individuals identify and change thoughts and behaviors that contribute to insomnia.
- Continuous Positive Airway Pressure (CPAP): A treatment for sleep apnea that involves wearing a mask that delivers pressurized air to keep the airway open during sleep.
- Medications: Several medications can be used to treat sleep disorders, such as insomnia, restless legs syndrome, and narcolepsy.
Future Directions
Further research is needed to fully elucidate the complex relationships between sleep disorders and chronic diseases. Future studies should focus on:
- Identifying specific mechanisms: Further research is needed to identify the specific mechanisms that link sleep disorders to chronic diseases.
- Developing targeted therapies: Developing targeted therapies that address the underlying mechanisms linking sleep disorders to chronic diseases.
- Implementing preventive strategies: Implementing preventive strategies to reduce the risk of developing sleep disorders and chronic diseases.
Conclusion
Sleep disorders are increasingly recognized as significant contributors to the development and progression of various chronic diseases. The relationships between sleep disorders and chronic diseases are complex and multifaceted, involving several underlying mechanisms, including inflammation, oxidative stress, hormonal imbalances, and sympathetic nervous system activation. Healthcare professionals should routinely screen patients for sleep disorders, particularly those with chronic diseases. Early diagnosis and treatment of sleep disorders can improve sleep quality, reduce the risk of chronic disease complications, and improve overall health outcomes.







Leave a Reply