“How Climate Change Affects Cardiovascular Risk
Related Articles How Climate Change Affects Cardiovascular Risk
- The Future Of Heart Transplants
- Pulmonary Hypertension And The Heart
- Disability Rights And Advocacy For Chronic Disease Patients – Part 7
- Innovative Therapies For Acute Lymphoblastic Leukemia (ALL)
- Lifestyle Changes To Manage Chronic Conditions – Part 5: Optimizing Sleep, Managing Pain, And Cultivating Mindfulness
Introduction
We will be happy to explore interesting topics related to How Climate Change Affects Cardiovascular Risk. Come on knit interesting information and provide new insights to readers.
How Climate Change Affects Cardiovascular Risk
Climate change is one of the most pressing global challenges of our time, with far-reaching consequences for human health. While the effects of climate change on respiratory illnesses, infectious diseases, and mental health have garnered significant attention, the impact on cardiovascular health is increasingly recognized as a major concern. Cardiovascular diseases (CVDs), including heart disease, stroke, and heart failure, are already the leading cause of death worldwide, and climate change is poised to exacerbate the risks and burdens associated with these conditions.
The Intertwined Relationship between Climate Change and Cardiovascular Health
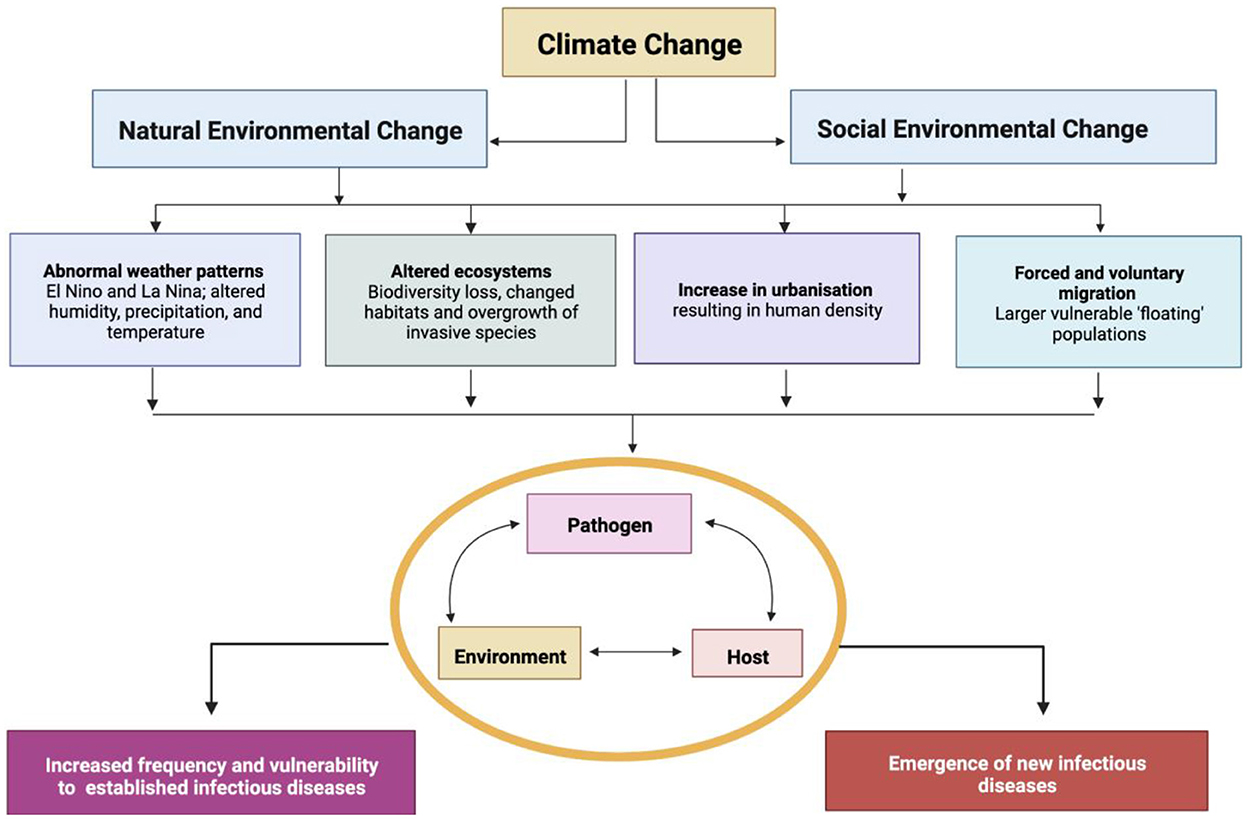
Climate change influences cardiovascular health through a complex web of direct and indirect pathways. Extreme weather events, air pollution, temperature fluctuations, and changes in vector-borne diseases all contribute to increased cardiovascular risk.
1. Extreme Weather Events
Climate change is driving more frequent and intense extreme weather events, such as heatwaves, floods, droughts, wildfires, and hurricanes. These events can have devastating consequences for cardiovascular health.
