“Pediatric Heart Disease: Diagnosis and Treatment
Related Articles Pediatric Heart Disease: Diagnosis and Treatment
- Telemedicine And Remote Monitoring For Chronic Illness Care – Part 10: The Future Of Remote Patient Monitoring: Trends, Challenges, And Opportunities
- Leukemia And Neurocognitive Function: Insights From Research
- Educational Interventions For Chronic Disease Prevention – Part 9: Harnessing Technology And Digital Platforms For Scalable Impact
- Gender Disparities In Chronic Disease Diagnosis And Treatment – Part 6
- Telemedicine And Remote Monitoring For Chronic Illness Care – Part 9: Ethical Considerations, Data Security, And Future Directions
Introduction
On this special occasion, we are happy to review interesting topics related to Pediatric Heart Disease: Diagnosis and Treatment. Come on knit interesting information and provide new insights to readers.
Table of Content
Pediatric Heart Disease: Diagnosis and Treatment
Pediatric heart disease encompasses a wide range of congenital and acquired heart conditions that affect infants, children, and adolescents. These conditions can range from mild to life-threatening, and early diagnosis and appropriate treatment are crucial for improving outcomes and quality of life. This article provides an overview of the diagnosis and treatment of pediatric heart disease, covering common types, diagnostic approaches, and various management strategies.
I. Types of Pediatric Heart Disease
Pediatric heart disease can be broadly classified into congenital and acquired heart diseases.
A. Congenital Heart Diseases (CHDs)
Congenital heart diseases are structural abnormalities present at birth. They are the most common type of heart disease in children, affecting approximately 1% of live births. CHDs can involve the heart’s walls, valves, arteries, and veins. Some common types of CHDs include:
- Ventricular Septal Defect (VSD): A hole in the wall separating the two ventricles.
- Atrial Septal Defect (ASD): A hole in the wall separating the two atria.
- Patent Ductus Arteriosus (PDA): Failure of the ductus arteriosus to close after birth.
- Tetralogy of Fallot (TOF): A combination of four defects: VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy.
- Transposition of the Great Arteries (TGA): The aorta and pulmonary artery are switched.
- Coarctation of the Aorta (CoA): Narrowing of the aorta.
- Atrioventricular Canal Defect (AV Canal): A large hole in the center of the heart, involving both atria and ventricles.
- Pulmonary Stenosis: Narrowing of the pulmonary valve.
