“Blood Clots and Their Relationship to the Heart
Related Articles Blood Clots and Their Relationship to the Heart
- Cultural Perspectives On Chronic Disease Management – Part 3
- Chronic Disease Trends In Aging Populations – Part 2
- Social Determinants Of Health And Chronic Disease Outcomes – Part 9
- Dietary Strategies For Coping With Chronic Diseases – Part 10
- Palliative Care And Quality Of Life For Chronic Illness Patients – Part 8: Ethical Considerations In Palliative Care
Introduction
With great enthusiasm, let’s explore interesting topics related to Blood Clots and Their Relationship to the Heart. Come on knit interesting information and provide new insights to readers.
Table of Content
Blood Clots and Their Relationship to the Heart
Blood clots are a natural and essential process in the body that helps to stop bleeding when a blood vessel is injured. However, when blood clots form inappropriately or in the wrong location, they can pose serious health risks, especially when they affect the heart. Understanding the relationship between blood clots and the heart is crucial for preventing and managing cardiovascular conditions.
The Formation of Blood Clots
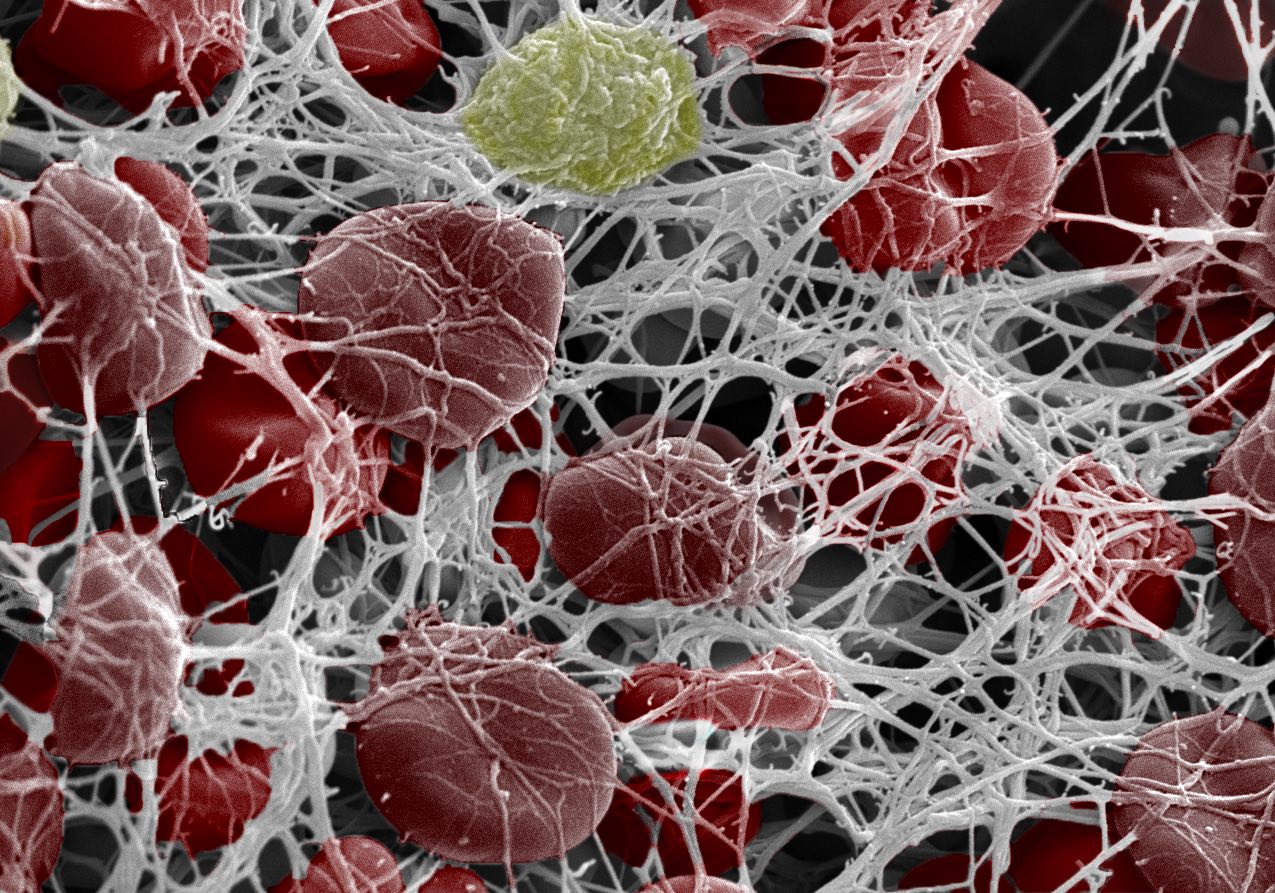
Blood clotting, also known as coagulation, is a complex process that involves various components in the blood, including platelets, clotting factors, and proteins. When a blood vessel is damaged, platelets rush to the site of injury and begin to clump together, forming a temporary plug. This process is called primary hemostasis.
