“The Impact of Obesity on Cardiovascular Disease
Related Articles The Impact of Obesity on Cardiovascular Disease
- Public Health Strategies For Leukemia Prevention
- Genetic Testing And Personalized Medicine In Chronic Diseases – Part 2
- Emerging Therapies For Managing Chronic Conditions – Part 6
- Workplace Accommodations For Employees With Chronic Diseases – Part 7
- Economic Burden Of Chronic Illnesses: A Global Perspective
Introduction
On this special occasion, we are happy to review interesting topics related to The Impact of Obesity on Cardiovascular Disease. Come on knit interesting information and provide new insights to readers.
Table of Content
The Impact of Obesity on Cardiovascular Disease
Introduction
Obesity has become a global health crisis, with alarming rates of prevalence in both developed and developing countries. While the visible effects of obesity are well-known, its profound impact on cardiovascular health is often underestimated. Cardiovascular disease (CVD) encompasses a range of conditions affecting the heart and blood vessels, including coronary artery disease, heart failure, stroke, and hypertension. Obesity is a major modifiable risk factor for CVD, contributing to its development, progression, and severity. This article explores the intricate relationship between obesity and CVD, delving into the underlying mechanisms, associated risk factors, clinical manifestations, and strategies for prevention and management.
Understanding Obesity
Obesity is a complex metabolic disorder characterized by excessive accumulation of body fat. It is typically defined by a body mass index (BMI) of 30 kg/m² or higher. BMI is a simple measure of weight relative to height, but it does not account for body composition or fat distribution. Other measures of obesity include waist circumference, waist-to-hip ratio, and body fat percentage.
Obesity results from an imbalance between energy intake and energy expenditure. When energy intake exceeds energy expenditure, the excess energy is stored as fat. Several factors contribute to this imbalance, including:
- Dietary factors: Consumption of calorie-dense foods high in fat, sugar, and processed ingredients.
- Physical inactivity: Sedentary lifestyles and lack of regular exercise.
- Genetic predisposition: Inherited genes that influence metabolism, appetite, and fat storage.
- Environmental factors: Availability of unhealthy foods, marketing of processed foods, and lack of safe places for physical activity.
- Hormonal factors: Hormones such as leptin and ghrelin play a role in appetite regulation.
- Medical conditions: Certain medical conditions, such as hypothyroidism and polycystic ovary syndrome (PCOS), can contribute to weight gain.
Obesity and Cardiovascular Risk Factors
Obesity is closely linked to several established risk factors for CVD, including:
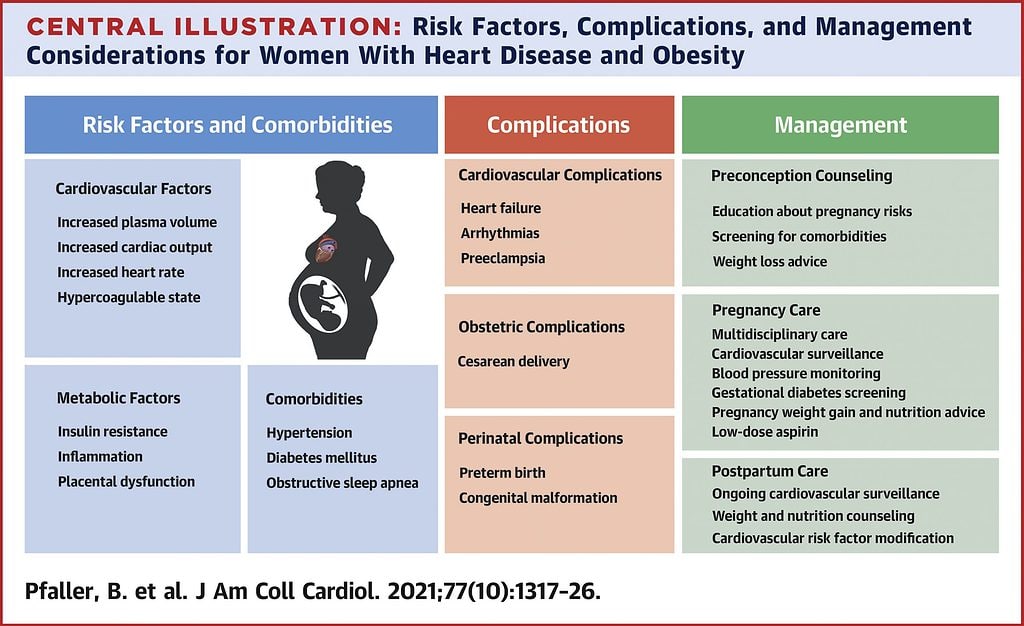
- Hypertension: Obesity increases blood volume and cardiac output, leading to elevated blood pressure. It also impairs the function of the kidneys, which play a crucial role in blood pressure regulation.