-
Heatwaves: Heatwaves place significant strain on the cardiovascular system. The body’s natural cooling mechanisms, such as sweating and vasodilation, become less effective in extreme heat. This can lead to dehydration, electrolyte imbalances, and increased heart rate. Individuals with pre-existing cardiovascular conditions are particularly vulnerable, as their hearts may struggle to meet the increased demands. Heatwaves have been linked to increased hospitalizations and mortality from heart attacks, strokes, and heart failure.
-
Floods: Floods can disrupt healthcare services, displace populations, and contaminate water sources. These disruptions can lead to medication shortages, delayed medical care, and increased stress levels, all of which can negatively impact cardiovascular health. Additionally, floodwaters can carry pathogens that increase the risk of infections, which can further strain the cardiovascular system.
-
Wildfires: Wildfires release large amounts of particulate matter into the air, which can travel long distances and affect air quality in areas far from the fires themselves. Exposure to particulate matter can trigger inflammation in the lungs and blood vessels, increasing the risk of heart attacks, strokes, and arrhythmias.
-
Hurricanes: Hurricanes can cause widespread damage to infrastructure, including hospitals and clinics. They can also disrupt transportation systems, making it difficult for people to access medical care. The stress and trauma associated with hurricanes can also increase the risk of cardiovascular events.
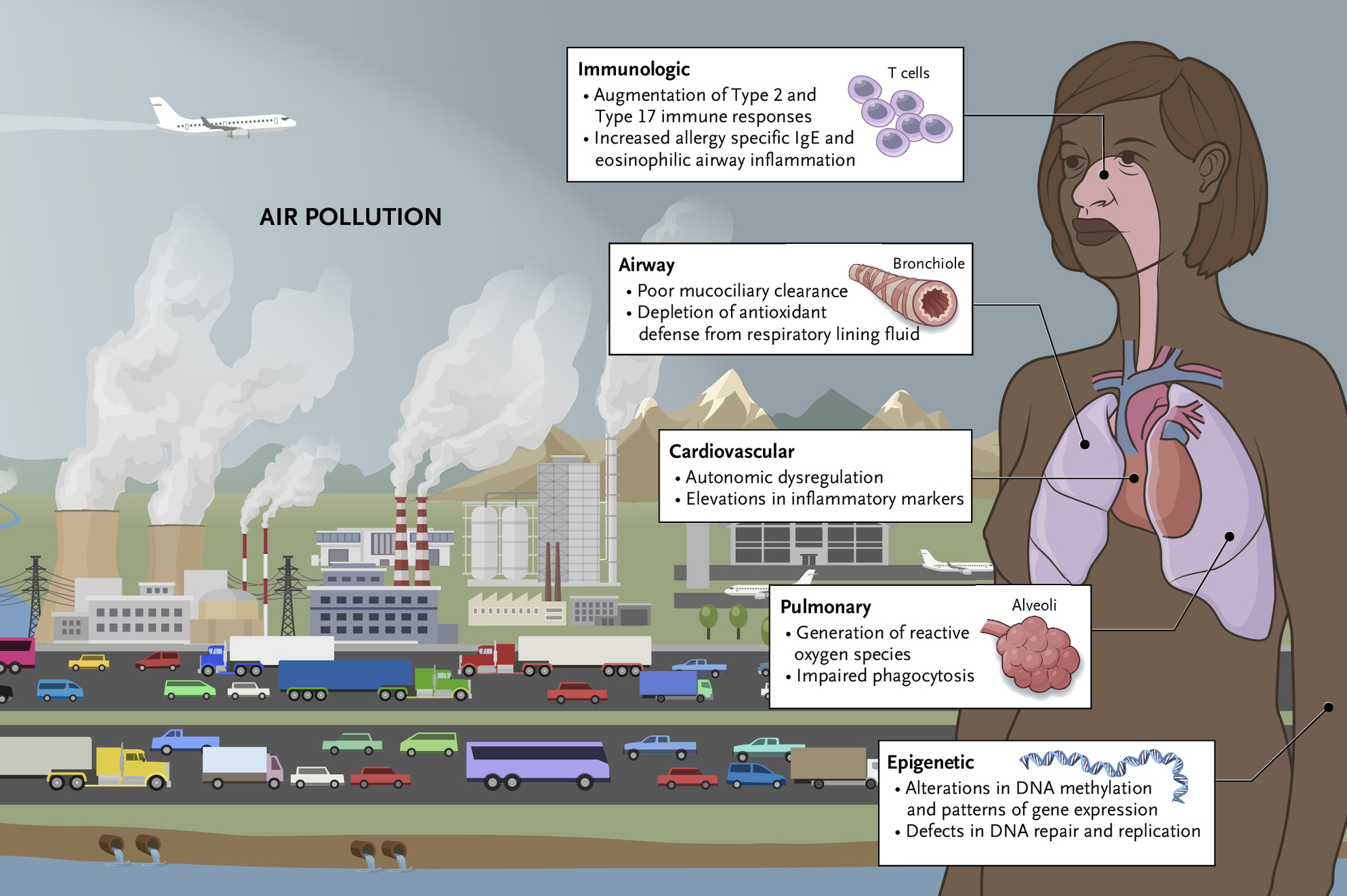
2. Air Pollution
Climate change is contributing to increased levels of air pollution, both directly and indirectly. Rising temperatures can accelerate the formation of ground-level ozone, a major component of smog. Wildfires, which are becoming more frequent and intense due to climate change, release large amounts of particulate matter into the air.