- Aortic Stenosis: Narrowing of the aortic valve.
- Hypoplastic Left Heart Syndrome (HLHS): Underdevelopment of the left side of the heart.
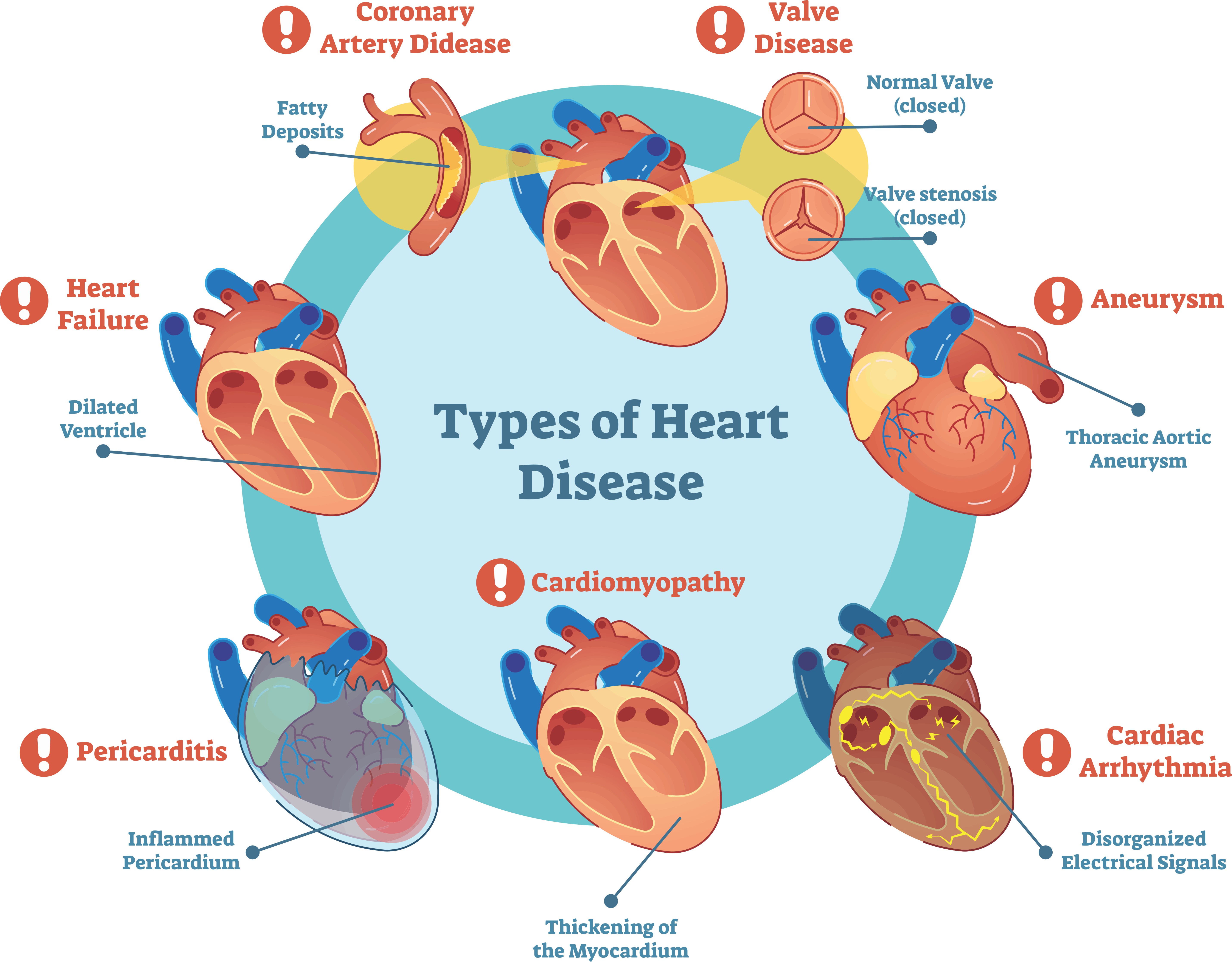
B. Acquired Heart Diseases
Acquired heart diseases develop after birth and are often caused by infection, inflammation, or other medical conditions. Some common types of acquired heart diseases in children include:
- Rheumatic Heart Disease (RHD): Damage to the heart valves caused by rheumatic fever, a complication of streptococcal infections.
- Kawasaki Disease: Inflammation of blood vessels, which can affect the coronary arteries.
- Myocarditis: Inflammation of the heart muscle, often caused by viral infections.
- Cardiomyopathy: Diseases of the heart muscle that can lead to heart failure.
- Arrhythmias: Irregular heart rhythms.
II. Diagnosis of Pediatric Heart Disease
Early and accurate diagnosis is essential for effective management of pediatric heart disease. The diagnostic process typically involves a combination of clinical evaluation, non-invasive tests, and invasive procedures.
A. Clinical Evaluation
- Medical History: A thorough medical history, including family history of heart disease, prenatal history, and any symptoms the child is experiencing.
- Physical Examination: A comprehensive physical examination, including assessment of heart rate, respiratory rate, blood pressure, and listening to the heart for murmurs or other abnormal sounds.
- Symptoms: Common symptoms of pediatric heart disease may include:
- Cyanosis (bluish discoloration of the skin)
- Shortness of breath
- Fatigue
- Poor feeding or weight gain
- Sweating
- Chest pain
- Swelling in the legs, ankles, or abdomen
- Irregular heart rhythms
B. Non-Invasive Tests
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart and can detect arrhythmias, heart enlargement, and other abnormalities.
- Echocardiogram: Uses sound waves to create images of the heart, allowing doctors to visualize the heart’s structure, function, and blood flow. There are several types of echocardiograms, including:
- Transthoracic Echocardiogram (TTE): Performed by placing a transducer on the chest.
- Transesophageal Echocardiogram (TEE): Performed by inserting a probe into the esophagus to obtain clearer images of the heart.
- Fetal Echocardiogram: Performed during pregnancy to detect heart defects in the fetus.
- Chest X-Ray: Provides an image of the heart and lungs and can help identify heart enlargement, fluid in the lungs, or other abnormalities.
