“Technology’s Role in Chronic Disease Self-Management – Part 8: The Future of Personalized and Predictive Care
Related Articles Technology’s Role in Chronic Disease Self-Management – Part 8: The Future of Personalized and Predictive Care
- Chronic Disease Trends In Aging Populations
- Medical Advances In Treating Rare Chronic Conditions – Part 2
- Holistic Wellness Programs For Chronic Disease Patients – Part 6
- Workplace Accommodations For Employees With Chronic Diseases – Part 2
- The Impact Of Chronic Illness On Mental Health – Part 6
Introduction
We will be happy to explore interesting topics related to Technology’s Role in Chronic Disease Self-Management – Part 8: The Future of Personalized and Predictive Care. Let’s knit interesting information and provide new insights to readers.
Table of Content
Technology’s Role in Chronic Disease Self-Management – Part 8: The Future of Personalized and Predictive Care
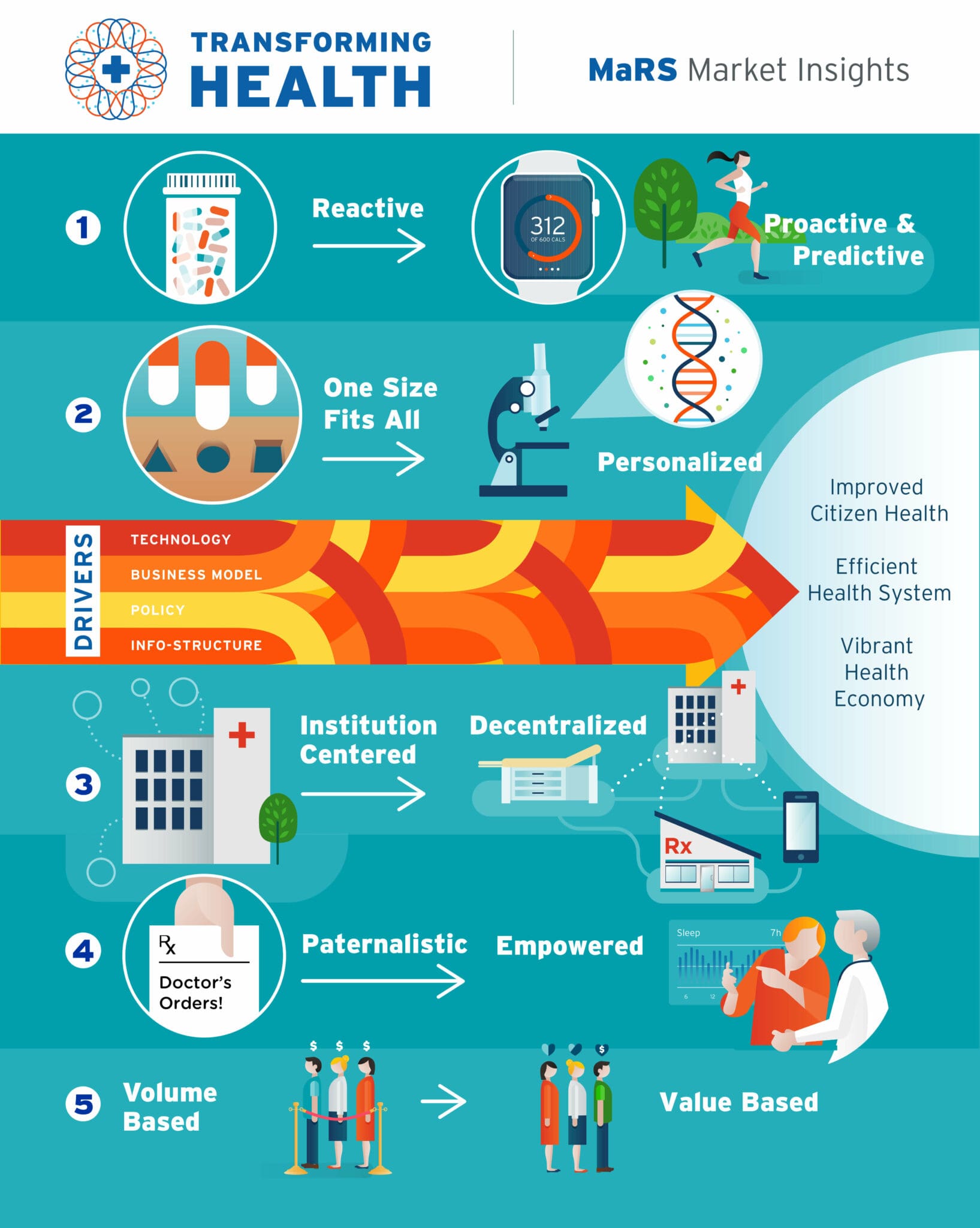
The relentless march of technological advancement continues to reshape healthcare, with chronic disease self-management emerging as a prime beneficiary. In previous installments of this series, we explored the transformative impact of various technologies, including telehealth, mobile apps, wearables, and remote monitoring devices. Now, in Part 8, we delve into the exciting frontier of personalized and predictive care, where technology promises to tailor interventions to individual needs and anticipate health events before they occur.
The Promise of Personalized Medicine
Personalized medicine, also known as precision medicine, aims to deliver the right treatment to the right patient at the right time. This approach recognizes that individuals respond differently to therapies due to variations in their genetic makeup, lifestyle, and environment. Technology plays a pivotal role in enabling personalized medicine by facilitating the collection, analysis, and interpretation of vast amounts of data.
