“The Role of Magnesium in Cardiovascular Function
Related Articles The Role of Magnesium in Cardiovascular Function
- Integrative Oncology Approaches In Leukemia Care
- Patient Empowerment In Chronic Disease Management: Part 4 – Leveraging Technology, Building Communities, And Navigating The Future
- Cardiovascular Complications Of COVID-19
- Integrative Medicine In Chronic Disease Care – Part 8: Integrative Approaches To Autoimmune Disorders
- Disability Rights And Advocacy For Chronic Disease Patients
Introduction
With great enthusiasm, let’s explore interesting topics related to The Role of Magnesium in Cardiovascular Function. Come on knit interesting information and provide new insights to readers.
Table of Content
The Role of Magnesium in Cardiovascular Function

Introduction
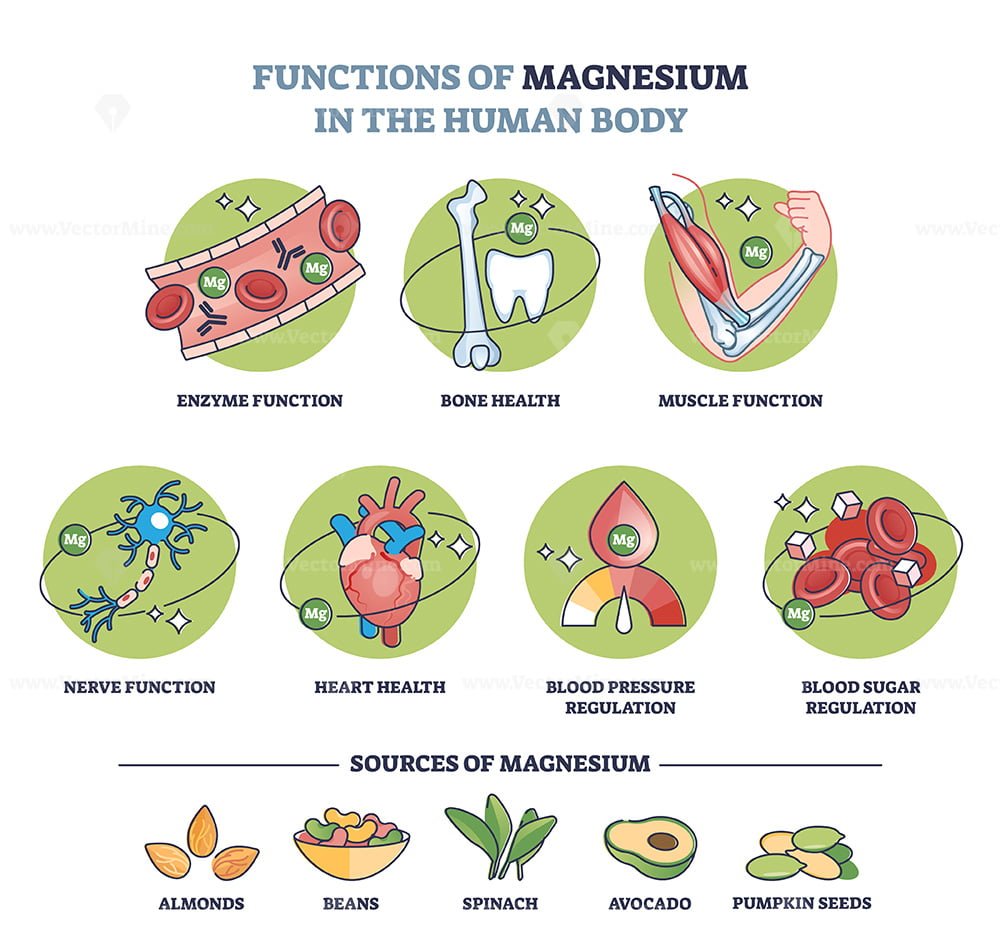
Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality worldwide. While traditional risk factors such as hypertension, hyperlipidemia, diabetes, and smoking are well-established, emerging evidence highlights the critical role of micronutrients, particularly magnesium, in maintaining cardiovascular health. Magnesium, an essential mineral involved in over 300 enzymatic reactions in the body, is crucial for various physiological processes, including muscle function, nerve transmission, blood glucose control, and blood pressure regulation. This article explores the multifaceted roles of magnesium in cardiovascular function, the impact of magnesium deficiency, and the potential benefits of magnesium supplementation.
