“Comorbidities Associated with Common Chronic Diseases – Part 8: Chronic Obstructive Pulmonary Disease (COPD)
Related Articles Comorbidities Associated with Common Chronic Diseases – Part 8: Chronic Obstructive Pulmonary Disease (COPD)
- Emerging Therapies For Managing Chronic Conditions – Part 4: Precision Medicine, Biologic Therapies, And Neuromodulation Techniques
- Yoga And Mindfulness Practices For Chronic Disease Patients – Part 7: Integrating Practices Into Daily Life And Overcoming Challenges
- Gender Disparities In Chronic Disease Diagnosis And Treatment
- Innovations In Medical Devices For Chronic Disease Management – Part 5
- Yoga And Mindfulness Practices For Chronic Disease Patients
Introduction
With great enthusiasm, let’s explore interesting topics related to Comorbidities Associated with Common Chronic Diseases – Part 8: Chronic Obstructive Pulmonary Disease (COPD). Come on knit interesting information and provide new insights to readers.
Table of Content
Comorbidities Associated with Common Chronic Diseases – Part 8: Chronic Obstructive Pulmonary Disease (COPD)

Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by persistent airflow limitation. It is a major global health problem, affecting millions of people worldwide and imposing a substantial burden on healthcare systems. While COPD primarily affects the lungs, it is increasingly recognized as a systemic disease with a wide range of comorbidities. These comorbidities can significantly impact the clinical course, prognosis, and quality of life of individuals with COPD.
Understanding COPD
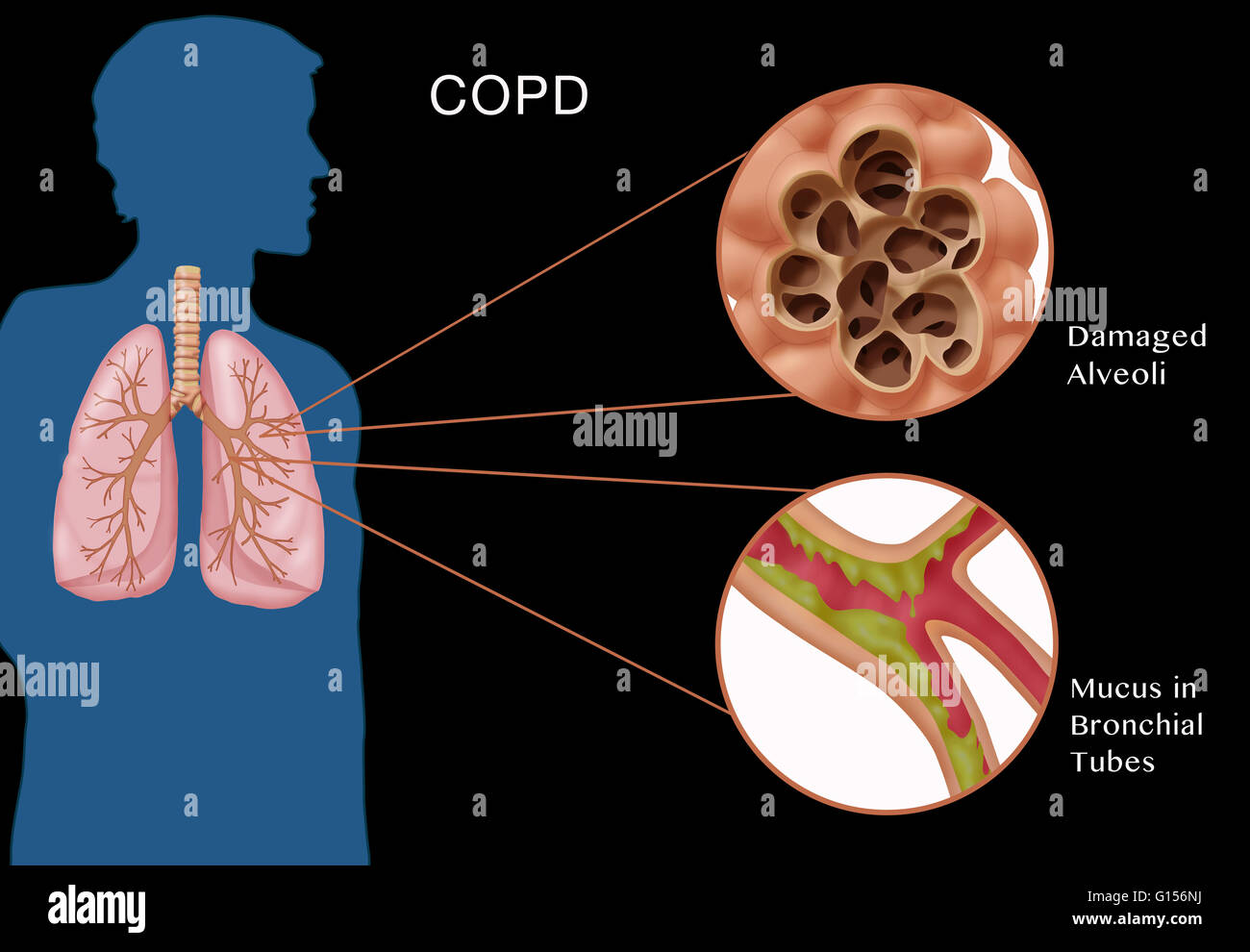
COPD encompasses two main conditions: emphysema and chronic bronchitis. Emphysema involves the destruction of the alveoli, the tiny air sacs in the lungs where oxygen and carbon dioxide exchange occurs. Chronic bronchitis is characterized by inflammation and narrowing of the bronchial tubes, leading to increased mucus production and chronic cough.
The primary cause of COPD is tobacco smoking, but other factors, such as exposure to air pollution, occupational dusts, and genetic predisposition, can also contribute to its development.
Common Comorbidities Associated with COPD
COPD rarely occurs in isolation. It is frequently associated with a variety of comorbidities, which can complicate the management of the disease and worsen patient outcomes. Some of the most common comorbidities associated with COPD include:
-
Cardiovascular Disease:
