“Mental Health Interventions for Chronic Disease Patients – Part 3: Tailored Approaches, Emerging Strategies, and Future Directions
Related Articles Mental Health Interventions for Chronic Disease Patients – Part 3: Tailored Approaches, Emerging Strategies, and Future Directions
- Ethical Considerations In Chronic Disease Research
- The Impact Of Chronic Illness On Mental Health
- Integrating Mental Health Care In Chronic Disease Clinics – Part 3
- Chronic Disease Surveillance And Epidemiology
- Genetic Testing And Personalized Medicine In Chronic Diseases: A New Era Of Healthcare
Introduction
With great enthusiasm, let’s explore interesting topics related to Mental Health Interventions for Chronic Disease Patients – Part 3: Tailored Approaches, Emerging Strategies, and Future Directions. Come on knit interesting information and provide new insights to readers.
Table of Content
Mental Health Interventions for Chronic Disease Patients – Part 3: Tailored Approaches, Emerging Strategies, and Future Directions
Introduction
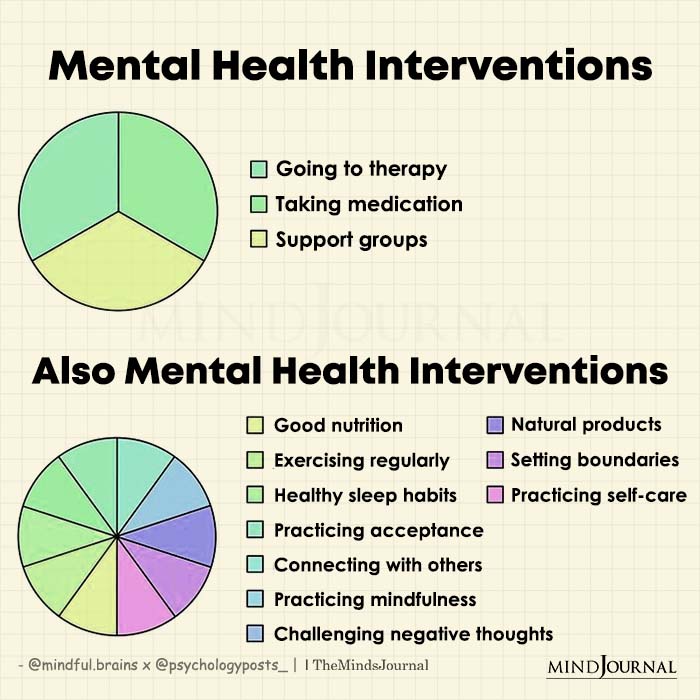
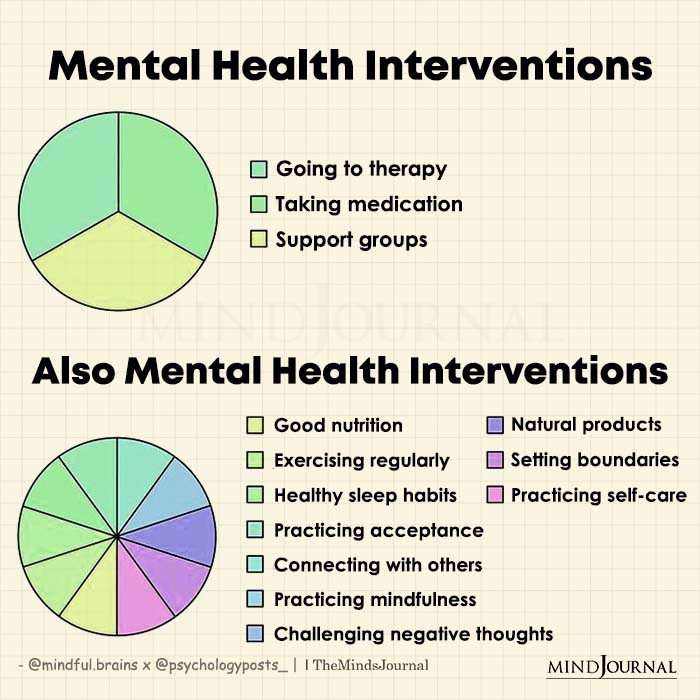
Chronic diseases, such as diabetes, cardiovascular disease, chronic respiratory illnesses, and arthritis, pose a significant global health burden. Beyond the physical challenges, these conditions often lead to substantial mental health issues, including depression, anxiety, and stress. The interplay between chronic illness and mental health is complex and bidirectional. Mental health conditions can exacerbate physical symptoms, reduce treatment adherence, and worsen overall prognosis. Conversely, living with a chronic illness can trigger or worsen mental health problems due to factors like chronic pain, disability, social isolation, and the emotional burden of managing a long-term condition.
