“Genetic Testing and Personalized Medicine in Chronic Diseases – Part 7
Related Articles Genetic Testing and Personalized Medicine in Chronic Diseases – Part 7
- The Impact Of Chronic Disease On Family Dynamics – Part 2
- Holistic Wellness Programs For Chronic Disease Patients – Part 7
- Environmental Factors And Chronic Disease Risk – Part 3
- Telemedicine And Remote Monitoring For Chronic Illness Care – Part 3
- Psychological Resilience In Chronic Disease Patients – Part 3: Strategies For Cultivating Resilience And Supporting Thriving
Introduction
We will be happy to explore interesting topics related to Genetic Testing and Personalized Medicine in Chronic Diseases – Part 7. Let’s knit interesting information and provide new insights to readers.
Table of Content
Genetic Testing and Personalized Medicine in Chronic Diseases – Part 7
Introduction
Chronic diseases, such as cardiovascular disease, cancer, diabetes, and neurodegenerative disorders, pose a significant global health burden. These conditions are characterized by their long duration, slow progression, and complex interplay of genetic, environmental, and lifestyle factors. Traditional approaches to managing chronic diseases often involve a one-size-fits-all strategy, which may not be effective for all patients due to individual variability in disease susceptibility, progression, and treatment response.
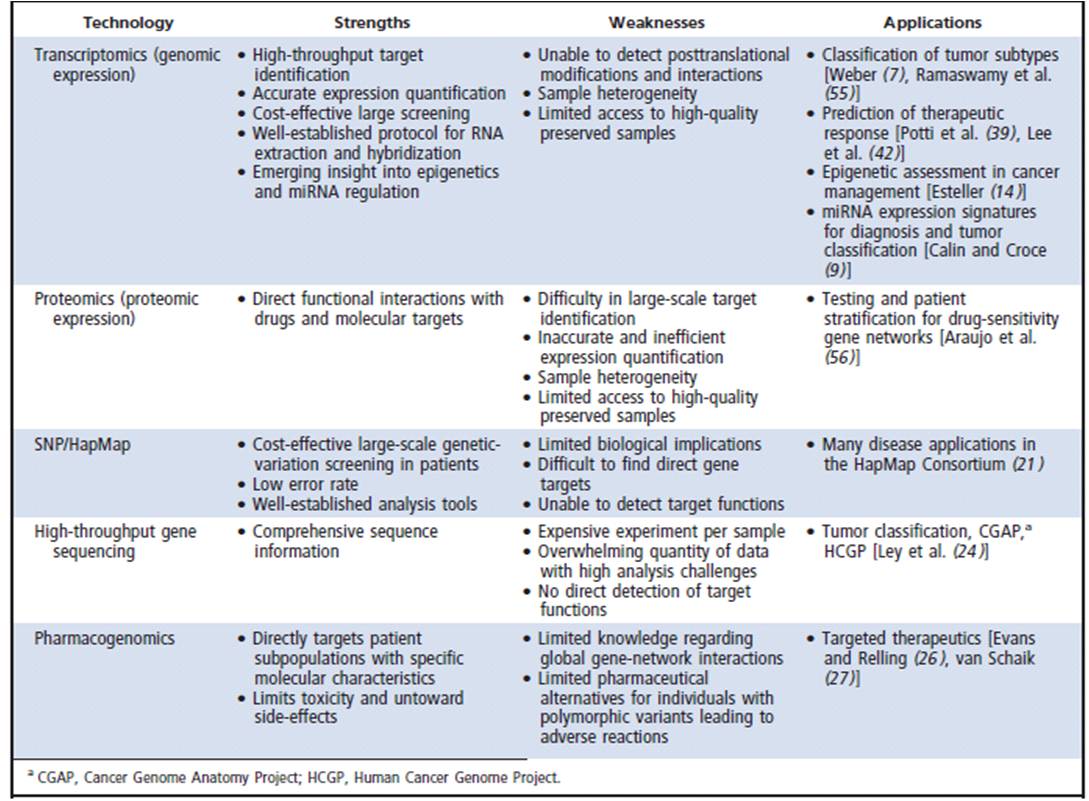
In recent years, advancements in genetic testing and personalized medicine have revolutionized the approach to chronic disease management. Genetic testing allows for the identification of genetic variations that contribute to disease risk, prognosis, and treatment response. Personalized medicine aims to tailor medical decisions, treatments, and preventive strategies to the individual characteristics of each patient, taking into account their genetic makeup, lifestyle, and environmental factors.
This article provides a comprehensive overview of the role of genetic testing and personalized medicine in the management of chronic diseases. It explores the applications of genetic testing in risk assessment, diagnosis, prognosis, and treatment selection for various chronic conditions. Additionally, it discusses the challenges and opportunities associated with the implementation of personalized medicine in clinical practice.
Genetic Testing in Chronic Diseases
Genetic testing plays a crucial role in the management of chronic diseases by providing valuable information about an individual’s risk of developing a disease, the underlying cause of the disease, the likely course of the disease, and the potential response to treatment.
-
Risk Assessment: Genetic testing can identify individuals who are at increased risk of developing certain chronic diseases based on their genetic makeup. For example, genetic testing can identify individuals with a higher risk of developing breast cancer, Alzheimer’s disease, or type 2 diabetes. This information can be used to implement preventive measures, such as lifestyle modifications, regular screening, or prophylactic medications, to reduce the risk of disease development or delay its onset.