- Dyslipidemia: Obesity is associated with abnormal lipid profiles, including elevated triglycerides, low high-density lipoprotein (HDL) cholesterol, and increased low-density lipoprotein (LDL) cholesterol. These lipid abnormalities promote the formation of atherosclerotic plaques in the arteries.
- Insulin Resistance and Type 2 Diabetes: Obesity is a major driver of insulin resistance, a condition in which the body’s cells become less responsive to insulin. Insulin resistance leads to elevated blood sugar levels and eventually type 2 diabetes. Diabetes is a potent risk factor for CVD, increasing the risk of heart attack, stroke, and peripheral artery disease.
- Inflammation: Obesity is characterized by chronic low-grade inflammation, with increased levels of inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6). Inflammation contributes to the development and progression of atherosclerosis.
- Sleep Apnea: Obesity is a strong risk factor for obstructive sleep apnea (OSA), a condition in which breathing repeatedly stops and starts during sleep. OSA can lead to hypertension, arrhythmias, and heart failure.
Mechanisms Linking Obesity to CVD
The relationship between obesity and CVD is complex and multifaceted. Several mechanisms contribute to the adverse effects of obesity on cardiovascular health:
- Endothelial Dysfunction: Obesity impairs the function of the endothelium, the inner lining of blood vessels. Endothelial dysfunction leads to reduced production of nitric oxide, a vasodilator that helps keep blood vessels open. It also promotes inflammation and the formation of blood clots.
- Atherosclerosis: Obesity accelerates the development of atherosclerosis, the buildup of plaque in the arteries. Atherosclerotic plaques can narrow the arteries, reducing blood flow to the heart and other organs. They can also rupture, leading to blood clot formation and acute events such as heart attack and stroke.
- Left Ventricular Hypertrophy: Obesity increases the workload on the heart, leading to left ventricular hypertrophy (LVH), an enlargement of the heart’s main pumping chamber. LVH can impair heart function and increase the risk of heart failure, arrhythmias, and sudden cardiac death.