Parts 1 and 2 of this series explored the prevalence of mental health issues among chronic disease patients, the impact of these comorbidities, and the rationale for integrated care. We also discussed common barriers to accessing mental health services and foundational interventions like cognitive behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and collaborative care models.
This third and final part delves into more tailored and emerging mental health interventions designed to address the specific needs of individuals living with chronic diseases. We will examine approaches that consider the unique challenges posed by different conditions, explore the potential of digital health technologies, and discuss future directions for research and clinical practice in this critical area.
Tailored Interventions for Specific Chronic Diseases
While general mental health interventions can be beneficial, tailoring approaches to the specific challenges of each chronic disease can enhance their effectiveness.
-
Diabetes: Diabetes distress, a unique form of emotional burden related to managing diabetes, is a common issue. Interventions tailored to diabetes distress often include:
- Problem-solving therapy: Helping patients identify and address specific challenges related to diabetes management, such as meal planning, medication adherence, or managing blood sugar fluctuations.
- Motivational interviewing: Supporting patients in exploring their ambivalence about diabetes management and building intrinsic motivation for self-care behaviors.
- Peer support groups: Connecting patients with others who have diabetes to share experiences, provide emotional support, and learn coping strategies.
-
Cardiovascular Disease: Depression and anxiety are significant risk factors for adverse cardiovascular events. Tailored interventions may include:
- Cardiac rehabilitation programs: Integrating mental health support into cardiac rehabilitation programs to address depression, anxiety, and stress related to heart disease.
- Stress management techniques: Teaching patients relaxation techniques, mindfulness, and other stress-reduction strategies to manage the physiological effects of stress on the cardiovascular system.
- Lifestyle modification counseling: Providing support and guidance to help patients adopt healthy lifestyle behaviors, such as regular exercise, a heart-healthy diet, and smoking cessation, which can improve both physical and mental health.
-
Chronic Respiratory Illnesses (COPD, Asthma): Breathlessness, fatigue, and social isolation are common challenges for individuals with chronic respiratory illnesses. Tailored interventions may include:
- Pulmonary rehabilitation programs: Similar to cardiac rehabilitation, pulmonary rehabilitation programs can integrate mental health support to address depression, anxiety, and breathlessness-related distress.
- Breathing retraining techniques: Teaching patients breathing exercises to improve respiratory function and reduce anxiety associated with breathlessness.
- Activity pacing strategies: Helping patients manage fatigue and conserve energy by pacing their activities and avoiding overexertion.
-
Chronic Pain Conditions (Arthritis, Fibromyalgia): Chronic pain can significantly impact mental health, leading to depression, anxiety, and disability. Tailored interventions may include:
- Cognitive behavioral therapy for chronic pain (CBT-CP): A specialized form of CBT that helps patients manage pain by addressing negative thoughts, beliefs, and behaviors related to pain.
- Acceptance and commitment therapy (ACT): Helping patients accept chronic pain as a part of their lives and commit to engaging in meaningful activities despite their pain.
- Mindfulness-based pain management (MBPM): Teaching patients mindfulness techniques to observe and accept pain sensations without judgment, reducing emotional reactivity to pain.
Emerging Strategies and Technologies
Advances in technology and innovative approaches are expanding the possibilities for delivering mental health interventions to chronic disease patients.
-
Digital Health Interventions:
- Mobile apps: Mobile apps can provide access to mental health resources, self-monitoring tools, and guided interventions for depression, anxiety, and stress management. Apps can also be tailored to specific chronic diseases, offering support for medication adherence, lifestyle modification, and symptom management.
- Telehealth: Telehealth allows patients to access mental health services remotely via video conferencing or phone calls. This can be particularly beneficial for individuals in rural areas, those with mobility limitations, or those who prefer the convenience of receiving care from home.
- Wearable sensors: Wearable sensors can track physiological data, such as heart rate, sleep patterns, and activity levels, providing insights into the relationship between physical and mental health. This data can be used to personalize interventions and track progress over time.