-
Diagnosis: Genetic testing can aid in the diagnosis of chronic diseases, particularly those with a genetic component. For example, genetic testing can confirm the diagnosis of cystic fibrosis, Huntington’s disease, or certain types of cancer. Genetic testing can also help to differentiate between different subtypes of a disease, which can have implications for treatment and prognosis.
-
Prognosis: Genetic testing can provide information about the likely course of a chronic disease. For example, genetic testing can predict the rate of disease progression in Alzheimer’s disease or the likelihood of recurrence in cancer. This information can be used to make informed decisions about treatment and care planning.
-
Treatment Selection: Genetic testing can guide the selection of the most appropriate treatment for a chronic disease based on an individual’s genetic makeup. For example, genetic testing can identify individuals who are more likely to respond to a particular drug or who are at higher risk of experiencing adverse drug reactions. This information can be used to personalize treatment plans and improve treatment outcomes.
Personalized Medicine in Chronic Diseases
Personalized medicine is an approach to healthcare that tailors medical decisions, treatments, and preventive strategies to the individual characteristics of each patient. This approach takes into account an individual’s genetic makeup, lifestyle, and environmental factors to optimize health outcomes.
-
Pharmacogenomics: Pharmacogenomics is the study of how genes affect a person’s response to drugs. Genetic testing can identify individuals who are more likely to respond to a particular drug or who are at higher risk of experiencing adverse drug reactions. This information can be used to personalize drug selection and dosage, improving treatment efficacy and reducing the risk of adverse events.
-
Targeted Therapies: Targeted therapies are drugs that are designed to specifically target cancer cells or other disease-causing cells. Genetic testing can identify individuals who are more likely to benefit from targeted therapies based on the genetic characteristics of their disease. This approach allows for the use of more effective and less toxic treatments.
-
Lifestyle Modifications: Personalized medicine also encompasses lifestyle modifications that are tailored to an individual’s genetic makeup and risk factors. For example, individuals with a genetic predisposition to heart disease may be advised to follow a heart-healthy diet and exercise regularly.
Applications of Genetic Testing and Personalized Medicine in Specific Chronic Diseases
-
Cardiovascular Disease: Genetic testing can identify individuals at increased risk of developing heart disease, such as those with familial hypercholesterolemia or hypertrophic cardiomyopathy. Pharmacogenomics can guide the selection of appropriate medications, such as statins or antiplatelet drugs, based on an individual’s genetic profile.
-
Cancer: Genetic testing plays a crucial role in cancer risk assessment, diagnosis, prognosis, and treatment selection. Genetic testing can identify individuals with a higher risk of developing breast cancer, ovarian cancer, or colon cancer. Targeted therapies are increasingly used in cancer treatment, and genetic testing can identify individuals who are more likely to benefit from these therapies.
-
Diabetes: Genetic testing can identify individuals at increased risk of developing type 2 diabetes. Pharmacogenomics can guide the selection of appropriate medications, such as metformin or sulfonylureas, based on an individual’s genetic profile.
-
Neurodegenerative Disorders: Genetic testing can aid in the diagnosis of neurodegenerative disorders, such as Alzheimer’s disease and Parkinson’s disease. Genetic testing can also provide information about the likely course of these diseases.
Challenges and Opportunities
While genetic testing and personalized medicine hold great promise for improving the management of chronic diseases, there are also challenges to their implementation in clinical practice.
- Cost: Genetic testing can be expensive, which may limit its accessibility to some patients.
- Data Interpretation: Interpreting genetic data can be complex, and healthcare professionals may need specialized training to understand and apply this information.
- Ethical Considerations: Genetic testing raises ethical concerns about privacy, discrimination, and the potential for genetic information to be used to make decisions about individuals without their consent.
- Lack of Awareness: Many healthcare professionals and patients are not fully aware of the potential benefits of genetic testing and personalized medicine.
Despite these challenges, there are also significant opportunities for the future of genetic testing and personalized medicine in chronic diseases.
- Decreasing Costs: The cost of genetic testing is decreasing, which will make it more accessible to a wider range of patients.
- Improved Data Interpretation: Advances in bioinformatics and artificial intelligence are improving the ability to interpret genetic data and translate it into clinically meaningful information.
- Increased Awareness: Efforts are underway to raise awareness among healthcare professionals and patients about the potential benefits of genetic testing and personalized medicine.
- Integration into Clinical Practice: Personalized medicine is increasingly being integrated into clinical practice, with the development of new guidelines and tools to support its implementation.
Conclusion
Genetic testing and personalized medicine are transforming the management of chronic diseases. By providing valuable information about an individual’s risk of developing a disease, the underlying cause of the disease, the likely course of the disease, and the potential response to treatment, genetic testing can guide personalized medical decisions and improve patient outcomes. While there are challenges to the implementation of personalized medicine in clinical practice, the opportunities for the future are significant. As the cost of genetic testing decreases, data interpretation improves, and awareness increases, personalized medicine is poised to play an increasingly important role in the management of chronic diseases.







Leave a Reply