1. Genetic Testing and Pharmacogenomics:
Genetic testing is becoming increasingly accessible and affordable, allowing individuals to gain insights into their predisposition to certain chronic diseases, such as diabetes, cardiovascular disease, and cancer. Pharmacogenomics, a related field, examines how genes affect a person’s response to drugs. By analyzing an individual’s genetic profile, healthcare providers can identify the most effective medications and dosages, minimizing the risk of adverse effects.
2. Omics Technologies:
Beyond genomics, other "omics" technologies, such as proteomics (study of proteins) and metabolomics (study of metabolites), provide a more comprehensive understanding of an individual’s biological state. These technologies can reveal subtle changes in the body that may indicate early signs of disease or predict the likelihood of disease progression.
3. Data Integration and Analysis:
The true power of personalized medicine lies in integrating data from various sources, including genetic information, medical history, lifestyle factors, and environmental exposures. Advanced analytics techniques, such as machine learning and artificial intelligence (AI), can analyze these complex datasets to identify patterns and predict individual health risks.
Predictive Analytics: Anticipating Health Events
Predictive analytics leverages data and statistical algorithms to forecast future events. In chronic disease self-management, predictive analytics can be used to identify individuals at high risk of developing complications, predict disease exacerbations, and personalize interventions to prevent adverse outcomes.
1. Risk Stratification:
Predictive models can stratify individuals based on their risk of developing specific chronic diseases or experiencing complications. This allows healthcare providers to focus resources on those who are most likely to benefit from early intervention. For example, predictive models can identify individuals with prediabetes who are at high risk of developing type 2 diabetes and target them with intensive lifestyle modification programs.
2. Early Warning Systems:
Predictive analytics can also be used to develop early warning systems that detect subtle changes in an individual’s health status that may indicate an impending crisis. For example, wearable sensors can track vital signs, such as heart rate and blood pressure, and alert healthcare providers if they detect abnormal patterns that may indicate an increased risk of heart attack or stroke.
3. Personalized Interventions:
Predictive analytics can inform the development of personalized interventions tailored to an individual’s specific needs and risk factors. For example, individuals at high risk of developing diabetic foot ulcers can be provided with specialized footwear, education on foot care, and remote monitoring to detect early signs of ulceration.
The Role of Artificial Intelligence (AI)
AI is rapidly transforming healthcare, with significant implications for personalized and predictive care in chronic disease self-management. AI algorithms can analyze vast amounts of data, identify patterns, and make predictions with remarkable accuracy.
1. Machine Learning:
Machine learning, a subset of AI, involves training algorithms on data to learn patterns and make predictions without explicit programming. Machine learning algorithms can be used to develop predictive models for various chronic diseases, personalize treatment plans, and automate tasks such as medication adherence monitoring.
2. Natural Language Processing (NLP):
NLP enables computers to understand and process human language. NLP can be used to extract information from electronic health records, analyze patient feedback, and provide personalized education and support.
3. Computer Vision:
Computer vision allows computers to "see" and interpret images. Computer vision can be used to analyze medical images, such as X-rays and MRIs, to detect early signs of disease or monitor disease progression.
Challenges and Considerations
While personalized and predictive care holds immense promise, several challenges and considerations must be addressed to ensure its responsible and effective implementation.
1. Data Privacy and Security:
The collection and use of sensitive health data raise concerns about privacy and security. Robust security measures and data governance policies are essential to protect patient information and maintain trust.
2. Data Bias:
AI algorithms are only as good as the data they are trained on. If the data is biased, the algorithms may perpetuate or even amplify existing health disparities. It is crucial to ensure that data used to train AI algorithms is representative of the population and free from bias.
3. Ethical Considerations:
The use of AI in healthcare raises ethical concerns about autonomy, transparency, and accountability. It is important to develop ethical guidelines and regulations to ensure that AI is used in a way that is fair, transparent, and respects patient autonomy.
4. Integration with Existing Systems:
Integrating personalized and predictive care technologies with existing healthcare systems can be complex and challenging. Interoperability standards and data exchange protocols are needed to ensure seamless data flow and communication between different systems.
5. Cost and Accessibility:
Personalized and predictive care technologies can be expensive, potentially exacerbating health disparities. Efforts are needed to reduce costs and ensure that these technologies are accessible to all individuals, regardless of their socioeconomic status.
The Future of Chronic Disease Self-Management
The future of chronic disease self-management is likely to be characterized by increasingly personalized and predictive care. As technology continues to advance, we can expect to see:
- More sophisticated predictive models: AI algorithms will become even more sophisticated, enabling more accurate predictions of disease risk and progression.
- More personalized interventions: Interventions will be tailored to an individual’s unique needs and preferences, taking into account their genetic makeup, lifestyle, and environment.
- More proactive care: Healthcare providers will be able to anticipate health events before they occur, allowing for early intervention and prevention of complications.
- Greater patient engagement: Patients will be more actively involved in their own care, empowered by technology to make informed decisions and manage their conditions effectively.
Conclusion
Personalized and predictive care represents a paradigm shift in chronic disease self-management. By leveraging technology to tailor interventions to individual needs and anticipate health events before they occur, we can improve outcomes, reduce costs, and empower individuals to live healthier, more fulfilling lives. However, it is crucial to address the challenges and considerations associated with these technologies to ensure their responsible and equitable implementation. As we move forward, collaboration between healthcare providers, technology developers, policymakers, and patients will be essential to realize the full potential of personalized and predictive care in chronic disease self-management.







Leave a Reply