“Precision Medicine in Cardiology: Individualized Approaches
Related Articles Precision Medicine in Cardiology: Individualized Approaches
- Integrative Care Models For Complex Chronic Diseases
- Cultural Perspectives On Chronic Disease Management – Part 10
- Emerging Therapies For Managing Chronic Conditions: A New Dawn Of Hope
- Ethical Considerations In Chronic Disease Research
- The Impact Of Air Pollution On Heart Health
Introduction
With great enthusiasm, let’s explore interesting topics related to Precision Medicine in Cardiology: Individualized Approaches. Let’s knit interesting information and provide new insights to readers.
Table of Content
Precision Medicine in Cardiology: Individualized Approaches
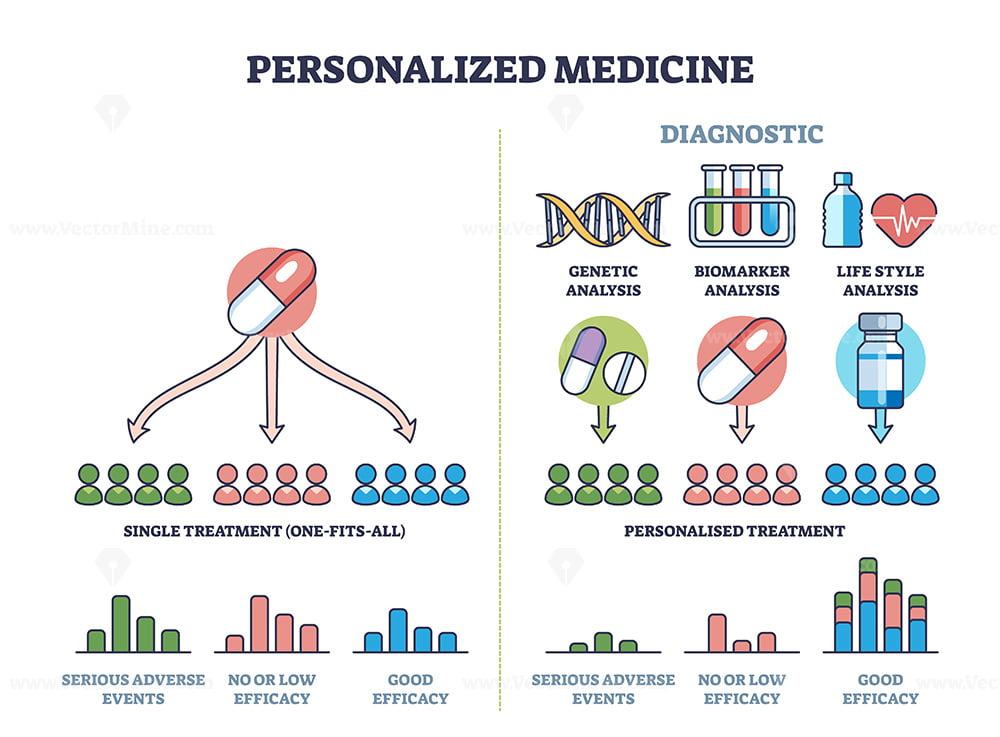
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality worldwide, posing a significant global health challenge. While conventional approaches to cardiology have made substantial progress in managing and treating CVD, they often follow a one-size-fits-all model, which may not be optimal for all patients. Precision medicine, an emerging field that aims to tailor medical treatment to the individual characteristics of each patient, holds great promise for revolutionizing cardiology. By integrating genomic, proteomic, metabolomic, and clinical data, precision medicine can enable more accurate risk stratification, earlier diagnosis, personalized treatment strategies, and improved outcomes for patients with CVD.
The Limitations of Conventional Cardiology
Traditional cardiology relies heavily on population-based guidelines and clinical trials that often do not account for the vast heterogeneity among patients. This approach can lead to several limitations:
-
Suboptimal Risk Stratification: Current risk assessment tools may not accurately identify individuals at high risk of developing CVD, leading to delayed or inadequate preventive measures.
-
Ineffective Treatment Strategies: Standard treatment protocols may not be effective for all patients due to variations in their genetic makeup, lifestyle, and environmental factors.
-
Adverse Drug Reactions: Patients may experience adverse drug reactions due to variations in their drug metabolism and response, which are not always predictable using conventional methods.
-
Delayed Diagnosis: Some cardiovascular conditions may remain undiagnosed until they reach an advanced stage, limiting the effectiveness of treatment interventions.
The Promise of Precision Medicine in Cardiology
Precision medicine offers a paradigm shift in cardiology by moving away from a one-size-fits-all approach to a more individualized and targeted approach. By integrating various data sources, precision medicine can:
-
Improve Risk Stratification: Identify individuals at high risk of developing CVD with greater accuracy, enabling earlier preventive interventions.
-
Tailor Treatment Strategies: Develop personalized treatment plans based on a patient’s unique characteristics, maximizing treatment efficacy and minimizing adverse effects.
-
Predict Drug Response: Identify patients who are likely to respond favorably to specific medications and those who may experience adverse reactions, optimizing drug selection and dosage.
-
Enable Earlier Diagnosis: Detect cardiovascular conditions at an earlier stage, allowing for timely interventions and improved outcomes.
Key Components of Precision Medicine in Cardiology
Precision medicine in cardiology relies on several key components:
-
Genomics: Analyzing an individual’s genome to identify genetic variations that may predispose them to CVD or influence their response to treatment.
