“Supraventricular Tachycardia: What It Means
Related Articles Supraventricular Tachycardia: What It Means
- Workplace Accommodations For Employees With Chronic Diseases
- Preventive Screening Guidelines For Chronic Conditions – Part 6
- Workplace Accommodations For Employees With Chronic Diseases – Part 3
- Psychological Resilience In Leukemia Patients: Navigating Challenges And Fostering Well-being
- Integrative Medicine In Leukemia Care: A Comprehensive Approach To Healing
Introduction
We will be happy to explore interesting topics related to Supraventricular Tachycardia: What It Means. Come on knit interesting information and provide new insights to readers.
Supraventricular Tachycardia: What It Means
Supraventricular tachycardia (SVT) is a type of abnormal heart rhythm, or arrhythmia, that originates in the upper chambers of the heart, above the ventricles. This condition can cause the heart to beat much faster than normal, sometimes up to 150-250 beats per minute or even higher. While SVT is often not life-threatening, it can be quite distressing and can significantly impact a person’s quality of life. Understanding what SVT is, its causes, symptoms, diagnosis, and treatment options is crucial for managing this condition effectively.
Understanding the Heart’s Electrical System
To fully grasp SVT, it’s essential to understand the heart’s electrical system. The heart’s natural pacemaker, the sinoatrial (SA) node, located in the right atrium, initiates the electrical impulses that control the heartbeat. These impulses travel through the atria, causing them to contract and pump blood into the ventricles. The impulses then reach the atrioventricular (AV) node, which acts as a gatekeeper, briefly delaying the signal before sending it down the His-Purkinje system to the ventricles. This coordinated electrical activity ensures that the heart beats in a regular and efficient manner.
In SVT, this normal electrical pathway is disrupted. Instead of following the regular route, the electrical signal gets caught in a loop, creating a rapid and repetitive firing that causes the heart to beat very quickly. This loop can occur due to several reasons, which we’ll explore in the causes section.
Causes of Supraventricular Tachycardia
SVT can arise from several underlying mechanisms, often involving abnormal electrical pathways or circuits within the heart. Here are some of the common causes:
-
AV Nodal Reentrant Tachycardia (AVNRT): This is the most common type of SVT. It occurs when there are two pathways within or near the AV node. One pathway conducts electrical impulses slowly, and the other conducts them quickly. When an impulse travels down the slow pathway and then back up the fast pathway, it creates a reentrant circuit, leading to rapid heartbeats.
-
AV Reciprocating Tachycardia (AVRT): This type involves an accessory pathway, an extra electrical connection between the atria and ventricles that is present at birth. The electrical impulse travels down the AV node to the ventricles and then back up to the atria through the accessory pathway, creating a reentrant circuit. Wolff-Parkinson-White (WPW) syndrome is a specific type of AVRT where the accessory pathway is particularly prominent and can be identified on an electrocardiogram (ECG).
-
Atrial Tachycardia: This type originates from a single location (focus) within the atria that fires electrical impulses rapidly and independently of the SA node. This rapid firing overrides the normal rhythm, causing the heart to beat quickly.
-
Less Common Causes: Less frequently, SVT can be triggered by other conditions such as:
- Certain medications: Some medications, such as decongestants or asthma inhalers, can increase heart rate and potentially trigger SVT in susceptible individuals.
- Excessive caffeine or alcohol consumption: These substances can stimulate the heart and increase the risk of arrhythmias.
- Hyperthyroidism: An overactive thyroid gland can lead to an elevated heart rate and increase the likelihood of SVT.
- Underlying heart conditions: Conditions like coronary artery disease, heart valve problems, or heart failure can sometimes contribute to the development of SVT.
- Electrolyte imbalances: Abnormal levels of electrolytes, such as potassium or magnesium, can disrupt the heart’s electrical activity.
In some cases, the exact cause of SVT may not be identifiable.
Symptoms of Supraventricular Tachycardia
The symptoms of SVT can vary from person to person and can depend on the frequency and duration of the rapid heartbeats. Some individuals may experience only mild symptoms, while others may have more severe symptoms that require immediate medical attention. Common symptoms include:
- Palpitations: A racing, pounding, or fluttering sensation in the chest. This is the most common symptom of SVT.
- Rapid Heartbeat: A noticeably fast heart rate, often exceeding 150 beats per minute. You may be able to feel your pulse racing in your neck or wrist.
- Dizziness or Lightheadedness: The rapid heartbeat can reduce blood flow to the brain, leading to dizziness or lightheadedness.