Magnesium: An Overview
Magnesium (Mg) is the fourth most abundant mineral in the human body and is essential for maintaining overall health. It plays a vital role in:
- Enzymatic Reactions: Magnesium is a cofactor for numerous enzymes involved in energy production, DNA and RNA synthesis, and protein synthesis.
- Muscle Function: It is crucial for muscle contraction and relaxation, including the heart muscle.
- Nerve Function: Magnesium helps regulate nerve transmission and neuromuscular conduction.
- Bone Health: It contributes to bone structure and mineralization.
- Blood Glucose Control: Magnesium influences insulin secretion and action, impacting blood sugar levels.
- Blood Pressure Regulation: It helps maintain healthy blood vessel function and blood pressure levels.
Magnesium and Blood Pressure Regulation
Hypertension is a significant risk factor for CVD, including heart attack, stroke, and kidney disease. Magnesium plays a crucial role in regulating blood pressure through several mechanisms:
- Vasodilation: Magnesium acts as a natural calcium channel blocker, promoting vasodilation (relaxation of blood vessels). This reduces peripheral vascular resistance and lowers blood pressure.
- Endothelial Function: Magnesium supports the health and function of the endothelium, the inner lining of blood vessels. A healthy endothelium produces nitric oxide (NO), a potent vasodilator that helps maintain blood pressure.
- Sodium and Potassium Balance: Magnesium influences the transport of sodium and potassium ions across cell membranes, which is essential for maintaining proper fluid balance and blood pressure.
- Renin-Angiotensin-Aldosterone System (RAAS) Modulation: Magnesium can modulate the RAAS, a hormonal system that regulates blood pressure and fluid balance. By inhibiting the RAAS, magnesium helps prevent sodium and water retention, thereby lowering blood pressure.
Magnesium and Arrhythmias
Cardiac arrhythmias, or irregular heartbeats, can range from benign to life-threatening. Magnesium is essential for maintaining proper electrical activity in the heart and preventing arrhythmias.
- Electrolyte Balance: Magnesium helps maintain the balance of other electrolytes, such as potassium and calcium, which are critical for cardiac electrophysiology.
- Ion Channel Function: Magnesium influences the function of ion channels in heart cells, including potassium, sodium, and calcium channels. These channels are responsible for generating and conducting electrical impulses in the heart.
- Action Potential Duration: Magnesium affects the duration of the action potential in heart cells, which is the electrical signal that triggers muscle contraction. By shortening the action potential, magnesium helps prevent arrhythmias.
- Atrial Fibrillation (AFib): Studies have shown that magnesium supplementation can reduce the risk of AFib, a common type of arrhythmia that increases the risk of stroke and heart failure.
Magnesium and Atherosclerosis
Atherosclerosis, the buildup of plaque in the arteries, is a leading cause of CVD. Magnesium may help prevent or slow the progression of atherosclerosis through several mechanisms:
- Inflammation: Magnesium has anti-inflammatory properties that can help reduce chronic inflammation in the arteries, a key factor in the development of atherosclerosis.
- Oxidative Stress: Magnesium acts as an antioxidant, protecting LDL cholesterol from oxidation. Oxidized LDL cholesterol is more likely to accumulate in the arteries and contribute to plaque formation.
- Platelet Aggregation: Magnesium can inhibit platelet aggregation, reducing the risk of blood clot formation in the arteries.
- Endothelial Function: By supporting endothelial function, magnesium helps maintain the integrity of the arterial walls and prevent plaque buildup.
Magnesium and Heart Failure
Heart failure is a chronic condition in which the heart is unable to pump enough blood to meet the body’s needs. Magnesium deficiency is common in patients with heart failure and can worsen the condition.
- Cardiac Contractility: Magnesium is essential for proper cardiac contractility, the ability of the heart muscle to contract and pump blood effectively.
- Ventricular Remodeling: Magnesium may help prevent ventricular remodeling, the structural changes that occur in the heart in response to chronic stress or injury.
- Arrhythmias: Magnesium deficiency can increase the risk of arrhythmias, which can further impair heart function in patients with heart failure.