-
Integrated Care Models:
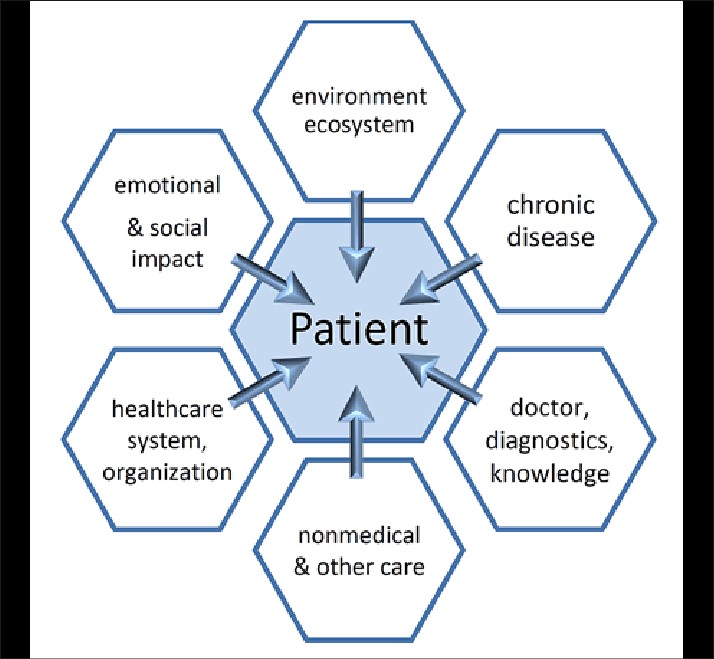
- Primary care integration: Integrating mental health services into primary care settings can improve access to care and reduce stigma. This can involve training primary care providers to screen for mental health issues and provide brief interventions, or co-locating mental health professionals in primary care clinics.
- Specialty care integration: Integrating mental health services into specialty care settings, such as cardiology or endocrinology clinics, can address the specific mental health needs of patients with chronic diseases. This can involve collaboration between medical specialists and mental health professionals to develop integrated treatment plans.
-
Personalized Medicine Approaches:
- Genetic testing: Genetic testing may help identify individuals who are at higher risk for developing mental health problems in response to chronic illness. This information can be used to target preventive interventions to those who are most likely to benefit.
- Biomarker research: Research on biomarkers, such as inflammatory markers or stress hormones, may help identify objective measures of mental health status in chronic disease patients. This could lead to more precise and personalized treatment approaches.
Future Directions
The field of mental health interventions for chronic disease patients is rapidly evolving, with several promising directions for future research and clinical practice.
-
Implementation Science:
- Dissemination and implementation research: More research is needed to understand how to effectively disseminate and implement evidence-based mental health interventions in real-world clinical settings. This includes identifying barriers to implementation and developing strategies to overcome them.
- Cost-effectiveness analysis: Conducting cost-effectiveness analyses of different mental health interventions can help inform resource allocation decisions and ensure that interventions are delivered in the most efficient and sustainable way.
-
Technology Development:
- Artificial intelligence (AI): AI has the potential to personalize mental health interventions and provide real-time support to chronic disease patients. AI-powered chatbots, for example, can provide automated counseling and support, while machine learning algorithms can predict which patients are most likely to benefit from specific interventions.
- Virtual reality (VR): VR can be used to create immersive and engaging experiences that promote relaxation, reduce anxiety, and improve coping skills. VR interventions have shown promise in managing chronic pain, reducing social isolation, and improving adherence to treatment.
-
Prevention and Early Intervention:
- Proactive screening: Implementing routine screening for mental health issues in chronic disease patients can help identify problems early and prevent them from becoming more severe.
- Resilience-building interventions: Developing interventions that focus on building resilience and coping skills can help individuals better manage the emotional challenges of living with a chronic illness.
-
Addressing Health Disparities:
- Culturally tailored interventions: Developing culturally tailored mental health interventions that are sensitive to the needs and preferences of diverse populations is essential to reduce health disparities.
- Community-based approaches: Engaging community-based organizations and leaders can help improve access to mental health services for underserved populations.
Conclusion
Mental health interventions are a crucial component of comprehensive care for individuals living with chronic diseases. Tailoring interventions to the specific challenges of each condition, leveraging emerging technologies, and focusing on prevention and early intervention can improve outcomes and enhance quality of life. As research continues to advance and new approaches are developed, the future of mental health care for chronic disease patients holds great promise. By prioritizing mental health and integrating it into routine medical care, we can empower individuals to live healthier, more fulfilling lives despite the challenges of chronic illness.






Leave a Reply