-
Proteomics: Studying the proteins present in an individual’s blood or tissue samples to identify biomarkers that can indicate the presence or severity of CVD.
-
Metabolomics: Analyzing the metabolites present in an individual’s blood or urine to identify metabolic signatures that can predict the risk of CVD or response to treatment.
-
Imaging: Utilizing advanced imaging techniques, such as cardiac MRI and PET scans, to visualize the structure and function of the heart and blood vessels, providing insights into disease progression and treatment response.
-
Electronic Health Records (EHRs): Integrating clinical data from EHRs, including patient demographics, medical history, medications, and laboratory results, to provide a comprehensive view of the patient’s health status.
Applications of Precision Medicine in Cardiology
Precision medicine has the potential to transform various aspects of cardiology, including:
-
Coronary Artery Disease (CAD):
- Risk Prediction: Genetic risk scores can identify individuals at high risk of developing CAD, even before the onset of symptoms.
- Personalized Treatment: Genotype-guided antiplatelet therapy can reduce the risk of stent thrombosis in patients undergoing percutaneous coronary intervention (PCI).
- Drug Response Prediction: Genetic testing can predict a patient’s response to statins, allowing for personalized lipid-lowering strategies.
-
Heart Failure:
- Diagnosis and Prognosis: Biomarkers, such as natriuretic peptides and cardiac troponins, can aid in the diagnosis and risk stratification of heart failure patients.
- Personalized Treatment: Genetic testing can identify patients who are likely to benefit from specific heart failure medications, such as beta-blockers and ACE inhibitors.
- Cardiac Resynchronization Therapy (CRT) Optimization: Genetic and imaging data can be used to optimize CRT device programming, improving patient outcomes.
-
Arrhythmias:
- Risk Prediction: Genetic testing can identify individuals at risk of sudden cardiac death due to inherited arrhythmia syndromes, such as long QT syndrome and Brugada syndrome.
- Personalized Treatment: Genotype-guided antiarrhythmic drug therapy can reduce the risk of drug-induced arrhythmias and improve treatment efficacy.
- Catheter Ablation Guidance: Imaging techniques, such as cardiac MRI, can guide catheter ablation procedures for atrial fibrillation and ventricular tachycardia, improving success rates and reducing complications.
-
Cardiomyopathies:
- Diagnosis and Genetic Counseling: Genetic testing can confirm the diagnosis of inherited cardiomyopathies, such as hypertrophic cardiomyopathy and dilated cardiomyopathy, and provide valuable information for genetic counseling.
- Risk Stratification: Genetic and imaging data can be used to identify patients at high risk of sudden cardiac death, guiding decisions about implantable cardioverter-defibrillator (ICD) placement.
- Personalized Treatment: Specific genetic mutations may predict response to certain medications, such as beta-blockers and ACE inhibitors, allowing for personalized treatment strategies.
-
Valvular Heart Disease:
- Risk Prediction: Biomarkers and imaging data can identify patients with asymptomatic valvular heart disease who are at high risk of developing complications, such as heart failure and stroke.
- Timing of Intervention: Precision medicine approaches can help determine the optimal timing for valve replacement or repair, based on individual patient characteristics and disease progression.
- Personalized Valve Selection: Genetic and clinical data can be used to guide the selection of the most appropriate type of prosthetic valve for each patient.
Challenges and Future Directions
Despite the immense potential of precision medicine in cardiology, several challenges remain:
-
Data Integration and Analysis: Integrating and analyzing the vast amounts of data generated by genomics, proteomics, metabolomics, imaging, and EHRs requires sophisticated computational tools and expertise.
-
Clinical Validation: Many precision medicine approaches are still in the early stages of development and require rigorous clinical validation to demonstrate their effectiveness and cost-effectiveness.
-
Ethical Considerations: The use of genetic and other sensitive data raises ethical concerns about privacy, discrimination, and informed consent.
-
Cost and Accessibility: Precision medicine technologies can be expensive, which may limit their accessibility to all patients.
To overcome these challenges and realize the full potential of precision medicine in cardiology, the following steps are necessary:
-
Develop Robust Data Infrastructure: Invest in the development of robust data infrastructure and analytical tools to facilitate the integration and analysis of large-scale datasets.
-
Conduct Large-Scale Clinical Trials: Conduct large-scale clinical trials to validate the effectiveness and cost-effectiveness of precision medicine approaches in diverse patient populations.
-
Address Ethical Concerns: Develop clear ethical guidelines and regulations to ensure the responsible use of genetic and other sensitive data.
-
Promote Education and Training: Promote education and training for healthcare professionals to ensure they have the knowledge and skills necessary to implement precision medicine approaches in clinical practice.
-
Reduce Costs and Improve Accessibility: Explore strategies to reduce the costs of precision medicine technologies and improve their accessibility to all patients, regardless of their socioeconomic status.
Conclusion
Precision medicine holds great promise for revolutionizing cardiology by enabling more accurate risk stratification, earlier diagnosis, personalized treatment strategies, and improved outcomes for patients with CVD. By integrating genomic, proteomic, metabolomic, imaging, and clinical data, precision medicine can tailor medical treatment to the individual characteristics of each patient, maximizing treatment efficacy and minimizing adverse effects. While challenges remain, ongoing research and technological advancements are paving the way for the widespread adoption of precision medicine in cardiology, ultimately leading to better cardiovascular health for all.







Leave a Reply