“Does Your Blood Type Affect Your Heart Disease Risk?
Related Articles Does Your Blood Type Affect Your Heart Disease Risk?
- Comorbidities Associated With Common Chronic Diseases – Part 4
- Lifestyle Changes To Manage Chronic Conditions – Part 9
- The Role Of Gut Microbiome In Heart Disease: A Comprehensive Overview
- Preventive Screening Guidelines For Chronic Conditions: A Comprehensive Overview
- Psychological Resilience In Chronic Disease Patients – Part 3: Strategies For Cultivating Resilience And Supporting Thriving
Introduction
We will be happy to explore interesting topics related to Does Your Blood Type Affect Your Heart Disease Risk?. Let’s knit interesting information and provide new insights to readers.
Table of Content
Does Your Blood Type Affect Your Heart Disease Risk?
Heart disease is a leading cause of death worldwide, affecting millions of people each year. While factors like diet, exercise, and genetics are well-established contributors to heart health, emerging research suggests that your blood type may also play a role in your risk of developing heart disease. In this comprehensive article, we will delve into the fascinating connection between blood type and heart disease, exploring the science behind this association, the specific blood types that may be at higher risk, and the implications for prevention and management.
Understanding Blood Types
Before we explore the link between blood type and heart disease, it’s essential to understand the basics of blood typing. Blood types are classified based on the presence or absence of specific antigens on the surface of red blood cells. The two main blood group systems are the ABO system and the Rh system.
- ABO System: The ABO system categorizes blood into four main types: A, B, AB, and O. These types are determined by the presence or absence of A and B antigens on red blood cells. Individuals with type A blood have A antigens, those with type B blood have B antigens, those with type AB blood have both A and B antigens, and those with type O blood have neither A nor B antigens.
- Rh System: The Rh system is determined by the presence or absence of the Rh factor, also known as the D antigen. Individuals with the Rh factor are considered Rh-positive (Rh+), while those without it are Rh-negative (Rh-).
Therefore, a person’s blood type is typically described using both the ABO and Rh systems, such as A+, A-, B+, B-, AB+, AB-, O+, or O-.
The Connection Between Blood Type and Heart Disease Risk
Over the years, numerous studies have investigated the association between blood type and the risk of developing heart disease. The results of these studies have revealed some intriguing patterns, suggesting that certain blood types may be associated with a higher or lower risk of cardiovascular issues.
1. Non-O Blood Types and Increased Risk
Several studies have consistently found that individuals with non-O blood types (A, B, and AB) may have a higher risk of developing heart disease compared to those with type O blood. This association has been observed in various populations and across different types of heart conditions.
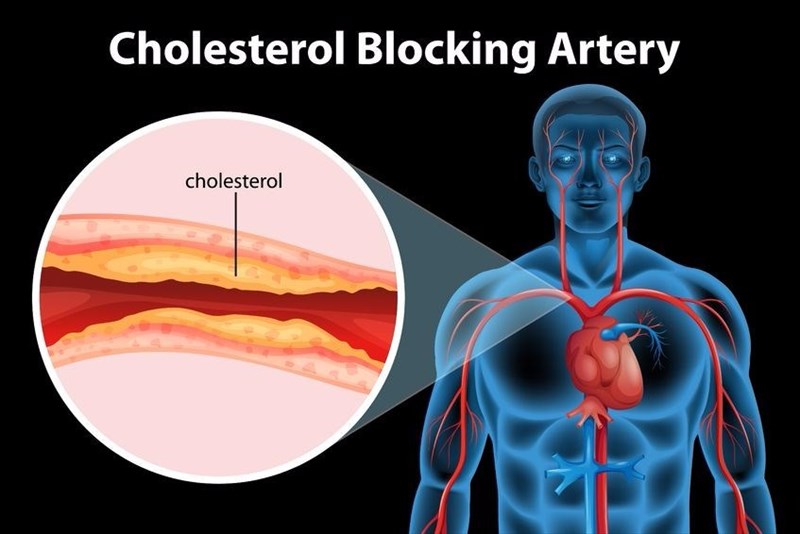
a. Coronary Artery Disease (CAD): Coronary artery disease, also known as ischemic heart disease, is the most common type of heart disease. It occurs when the arteries that supply blood to the heart become narrowed or blocked, typically due to the buildup of plaque (atherosclerosis). Research has indicated that individuals with non-O blood types may have a higher risk of developing CAD.
b. Myocardial Infarction (Heart Attack): A myocardial infarction, commonly known as a heart attack, occurs when blood flow to the heart muscle is suddenly blocked, leading to damage or death of heart tissue. Studies have suggested that non-O blood types may be associated with an increased risk of heart attack.
c. Heart Failure: Heart failure is a chronic condition in which the heart is unable to pump enough blood to meet the body’s needs. Research has indicated that individuals with non-O blood types may have a higher risk of developing heart failure.