- Shortness of Breath: The heart’s increased workload can make it difficult to breathe comfortably.
- Chest Pain or Discomfort: Some individuals may experience chest pain, pressure, or tightness during an SVT episode.
- Anxiety or Nervousness: The sudden onset of a rapid heartbeat can trigger feelings of anxiety or nervousness.
- Sweating: Excessive sweating may occur as the body tries to cope with the increased heart rate.
- Fainting or Near-Fainting (Syncope): In severe cases, the reduced blood flow to the brain can cause fainting or near-fainting.
It’s important to note that some individuals may experience SVT without any noticeable symptoms. These episodes may only be detected during a routine medical examination or through heart monitoring.
Diagnosing Supraventricular Tachycardia
Diagnosing SVT typically involves a combination of physical examination, medical history, and diagnostic tests. The most important diagnostic tool is the electrocardiogram (ECG), which records the heart’s electrical activity.
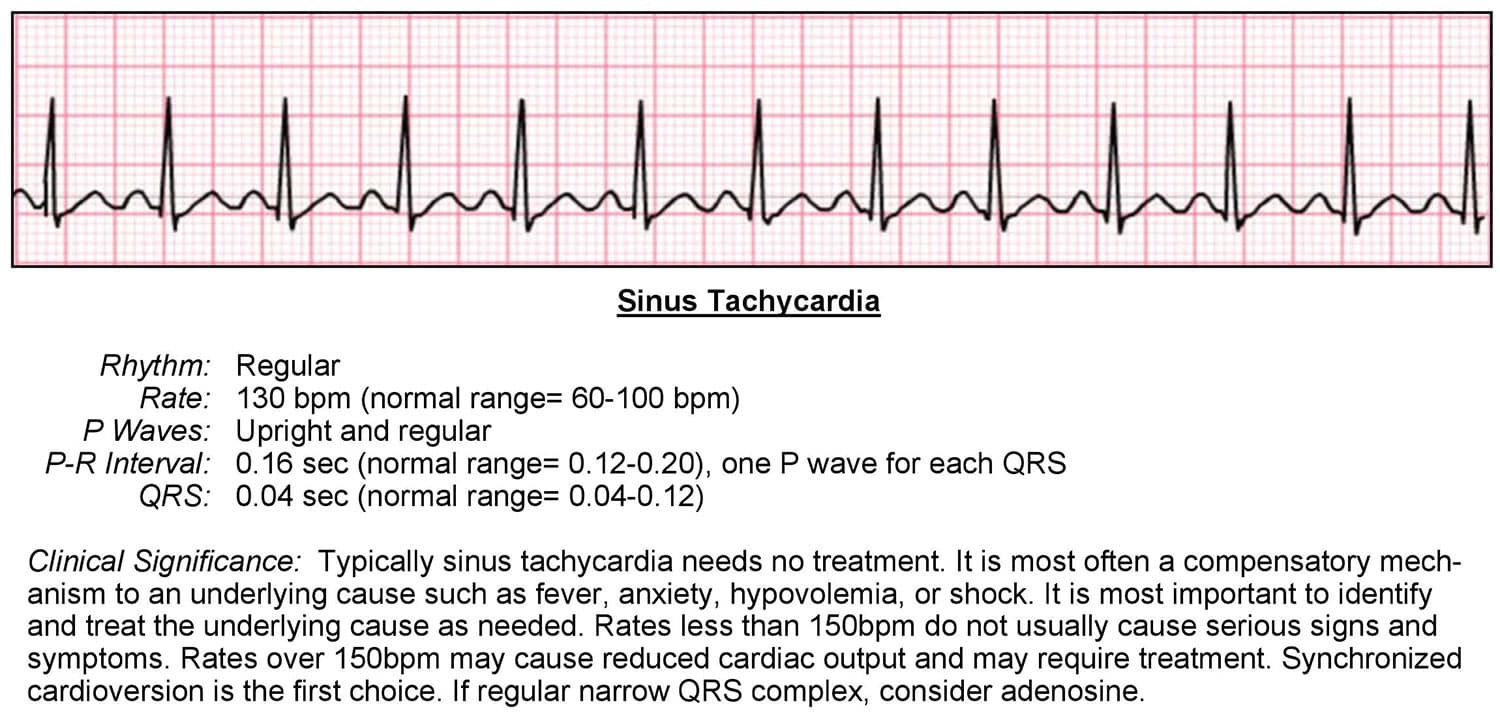
- Electrocardiogram (ECG): An ECG can reveal the characteristic features of SVT, such as the rapid heart rate and the abnormal electrical patterns. A standard ECG records the heart’s electrical activity over a short period (usually a few seconds).