- Heart Failure: Obesity is a major risk factor for heart failure, a condition in which the heart is unable to pump enough blood to meet the body’s needs. Obesity can lead to both systolic heart failure (reduced pumping ability) and diastolic heart failure (impaired filling of the heart).
- Arrhythmias: Obesity increases the risk of various arrhythmias, including atrial fibrillation, a common heart rhythm disorder that can lead to stroke and heart failure.
Clinical Manifestations of CVD in Obese Individuals
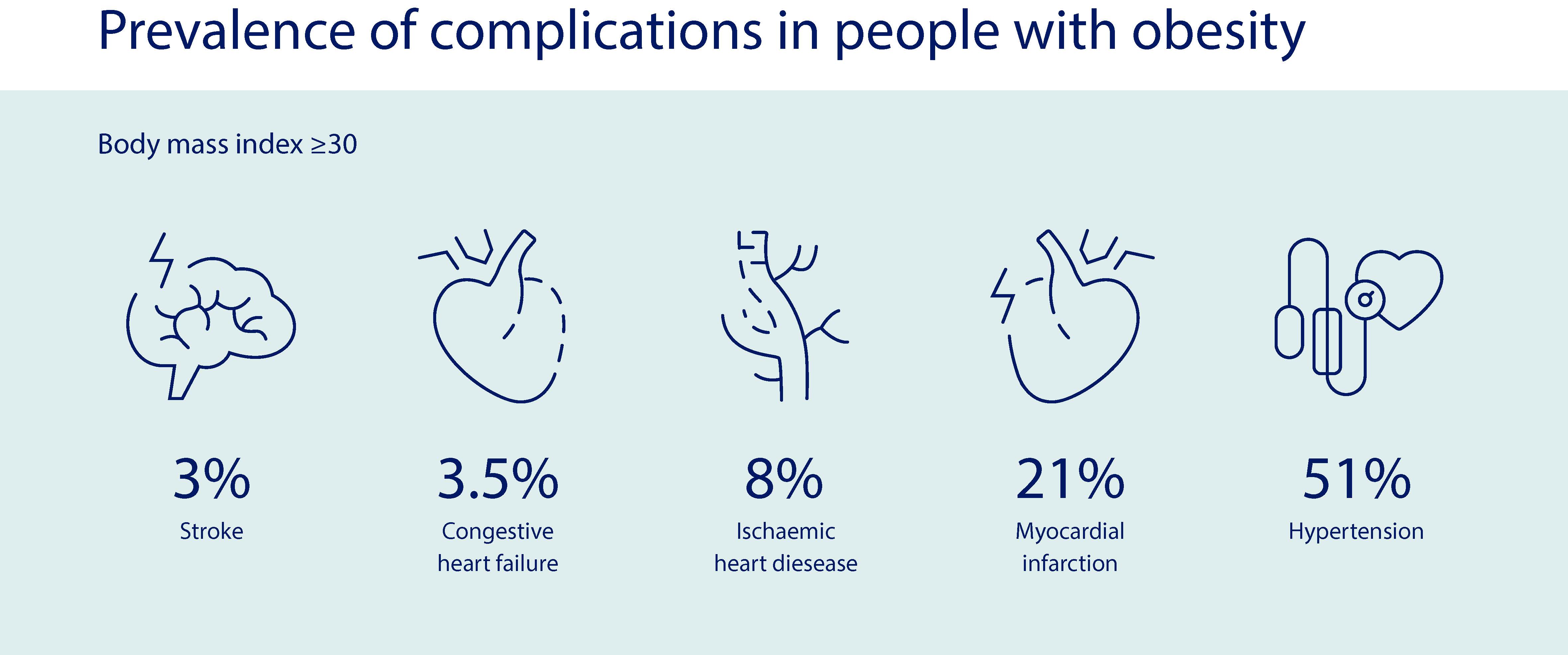
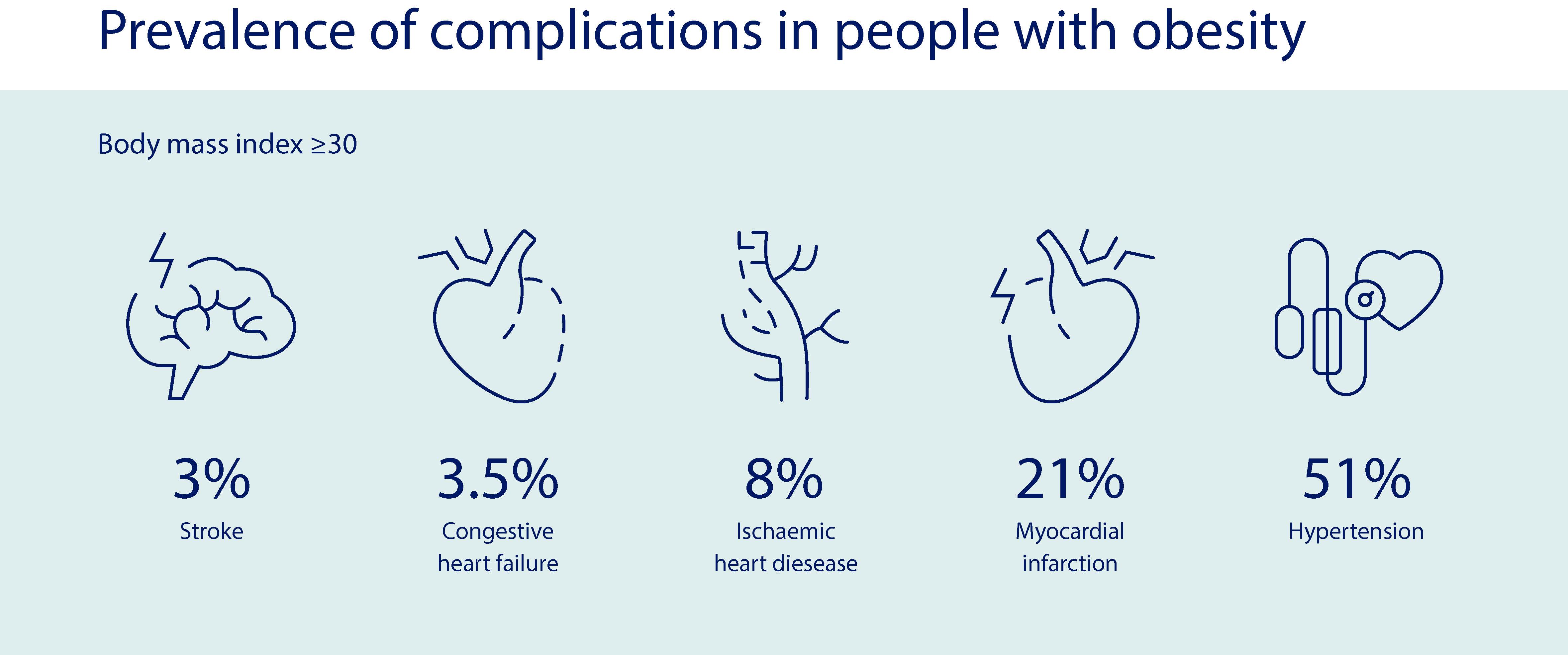
Obese individuals are at increased risk of developing a wide range of CVD conditions, including:
- Coronary Artery Disease (CAD): CAD is the most common type of heart disease and is caused by the buildup of plaque in the coronary arteries, which supply blood to the heart muscle. Obese individuals are more likely to develop CAD and experience heart attacks and angina (chest pain).
- Heart Failure: Obesity is a major risk factor for heart failure, a condition in which the heart is unable to pump enough blood to meet the body’s needs. Obese individuals are more likely to develop both systolic and diastolic heart failure.
- Stroke: Obesity increases the risk of stroke, which occurs when blood flow to the brain is interrupted. Obese individuals are more likely to experience ischemic stroke (caused by a blood clot) and hemorrhagic stroke (caused by bleeding in the brain).
- Hypertension: Obesity is a major cause of hypertension, or high blood pressure. Hypertension increases the risk of heart attack, stroke, kidney disease, and other health problems.
- Peripheral Artery Disease (PAD): PAD is a condition in which the arteries that supply blood to the legs and feet become narrowed or blocked. Obese individuals are more likely to develop PAD and experience leg pain, numbness, and ulcers.
- Venous Thromboembolism (VTE): VTE is a condition in which blood clots form in the veins, usually in the legs or lungs. Obese individuals are at increased risk of VTE.
Prevention and Management
Preventing and managing obesity is crucial for reducing the risk of CVD. Lifestyle modifications are the cornerstone of obesity management and include:
