“Bone Health and Chronic Kidney Disease
Related Articles Bone Health and Chronic Kidney Disease
- Bone Health In Elderly Populations: Concerns And Care
- The Intricate Link Between Vitamin D Deficiency And Bone Health
- Environmental Factors Affecting Bone Density
- Dental Health And Bone Density: Interconnections
- Understanding Bone Fractures: Types, Causes, And Treatment
Introduction
With great enthusiasm, let’s explore interesting topics related to Bone Health and Chronic Kidney Disease. Let’s knit interesting information and provide new insights to readers.
Table of Content
Bone Health and Chronic Kidney Disease

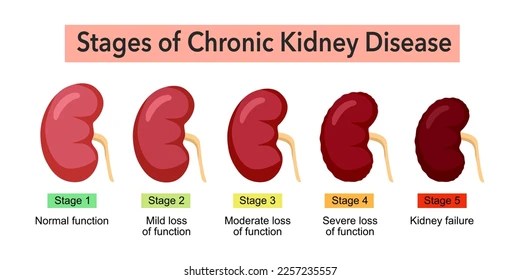
Chronic kidney disease (CKD) is a progressive condition characterized by a gradual loss of kidney function over time. While the primary concern with CKD is often related to the kidneys’ inability to filter waste and regulate fluids, the disease also has significant effects on other systems in the body, including the skeletal system. Bone health is frequently compromised in individuals with CKD, leading to a condition known as chronic kidney disease-mineral and bone disorder (CKD-MBD). This disorder encompasses a range of abnormalities in mineral metabolism, bone turnover, and skeletal structure, resulting in increased risks of fractures, cardiovascular complications, and reduced quality of life.
Understanding the Link Between CKD and Bone Health
To comprehend the impact of CKD on bone health, it is essential to understand the intricate relationship between the kidneys and skeletal system. The kidneys play a crucial role in maintaining mineral homeostasis, particularly calcium and phosphorus balance, which are vital for bone health. In addition, the kidneys are responsible for activating vitamin D, a hormone that promotes calcium absorption in the gut and regulates bone turnover.
As kidney function declines in CKD, several factors contribute to the development of CKD-MBD:
-
Phosphorus Retention: The kidneys normally excrete excess phosphorus in the urine. In CKD, the kidneys’ ability to eliminate phosphorus is impaired, leading to hyperphosphatemia, or elevated phosphorus levels in the blood. High phosphorus levels trigger the release of parathyroid hormone (PTH), which attempts to restore phosphorus balance by increasing bone resorption, the process by which bone is broken down to release calcium and phosphorus into the bloodstream.
-
Vitamin D Deficiency: The kidneys are responsible for converting inactive vitamin D into its active form, calcitriol. In CKD, the kidneys’ ability to activate vitamin D is diminished, resulting in vitamin D deficiency. Vitamin D deficiency reduces calcium absorption from the gut, further stimulating PTH secretion and bone resorption.
-
Calcium Imbalance: CKD can lead to both hypocalcemia (low calcium levels) and hypercalcemia (high calcium levels). Hypocalcemia is often caused by vitamin D deficiency and impaired calcium absorption. Hypercalcemia can occur in advanced CKD due to excessive bone resorption or the use of calcium-based phosphate binders.
-
Parathyroid Hormone (PTH) Dysregulation: As mentioned earlier, PTH plays a central role in CKD-MBD. In response to hyperphosphatemia and vitamin D deficiency, the parathyroid glands become overactive and secrete excessive amounts of PTH, leading to secondary hyperparathyroidism. Chronic elevation of PTH can result in high-turnover bone disease, characterized by accelerated bone resorption and formation, but with structurally abnormal bone.
-
Fibroblast Growth Factor 23 (FGF23): FGF23 is a hormone produced by bone cells that regulates phosphorus and vitamin D metabolism. In early CKD, FGF23 levels increase to promote phosphorus excretion by the kidneys. However, as CKD progresses, the kidneys become less responsive to FGF23, leading to further phosphorus retention and suppression of vitamin D activation.
-
Acidosis: CKD can cause metabolic acidosis, a condition in which the body’s pH becomes too acidic. Chronic acidosis can contribute to bone loss by stimulating bone resorption to buffer the excess acid.
-
Inflammation: CKD is associated with chronic inflammation, which can have detrimental effects on bone health. Inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), can stimulate bone resorption and inhibit bone formation.
Consequences of CKD-MBD
CKD-MBD has significant consequences for individuals with CKD, including:
-
Increased Fracture Risk: The most well-known consequence of CKD-MBD is an increased risk of fractures. CKD-related bone abnormalities, such as low bone mineral density and abnormal bone structure, make bones more fragile and susceptible to fractures, even from minor trauma. Fractures can lead to pain, disability, and reduced quality of life.