- Endothelial Function: Magnesium supports endothelial function, which is crucial for maintaining blood flow and oxygen delivery to the heart muscle.
Magnesium Deficiency and Cardiovascular Risk
Magnesium deficiency is more common than previously thought, with many individuals not meeting the recommended daily intake. Several factors can contribute to magnesium deficiency:
- Dietary Factors: A diet low in magnesium-rich foods, such as green leafy vegetables, nuts, seeds, and whole grains, can lead to deficiency.
- Medications: Certain medications, such as diuretics, proton pump inhibitors (PPIs), and some antibiotics, can increase magnesium excretion and lead to deficiency.
- Gastrointestinal Disorders: Conditions such as Crohn’s disease, ulcerative colitis, and celiac disease can impair magnesium absorption.
- Chronic Diseases: Diabetes, kidney disease, and alcoholism can increase the risk of magnesium deficiency.
- Age: Older adults are more likely to be magnesium deficient due to decreased absorption and increased excretion.
Magnesium deficiency has been linked to an increased risk of several cardiovascular conditions:
- Hypertension: Low magnesium levels can contribute to elevated blood pressure.
- Arrhythmias: Magnesium deficiency can increase the risk of arrhythmias, including atrial fibrillation and ventricular arrhythmias.
- Atherosclerosis: Low magnesium levels may promote inflammation and oxidative stress, contributing to the development of atherosclerosis.
- Heart Failure: Magnesium deficiency can worsen cardiac function and increase the risk of complications in patients with heart failure.
Magnesium Supplementation: Benefits and Considerations
Magnesium supplementation may be beneficial for individuals with magnesium deficiency or those at high risk of CVD. Studies have shown that magnesium supplementation can:
- Lower Blood Pressure: Magnesium supplementation has been shown to lower blood pressure in individuals with hypertension.
- Reduce Arrhythmias: Magnesium supplementation can reduce the risk of arrhythmias, particularly atrial fibrillation.
- Improve Endothelial Function: Magnesium supplementation can improve endothelial function and reduce inflammation in the arteries.
- Enhance Insulin Sensitivity: Magnesium supplementation may improve insulin sensitivity and blood glucose control, which can reduce the risk of diabetes and CVD.
However, it is essential to consider the following when considering magnesium supplementation:
- Form of Magnesium: Different forms of magnesium supplements have varying bioavailability. Magnesium citrate, magnesium glycinate, and magnesium chloride are generally well-absorbed.
- Dosage: The recommended daily intake of magnesium is 400-420 mg for men and 310-320 mg for women. However, individual needs may vary.
- Side Effects: High doses of magnesium can cause gastrointestinal side effects, such as diarrhea.
- Drug Interactions: Magnesium can interact with certain medications, such as antibiotics and bisphosphonates.
- Consultation with Healthcare Provider: It is essential to consult with a healthcare provider before starting magnesium supplementation, especially if you have underlying health conditions or are taking medications.
Dietary Sources of Magnesium
Increasing dietary intake of magnesium-rich foods is a safe and effective way to improve magnesium status. Excellent sources of magnesium include:
- Green Leafy Vegetables: Spinach, kale, and collard greens
- Nuts and Seeds: Almonds, cashews, pumpkin seeds, and sunflower seeds
- Whole Grains: Brown rice, quinoa, and oats
- Legumes: Black beans, kidney beans, and lentils
- Avocados
- Dark Chocolate
Conclusion
Magnesium plays a critical role in maintaining cardiovascular health. It helps regulate blood pressure, prevent arrhythmias, reduce inflammation, and improve endothelial function. Magnesium deficiency is common and can increase the risk of CVD. Magnesium supplementation may be beneficial for individuals with deficiency or those at high risk of CVD. However, it is essential to consult with a healthcare provider before starting supplementation. Increasing dietary intake of magnesium-rich foods is a safe and effective way to improve magnesium status and support cardiovascular health.
By understanding the multifaceted roles of magnesium in cardiovascular function, healthcare professionals and individuals can take proactive steps to ensure adequate magnesium intake and reduce the risk of CVD. Further research is needed to fully elucidate the mechanisms by which magnesium affects cardiovascular health and to determine the optimal strategies for magnesium supplementation in different populations.







Leave a Reply