2. Potential Mechanisms Behind the Association
The exact mechanisms by which blood type may influence heart disease risk are not fully understood, but several potential factors have been proposed:
a. von Willebrand Factor (vWF): von Willebrand factor is a protein involved in blood clotting. Studies have shown that individuals with non-O blood types tend to have higher levels of vWF in their blood. Elevated vWF levels can increase the risk of blood clot formation, which can contribute to the development of heart disease.
b. Inflammation: Inflammation plays a significant role in the development of atherosclerosis and other cardiovascular conditions. Research has suggested that non-O blood types may be associated with higher levels of inflammatory markers in the blood, potentially contributing to an increased risk of heart disease.
c. Cholesterol Levels: Cholesterol is a fatty substance that can accumulate in the arteries, leading to plaque formation. Some studies have indicated that non-O blood types may be associated with higher levels of LDL cholesterol (the "bad" cholesterol), which can increase the risk of heart disease.
d. Gut Microbiome: The gut microbiome, the community of microorganisms living in the digestive tract, can influence various aspects of health, including cardiovascular health. Emerging research suggests that blood type may affect the composition of the gut microbiome, potentially impacting heart disease risk.
3. Specific Blood Types and Risk Levels
While non-O blood types, in general, have been associated with a higher risk of heart disease, some studies have explored the specific risk levels associated with each blood type:
a. Type A Blood: Type A blood has been linked to a slightly increased risk of CAD and heart attack compared to type O blood. This may be due to the higher levels of LDL cholesterol and inflammatory markers often observed in individuals with type A blood.
b. Type B Blood: Type B blood has also been associated with a slightly increased risk of heart disease, particularly heart failure. This may be related to the influence of type B blood on the gut microbiome and its potential impact on inflammation.
c. Type AB Blood: Type AB blood is the least common blood type and has been associated with the highest risk of heart disease among the non-O blood types. Individuals with type AB blood may have a higher risk of CAD, heart attack, and heart failure. This may be due to the combined effects of the A and B antigens on vWF levels, inflammation, and cholesterol levels.
4. Limitations and Future Research
It’s important to note that while the association between blood type and heart disease risk is intriguing, it’s not a definitive cause-and-effect relationship. Several limitations and areas for future research exist:
- Observational Studies: Most studies on blood type and heart disease are observational, meaning they can identify associations but cannot prove causation.
- Confounding Factors: The association between blood type and heart disease may be influenced by other factors, such as genetics, lifestyle, and environmental exposures.
- Heterogeneity: The results of studies may vary depending on the population studied, the type of heart disease investigated, and the methods used.
- Mechanism of Action: The exact mechanisms by which blood type influences heart disease risk need further investigation.
Future research should focus on addressing these limitations and exploring the underlying mechanisms of the association between blood type and heart disease. This may involve conducting large-scale, prospective studies, investigating the role of genetics and lifestyle factors, and exploring the potential for targeted interventions based on blood type.
Implications for Prevention and Management
While you cannot change your blood type, understanding its potential influence on heart disease risk can inform preventive measures and management strategies:
1. Lifestyle Modifications: Regardless of your blood type, adopting a heart-healthy lifestyle is crucial for preventing heart disease. This includes:
- Healthy Diet: Consume a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit your intake of saturated and trans fats, cholesterol, sodium, and added sugars.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week.
- Weight Management: Maintain a healthy weight to reduce your risk of heart disease.
- Smoking Cessation: Quit smoking to significantly reduce your risk of heart disease and other health problems.
- Stress Management: Practice stress-reducing techniques, such as yoga, meditation, or spending time in nature.
2. Regular Check-ups: If you have a non-O blood type, it’s essential to have regular check-ups with your healthcare provider to monitor your heart health. This may include blood pressure measurements, cholesterol screening, and other tests as needed.
3. Early Detection and Treatment: If you have a family history of heart disease or other risk factors, your healthcare provider may recommend early screening for heart disease. Early detection and treatment can help prevent or delay the progression of heart disease.
4. Personalized Approaches: As research on blood type and heart disease progresses, it may be possible to develop personalized prevention and treatment strategies based on an individual’s blood type. This could involve tailoring dietary recommendations, exercise plans, or medication regimens to optimize heart health.
Conclusion
The association between blood type and heart disease risk is a fascinating area of research that has revealed some intriguing patterns. While individuals with non-O blood types (A, B, and AB) may have a slightly higher risk of developing heart disease compared to those with type O blood, it’s important to remember that blood type is just one factor among many that contribute to heart health.
Regardless of your blood type, adopting a heart-healthy lifestyle, having regular check-ups, and seeking early detection and treatment are crucial for preventing and managing heart disease. As research continues to unravel the complex interplay between blood type, genetics, lifestyle, and heart health, it may be possible to develop more personalized approaches to prevention and treatment, ultimately reducing the burden of heart disease worldwide.








Leave a Reply