Cardiovascular disease (CVD) is a leading comorbidity in individuals with COPD. Several factors contribute to this association, including shared risk factors such as smoking, inflammation, and oxidative stress. COPD can increase the risk of various cardiovascular conditions, including:
- Ischemic Heart Disease: COPD is associated with an increased risk of coronary artery disease, angina, and myocardial infarction (heart attack).
- Heart Failure: COPD can lead to pulmonary hypertension, which increases the workload on the right side of the heart, potentially leading to right-sided heart failure (cor pulmonale). COPD can also contribute to left ventricular dysfunction and heart failure with preserved ejection fraction (HFpEF).
- Arrhythmias: COPD is associated with an increased risk of atrial fibrillation and other arrhythmias, which can further compromise cardiac function.
- Peripheral Artery Disease: COPD is linked to an increased risk of peripheral artery disease, which can cause leg pain, claudication, and increase the risk of amputation.
-
Lung Cancer:
Lung cancer is a significant comorbidity in individuals with COPD. Both COPD and lung cancer share common risk factors, such as smoking and exposure to environmental pollutants. COPD can increase the risk of developing lung cancer, and lung cancer can worsen the symptoms and prognosis of COPD.
-
Osteoporosis:
Osteoporosis, a condition characterized by decreased bone density and increased risk of fractures, is a common comorbidity in individuals with COPD. Several factors contribute to this association, including:
- Systemic Inflammation: COPD is associated with chronic systemic inflammation, which can promote bone resorption and reduce bone formation.
- Corticosteroid Use: Inhaled and oral corticosteroids, commonly used to treat COPD, can have adverse effects on bone metabolism and increase the risk of osteoporosis.
- Vitamin D Deficiency: Many individuals with COPD have low levels of vitamin D, which is essential for bone health.
- Physical Inactivity: COPD can lead to reduced physical activity, which can contribute to bone loss.
-
Depression and Anxiety:
Depression and anxiety are common psychiatric comorbidities in individuals with COPD. The chronic nature of COPD, the associated symptoms such as breathlessness and fatigue, and the impact on daily activities can contribute to the development of mood disorders. Depression and anxiety can worsen the symptoms of COPD, reduce adherence to treatment, and negatively impact quality of life.