-
Particulate Matter: Particulate matter (PM) is a mixture of tiny particles and liquid droplets that can be inhaled deep into the lungs. Fine particulate matter (PM2.5) is particularly harmful, as it can enter the bloodstream and trigger inflammation throughout the body. Exposure to PM2.5 has been linked to increased risk of heart attacks, strokes, arrhythmias, and heart failure.
-
Ozone: Ozone is a gas that can irritate the lungs and airways. Exposure to ozone can trigger inflammation in the lungs, making it more difficult to breathe. Ozone exposure has been linked to increased risk of respiratory illnesses, such as asthma and bronchitis, which can further strain the cardiovascular system.
3. Temperature Fluctuations
Climate change is causing more extreme temperature fluctuations, with hotter summers and colder winters. These fluctuations can place additional stress on the cardiovascular system.
-
Cold Weather: Cold weather can cause blood vessels to constrict, increasing blood pressure and the risk of blood clots. Cold weather has been linked to increased risk of heart attacks and strokes.
-
Hot Weather: Hot weather can cause blood vessels to dilate, lowering blood pressure. This can lead to dizziness, fainting, and dehydration. Hot weather can also increase the risk of heatstroke, a life-threatening condition that can damage the heart.
4. Changes in Vector-Borne Diseases
Climate change is altering the distribution and prevalence of vector-borne diseases, such as Lyme disease, West Nile virus, and Zika virus. These diseases can cause inflammation and damage to the heart, increasing the risk of cardiovascular complications.
-
Lyme Disease: Lyme disease is caused by bacteria transmitted through the bite of infected ticks. Lyme disease can cause inflammation of the heart, leading to myocarditis (inflammation of the heart muscle) and heart block (a disruption of the electrical signals that control the heartbeat).
-
West Nile Virus: West Nile virus is transmitted through the bite of infected mosquitoes. West Nile virus can cause inflammation of the heart, leading to myocarditis and pericarditis (inflammation of the sac surrounding the heart).
-
Zika Virus: Zika virus is transmitted through the bite of infected mosquitoes. Zika virus infection during pregnancy can cause microcephaly (a birth defect in which the baby’s head is smaller than expected) and other birth defects. Zika virus infection has also been linked to increased risk of Guillain-Barré syndrome, a rare autoimmune disorder that can cause paralysis.
Vulnerable Populations
Certain populations are particularly vulnerable to the cardiovascular effects of climate change. These include:
-
Older Adults: Older adults are more likely to have pre-existing cardiovascular conditions, making them more susceptible to the effects of extreme weather events and air pollution.
-
Children: Children’s cardiovascular systems are still developing, making them more vulnerable to the effects of air pollution and temperature fluctuations.
-
People with Pre-Existing Cardiovascular Conditions: People with pre-existing cardiovascular conditions, such as heart disease, stroke, and heart failure, are at increased risk of experiencing cardiovascular events during extreme weather events and periods of high air pollution.
-
Low-Income Communities: Low-income communities are often located in areas that are more vulnerable to the effects of climate change, such as floodplains and areas with high levels of air pollution. They also may have limited access to healthcare and resources to cope with the health impacts of climate change.
Prevention and Mitigation Strategies
Addressing the cardiovascular risks of climate change requires a multi-pronged approach that includes both prevention and mitigation strategies.
-
Reduce Greenhouse Gas Emissions: The most important step in preventing the cardiovascular effects of climate change is to reduce greenhouse gas emissions. This can be achieved through a variety of measures, such as transitioning to renewable energy sources, improving energy efficiency, and reducing deforestation.
-
Adapt to Climate Change: Even if greenhouse gas emissions are reduced, some degree of climate change is inevitable. It is therefore important to adapt to the changing climate by implementing measures to protect cardiovascular health. These measures include:
- Developing heat action plans to protect vulnerable populations during heatwaves.
- Improving air quality monitoring and warning systems.
- Strengthening healthcare infrastructure to withstand extreme weather events.
- Promoting healthy lifestyles, such as eating a healthy diet and getting regular exercise.
-
Raise Awareness: It is important to raise awareness among the public and healthcare professionals about the cardiovascular risks of climate change. This can be achieved through educational campaigns, public service announcements, and training programs for healthcare professionals.
Conclusion
Climate change is a significant threat to cardiovascular health. Extreme weather events, air pollution, temperature fluctuations, and changes in vector-borne diseases all contribute to increased cardiovascular risk. Certain populations, such as older adults, children, people with pre-existing cardiovascular conditions, and low-income communities, are particularly vulnerable. Addressing the cardiovascular risks of climate change requires a multi-pronged approach that includes both prevention and mitigation strategies. By reducing greenhouse gas emissions, adapting to climate change, and raising awareness, we can protect cardiovascular health and build a more sustainable future.







Leave a Reply