- Dietary Changes: Adopting a healthy eating pattern that is low in calories, saturated fat, trans fat, cholesterol, and added sugars. Emphasize fruits, vegetables, whole grains, and lean protein sources.
- Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week. Incorporate strength training exercises to build muscle mass and boost metabolism.
- Behavioral Therapy: Addressing underlying behavioral factors that contribute to overeating and physical inactivity. Techniques such as cognitive-behavioral therapy (CBT) and motivational interviewing can help individuals make sustainable lifestyle changes.
In some cases, medications or surgery may be necessary to achieve significant weight loss and improve cardiovascular health.
- Medications: Several medications are approved for the treatment of obesity, including orlistat, lorcaserin, phentermine-topiramate, and naltrexone-bupropion. These medications work by suppressing appetite, increasing satiety, or blocking the absorption of fat.
- Bariatric Surgery: Bariatric surgery, also known as weight loss surgery, is a surgical procedure that alters the digestive system to reduce food intake and absorption. Bariatric surgery is an effective treatment for severe obesity and can lead to significant improvements in cardiovascular risk factors.
Conclusion
Obesity is a major modifiable risk factor for cardiovascular disease. It contributes to the development, progression, and severity of CVD through a variety of mechanisms, including hypertension, dyslipidemia, insulin resistance, inflammation, and endothelial dysfunction. Obese individuals are at increased risk of developing coronary artery disease, heart failure, stroke, hypertension, peripheral artery disease, and venous thromboembolism. Preventing and managing obesity through lifestyle modifications, medications, and surgery is crucial for reducing the risk of CVD and improving cardiovascular health. Public health initiatives aimed at promoting healthy eating, physical activity, and weight management are essential for addressing the global obesity epidemic and its devastating impact on cardiovascular health.






Leave a Reply