Next, a cascade of reactions involving clotting factors occurs, leading to the formation of fibrin strands. Fibrin acts as a mesh-like structure that reinforces the platelet plug, creating a stable blood clot. This process is called secondary hemostasis.
Once the blood vessel has healed, the clot is no longer needed, and the body initiates a process called fibrinolysis to break down the clot. This process ensures that blood flow is restored and that the clot does not continue to grow or travel to other parts of the body.
The Heart’s Vulnerability to Blood Clots
The heart is a vital organ responsible for pumping blood throughout the body. It relies on a constant supply of oxygen and nutrients to function properly. The heart’s vulnerability to blood clots arises from its intricate network of blood vessels, including the coronary arteries, which supply blood to the heart muscle itself.
When a blood clot forms in a coronary artery, it can obstruct blood flow to the heart muscle, leading to a condition called myocardial infarction, commonly known as a heart attack. A heart attack can cause irreversible damage to the heart muscle and can be life-threatening.
In addition to the coronary arteries, blood clots can also form in the heart chambers, such as the atria or ventricles. These clots can break loose and travel to other parts of the body, causing a stroke if they block blood flow to the brain or pulmonary embolism if they lodge in the lungs.
Conditions That Increase the Risk of Blood Clots in the Heart
Several factors and conditions can increase the risk of blood clots forming in the heart or traveling to the heart from other parts of the body. These include:
-
Atrial Fibrillation (AFib): AFib is a common heart rhythm disorder characterized by irregular and rapid heartbeats. In AFib, the atria (upper chambers of the heart) quiver instead of contracting effectively, which can lead to blood pooling and clot formation.
-
Heart Valve Disorders: Conditions such as mitral valve stenosis or aortic valve stenosis can disrupt normal blood flow through the heart, increasing the risk of clot formation.
-
Cardiomyopathy: Cardiomyopathy is a condition in which the heart muscle becomes enlarged, thickened, or stiff. This can impair the heart’s ability to pump blood effectively, leading to blood pooling and clot formation.
-
Congenital Heart Defects: Some congenital heart defects can alter blood flow patterns in the heart, increasing the risk of clot formation.
-
Deep Vein Thrombosis (DVT): DVT is a condition in which blood clots form in the deep veins, usually in the legs. These clots can break loose and travel to the heart, potentially causing a pulmonary embolism.
-
Pulmonary Embolism (PE): PE occurs when a blood clot travels to the lungs and blocks a pulmonary artery. This can strain the heart and increase the risk of further clot formation.
-
Coronary Artery Disease (CAD): CAD is characterized by the buildup of plaque in the coronary arteries, which can lead to blood clot formation and heart attacks.
-
Sedentary Lifestyle: Prolonged periods of inactivity can slow blood flow and increase the risk of clot formation, especially in the legs.
-
Surgery and Trauma: Surgical procedures and traumatic injuries can damage blood vessels and trigger the clotting process.
-
Pregnancy: Pregnancy increases the risk of blood clots due to hormonal changes and increased pressure on the veins in the pelvis.
-
Certain Medications: Some medications, such as birth control pills and hormone replacement therapy, can increase the risk of blood clots.
-
Smoking: Smoking damages blood vessels and increases the risk of clot formation.
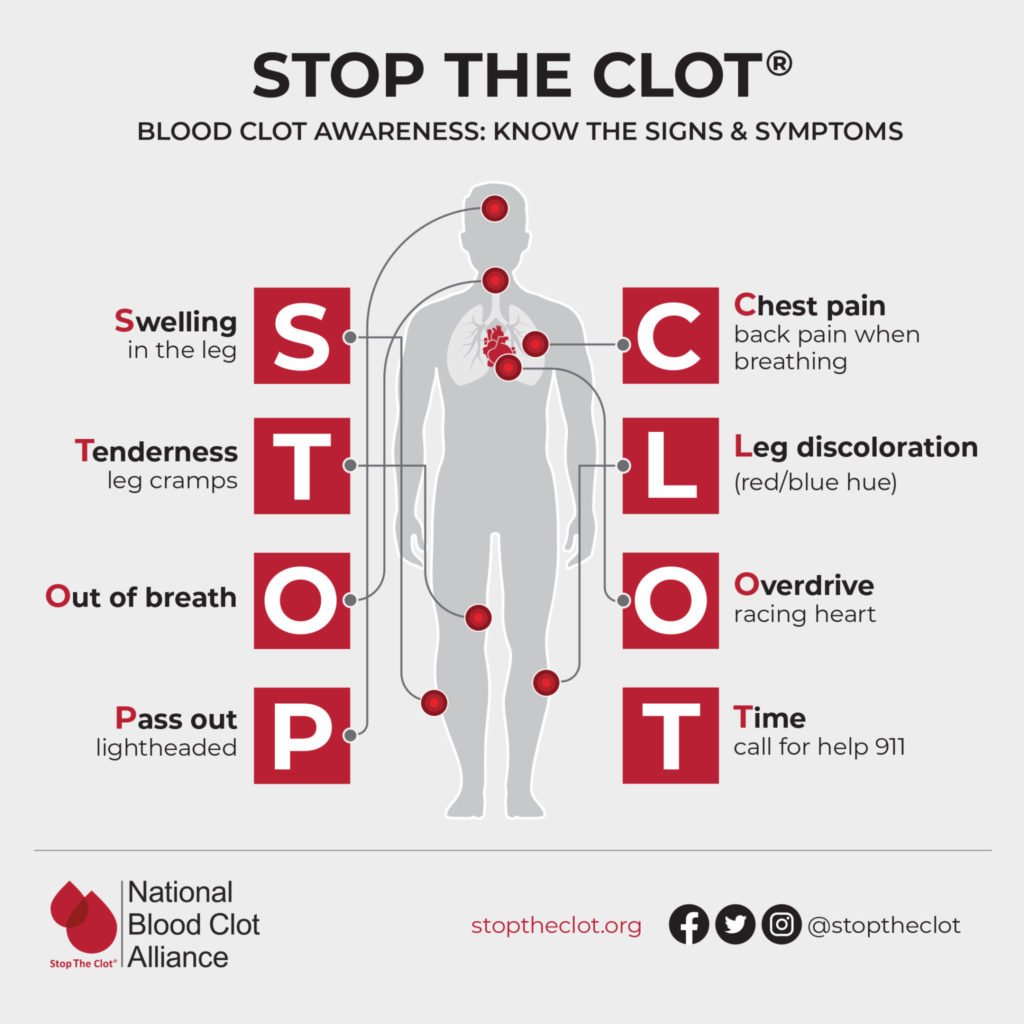
Symptoms of Blood Clots in the Heart
The symptoms of blood clots in the heart can vary depending on the location and size of the clot, as well as the overall health of the individual. Some common symptoms include:
- Chest pain or discomfort
- Shortness of breath
- Sweating
- Nausea or vomiting
- Lightheadedness or dizziness
- Irregular heartbeat
- Pain in the arm, shoulder, or jaw
It is important to seek immediate medical attention if you experience any of these symptoms, as they could indicate a heart attack or other serious cardiovascular event.
Diagnosis of Blood Clots in the Heart
Diagnosing blood clots in the heart typically involves a combination of medical history, physical examination, and diagnostic tests. Some common diagnostic tests include:
-
Electrocardiogram (ECG or EKG): An ECG records the electrical activity of the heart and can help identify abnormalities in heart rhythm or signs of a heart attack.
-
Echocardiogram: An echocardiogram uses sound waves to create images of the heart, allowing doctors to assess the heart’s structure and function.
-
Blood Tests: Blood tests can measure levels of certain enzymes and proteins that are released into the bloodstream when the heart muscle is damaged.
-
Coronary Angiography: Coronary angiography involves injecting a contrast dye into the coronary arteries and taking X-ray images to visualize any blockages or narrowing.
-
CT Scan or MRI: In some cases, a CT scan or MRI may be used to visualize blood clots in the heart or lungs.
Treatment of Blood Clots in the Heart
The treatment of blood clots in the heart depends on the location and size of the clot, as well as the underlying cause. Some common treatment options include:
-
Anticoagulant Medications: Anticoagulants, also known as blood thinners, are medications that help prevent blood clots from forming or growing larger. Common anticoagulants include warfarin, heparin, and direct oral anticoagulants (DOACs).
-
Thrombolytic Therapy: Thrombolytic therapy involves using medications to dissolve blood clots that have already formed. This treatment is often used in emergency situations, such as a heart attack or stroke.
-
Antiplatelet Medications: Antiplatelet medications, such as aspirin and clopidogrel, help prevent platelets from clumping together and forming clots.
-
Angioplasty and Stenting: Angioplasty is a procedure in which a balloon-tipped catheter is used to open a blocked coronary artery. A stent, which is a small mesh tube, may be placed in the artery to help keep it open.
-
Surgery: In some cases, surgery may be necessary to remove a blood clot or repair a damaged heart valve.
Prevention of Blood Clots in the Heart
There are several steps you can take to reduce your risk of developing blood clots in the heart:
-
Manage Risk Factors: Control risk factors such as high blood pressure, high cholesterol, diabetes, and obesity.
-
Maintain a Healthy Lifestyle: Eat a healthy diet, exercise regularly, and maintain a healthy weight.
-
Quit Smoking: Smoking damages blood vessels and increases the risk of clot formation.
-
Stay Hydrated: Dehydration can increase the risk of blood clots.
-
Move Regularly: Avoid prolonged periods of inactivity, especially during long flights or car rides.
-
Follow Doctor’s Recommendations: If you have a condition that increases your risk of blood clots, follow your doctor’s recommendations for medication and lifestyle changes.
Conclusion
Blood clots can pose a significant threat to the heart, leading to heart attacks, strokes, and other serious cardiovascular events. Understanding the relationship between blood clots and the heart, as well as the risk factors and symptoms associated with blood clots, is crucial for preventing and managing these conditions. By adopting a healthy lifestyle, managing risk factors, and seeking prompt medical attention when necessary, you can reduce your risk of developing blood clots in the heart and protect your cardiovascular health.







Leave a Reply