-
Metabolic Syndrome and Diabetes:
Metabolic syndrome, a cluster of conditions including abdominal obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels, is more prevalent in individuals with COPD. COPD is also associated with an increased risk of type 2 diabetes. Several factors may contribute to this association, including:
- Systemic Inflammation: COPD-related inflammation can impair insulin sensitivity and glucose metabolism.
- Physical Inactivity: Reduced physical activity due to COPD can contribute to weight gain and insulin resistance.
- Corticosteroid Use: Corticosteroids can increase blood sugar levels and increase the risk of diabetes.
-
Gastroesophageal Reflux Disease (GERD):
GERD, a condition in which stomach acid flows back into the esophagus, is a common comorbidity in individuals with COPD. The mechanisms underlying this association are not fully understood, but factors such as increased abdominal pressure due to chronic coughing and the use of certain medications may play a role. GERD can worsen the symptoms of COPD and contribute to exacerbations.
-
Obstructive Sleep Apnea (OSA):
OSA, a condition characterized by repeated episodes of upper airway obstruction during sleep, is more prevalent in individuals with COPD. The combination of COPD and OSA, known as overlap syndrome, can lead to more severe hypoxemia (low blood oxygen levels) and hypercapnia (high blood carbon dioxide levels), increasing the risk of pulmonary hypertension and cardiovascular complications.
-
Skeletal Muscle Dysfunction:
COPD can lead to skeletal muscle dysfunction, characterized by muscle weakness, reduced muscle mass, and impaired muscle endurance. Several factors contribute to this, including:
- Systemic Inflammation: COPD-related inflammation can promote muscle protein breakdown and reduce muscle protein synthesis.
- Hypoxemia: Low blood oxygen levels can impair muscle function.
- Physical Inactivity: Reduced physical activity can lead to muscle atrophy.
- Malnutrition: COPD can lead to reduced appetite and malnutrition, which can contribute to muscle loss.
-
Cognitive Impairment:
COPD is associated with an increased risk of cognitive impairment, including memory loss, attention deficits, and executive dysfunction. Several factors may contribute to this association, including:
- Hypoxemia: Chronic hypoxemia can damage brain cells.
- Systemic Inflammation: COPD-related inflammation can affect brain function.
- Cerebrovascular Disease: COPD is associated with an increased risk of stroke and other cerebrovascular diseases, which can impair cognitive function.
Management of Comorbidities in COPD
The management of comorbidities in COPD is essential for improving patient outcomes and quality of life. A comprehensive approach that addresses both the respiratory and non-respiratory aspects of the disease is necessary. Key strategies include:
- Smoking Cessation: Smoking cessation is the most important intervention for individuals with COPD, as it can slow the progression of the disease and reduce the risk of comorbidities.
- Pulmonary Rehabilitation: Pulmonary rehabilitation programs can improve exercise tolerance, reduce breathlessness, and enhance quality of life.
- Pharmacological Management: Bronchodilators, inhaled corticosteroids, and other medications can help to relieve symptoms and prevent exacerbations.
- Oxygen Therapy: Supplemental oxygen therapy may be necessary for individuals with severe hypoxemia.
- Management of Specific Comorbidities: Each comorbidity should be managed according to established guidelines. This may involve medications, lifestyle modifications, and other interventions.
- Multidisciplinary Care: A multidisciplinary team, including pulmonologists, cardiologists, psychiatrists, and other healthcare professionals, can provide comprehensive care for individuals with COPD and comorbidities.
Conclusion
COPD is a complex disease that is frequently associated with a wide range of comorbidities. These comorbidities can significantly impact the clinical course, prognosis, and quality of life of individuals with COPD. Recognizing and managing these comorbidities is essential for improving patient outcomes. A comprehensive approach that addresses both the respiratory and non-respiratory aspects of the disease, including smoking cessation, pulmonary rehabilitation, pharmacological management, and management of specific comorbidities, is necessary for optimal care. Future research should focus on further elucidating the mechanisms underlying the association between COPD and its comorbidities and on developing more effective strategies for prevention and management.







Leave a Reply