- Holter Monitor: If SVT episodes are infrequent or unpredictable, a Holter monitor may be used. This is a portable ECG device that continuously records the heart’s electrical activity over a period of 24-48 hours or even longer.
- Event Recorder: An event recorder is another type of portable ECG device that records the heart’s electrical activity only when the patient experiences symptoms. The patient activates the device when they feel a rapid heartbeat or other symptoms.
- Electrophysiology (EP) Study: An EP study is an invasive procedure that involves inserting catheters into blood vessels and threading them to the heart. The catheters are used to record the heart’s electrical activity from within and to stimulate the heart to induce arrhythmias. An EP study can help identify the specific location and mechanism of the SVT, which is crucial for guiding treatment decisions.
- Echocardiogram: An echocardiogram is an ultrasound of the heart that can assess the heart’s structure and function. It can help rule out underlying heart conditions that may be contributing to the SVT.
- Blood Tests: Blood tests may be performed to check for electrolyte imbalances, thyroid problems, or other conditions that could be contributing to the SVT.
Treatment Options for Supraventricular Tachycardia
The treatment for SVT depends on the frequency and severity of the episodes, the underlying cause, and the patient’s overall health. Treatment options range from simple vagal maneuvers to medications and invasive procedures.
-
Vagal Maneuvers: These are simple techniques that can sometimes stop an SVT episode by stimulating the vagus nerve, which helps slow down the heart rate. Common vagal maneuvers include:
- Valsalva Maneuver: Trying to exhale forcefully while holding your nose and keeping your mouth closed.
- Carotid Sinus Massage: Applying gentle pressure to the carotid artery in the neck (this should only be performed by a healthcare professional).
- Coughing: Coughing forcefully several times in a row.
- Applying a cold compress to the face: Submerging your face in ice water for a short period.
-
Medications: Several medications can be used to control SVT, either to stop an ongoing episode or to prevent future episodes.
- Adenosine: This medication is often used to stop an acute SVT episode. It is administered intravenously and works by temporarily blocking the AV node, interrupting the reentrant circuit.
- Calcium Channel Blockers: These medications, such as verapamil and diltiazem, slow down the heart rate by blocking the flow of calcium into the heart cells.
- Beta-Blockers: These medications, such as metoprolol and propranolol, block the effects of adrenaline on the heart, slowing down the heart rate and reducing the force of heart contractions.
- Antiarrhythmic Medications: These medications, such as flecainide, propafenone, and amiodarone, help prevent arrhythmias by altering the heart’s electrical activity.
-
Catheter Ablation: This is a minimally invasive procedure that is often used to permanently cure SVT. During catheter ablation, a catheter is inserted into a blood vessel and threaded to the heart. Radiofrequency energy is then used to destroy (ablate) the abnormal electrical pathway or focus that is causing the SVT. Catheter ablation is highly effective for treating AVNRT, AVRT, and atrial tachycardia.
-
Cardioversion: This procedure involves delivering an electrical shock to the heart to restore a normal rhythm. Cardioversion is typically used in emergency situations when medications are not effective or when the patient is unstable.
Lifestyle Modifications
In addition to medical treatments, certain lifestyle modifications can help manage SVT:
- Avoid Triggers: Identify and avoid potential triggers of SVT, such as excessive caffeine or alcohol consumption, smoking, and certain medications.
- Manage Stress: Stress can trigger SVT episodes in some individuals. Practice stress-reducing techniques such as yoga, meditation, or deep breathing exercises.
- Maintain a Healthy Weight: Obesity can increase the risk of heart problems, including arrhythmias. Maintaining a healthy weight through diet and exercise can help reduce the risk of SVT.
- Regular Exercise: Regular exercise can improve cardiovascular health and reduce the risk of arrhythmias. However, it’s important to talk to your doctor before starting a new exercise program, especially if you have SVT.
- Stay Hydrated: Dehydration can sometimes trigger arrhythmias. Drink plenty of fluids throughout the day.
Living with Supraventricular Tachycardia
Living with SVT can be challenging, but with proper diagnosis, treatment, and lifestyle modifications, most individuals can manage their condition effectively and live a normal, active life. It’s important to work closely with your doctor to develop a personalized treatment plan and to monitor your condition regularly. Be sure to report any changes in your symptoms or any new concerns to your doctor promptly. With the right approach, you can minimize the impact of SVT on your life and maintain a good quality of life.








Leave a Reply