-
Cardiovascular Complications: CKD-MBD is also associated with an increased risk of cardiovascular complications, such as vascular calcification and cardiovascular events. Elevated phosphorus levels and PTH can promote calcification of blood vessels, leading to stiffening of the arteries and increased risk of heart attack, stroke, and peripheral artery disease.
-
Bone Pain and Muscle Weakness: CKD-MBD can cause bone pain and muscle weakness, which can significantly impair physical function and quality of life. Bone pain may be caused by increased bone turnover and microfractures. Muscle weakness can result from vitamin D deficiency, electrolyte imbalances, and uremic toxins.
-
Growth Retardation in Children: Children with CKD are particularly vulnerable to the effects of CKD-MBD, as it can impair bone growth and development, leading to growth retardation and skeletal deformities.
Diagnosis of CKD-MBD
Diagnosing CKD-MBD involves a combination of clinical assessment, laboratory testing, and imaging studies.
-
Clinical Assessment: Healthcare providers will evaluate patients for symptoms of CKD-MBD, such as bone pain, muscle weakness, fractures, and cardiovascular disease. They will also inquire about risk factors for CKD-MBD, such as age, gender, race, and history of fractures.
-
Laboratory Testing: Laboratory tests are essential for assessing mineral metabolism and bone turnover in CKD patients. Key laboratory tests include:
- Serum Phosphorus: Measures the level of phosphorus in the blood.
- Serum Calcium: Measures the level of calcium in the blood.
- Parathyroid Hormone (PTH): Measures the level of PTH in the blood.
- Vitamin D (25-hydroxyvitamin D): Measures the level of vitamin D in the blood.
- Alkaline Phosphatase: Measures the level of alkaline phosphatase, an enzyme that is elevated in bone disorders.
- Fibroblast Growth Factor 23 (FGF23): Measures the level of FGF23 in the blood.
-
Imaging Studies: Imaging studies, such as bone densitometry (DEXA scan), can be used to assess bone mineral density and fracture risk. DEXA scans measure the density of bone in the spine and hip, which are common sites of fractures.
Management of CKD-MBD
The management of CKD-MBD aims to correct mineral imbalances, control PTH levels, prevent fractures, and reduce cardiovascular risk. Treatment strategies include:
-
Dietary Phosphorus Restriction: Limiting phosphorus intake through diet is a cornerstone of CKD-MBD management. Patients are advised to avoid foods high in phosphorus, such as dairy products, processed foods, and dark-colored sodas.
-
Phosphate Binders: Phosphate binders are medications that bind to phosphorus in the gut, preventing its absorption into the bloodstream. Phosphate binders are typically taken with meals to maximize their effectiveness. Different types of phosphate binders are available, including calcium-based binders, non-calcium-based binders (such as sevelamer and lanthanum), and iron-based binders.
-
Vitamin D Supplementation: Vitamin D supplementation is often necessary to correct vitamin D deficiency and improve calcium absorption. Calcitriol, the active form of vitamin D, is commonly prescribed for CKD patients. Other vitamin D analogs, such as paricalcitol and doxercalciferol, are also available.
-
Calcimimetics: Calcimimetics are medications that mimic the effects of calcium on the parathyroid glands, suppressing PTH secretion. Cinacalcet is a commonly used calcimimetic.
-
Parathyroidectomy: In severe cases of secondary hyperparathyroidism that are unresponsive to medical management, parathyroidectomy (surgical removal of the parathyroid glands) may be considered.
-
Dialysis Management: Optimizing dialysis regimens can help improve mineral balance and reduce the risk of CKD-MBD. Frequent or extended dialysis sessions can remove more phosphorus from the blood.
-
Bisphosphonates and Other Bone-Specific Therapies: Bisphosphonates are medications that inhibit bone resorption and increase bone mineral density. While bisphosphonates are commonly used to treat osteoporosis, their use in CKD patients is controversial due to concerns about potential side effects, such as adynamic bone disease (a condition in which bone turnover is suppressed too much) and atypical fractures. Other bone-specific therapies, such as denosumab, may also be considered in select CKD patients.
-
Lifestyle Modifications: Lifestyle modifications, such as regular exercise and smoking cessation, can also help improve bone health in CKD patients. Weight-bearing exercises can stimulate bone formation and increase bone mineral density.
Conclusion
CKD-MBD is a common and serious complication of chronic kidney disease that can have significant consequences for bone health, cardiovascular health, and overall quality of life. Early diagnosis and management of CKD-MBD are essential to prevent fractures, reduce cardiovascular risk, and improve outcomes for individuals with CKD. Healthcare providers should routinely monitor mineral metabolism and bone turnover in CKD patients and implement appropriate treatment strategies to correct imbalances and protect bone health.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.







Leave a Reply