- Cardiac Magnetic Resonance Imaging (MRI): Uses magnetic fields and radio waves to create detailed images of the heart and blood vessels.
- Cardiac Computed Tomography (CT) Scan: Uses X-rays to create detailed images of the heart and blood vessels.
- Exercise Stress Test: Assesses the heart’s function during exercise and can help detect arrhythmias or ischemia (reduced blood flow to the heart).
- Holter Monitor: A portable ECG that records the heart’s electrical activity over a period of 24-48 hours or longer, used to detect intermittent arrhythmias.
C. Invasive Procedures
- Cardiac Catheterization: A thin, flexible tube (catheter) is inserted into a blood vessel and guided to the heart. This procedure allows doctors to measure pressures in the heart, take blood samples, and perform interventions such as balloon angioplasty or stent placement.
- Electrophysiology Study (EPS): A catheter is used to map the electrical activity of the heart and identify the source of arrhythmias.
III. Treatment of Pediatric Heart Disease
Treatment for pediatric heart disease depends on the specific condition, its severity, and the child’s overall health. Treatment options may include medication, interventional procedures, and surgery.
A. Medical Management
- Medications:
- Diuretics: Help remove excess fluid from the body.
- ACE Inhibitors: Relax blood vessels and lower blood pressure.
- Beta-Blockers: Slow the heart rate and lower blood pressure.
- Digoxin: Helps the heart pump more efficiently.
- Antiarrhythmic Drugs: Help control irregular heart rhythms.
- Prostaglandins: Used to keep the ductus arteriosus open in infants with certain congenital heart defects.
- Nutritional Support: Ensuring adequate nutrition is crucial for growth and development in children with heart disease. Some infants may require high-calorie formulas or feeding tubes.
- Infection Prevention: Children with heart disease are at increased risk of infections, so preventive measures such as vaccinations and good hygiene are essential.
B. Interventional Procedures
- Balloon Angioplasty: A balloon-tipped catheter is used to widen narrowed blood vessels or heart valves.
- Stent Placement: A small mesh tube (stent) is placed in a blood vessel to keep it open.
- Closure Devices: Devices used to close holes in the heart, such as VSDs, ASDs, and PDAs, through cardiac catheterization.
- Valve Repair or Replacement: Repairing or replacing damaged heart valves using minimally invasive techniques.
C. Surgical Management
- Open-Heart Surgery: Involves making an incision in the chest to access the heart and repair or correct defects. Common surgical procedures include:
- VSD Closure: Patching the hole in the ventricular septum.
- ASD Closure: Patching the hole in the atrial septum.
- Tetralogy of Fallot Repair: Correcting the four defects of TOF.
- Transposition of the Great Arteries (TGA) Repair: Switching the aorta and pulmonary artery to their correct positions.
- Coarctation of the Aorta Repair: Removing the narrowed section of the aorta and reconnecting the ends.
- Valve Repair or Replacement: Repairing or replacing damaged heart valves.
- Heart Transplantation: In severe cases of heart failure, heart transplantation may be necessary.
IV. Long-Term Management and Follow-Up
Children with heart disease require long-term monitoring and follow-up to ensure optimal health and quality of life. This includes:
- Regular Check-Ups: Regular visits with a pediatric cardiologist to monitor heart function, detect any complications, and adjust treatment as needed.
- Medication Management: Ensuring that the child is taking medications as prescribed and monitoring for any side effects.
- Lifestyle Modifications: Encouraging a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking.
- Endocarditis Prophylaxis: Antibiotics may be recommended before certain dental or surgical procedures to prevent endocarditis (infection of the heart valves).
- Psychosocial Support: Providing support to the child and family to cope with the emotional and psychological challenges of living with heart disease.
V. Advances in Pediatric Cardiology
Pediatric cardiology has made significant advances in recent years, leading to improved outcomes for children with heart disease. Some of these advances include:
- Improved Diagnostic Techniques: Advanced imaging techniques such as fetal echocardiography and cardiac MRI allow for earlier and more accurate diagnosis of heart defects.
- Minimally Invasive Procedures: Interventional procedures such as balloon angioplasty and stent placement offer less invasive alternatives to surgery.
- Surgical Techniques: Advances in surgical techniques have improved the success rates of complex heart surgeries.
- Genetic Testing: Genetic testing can help identify the underlying causes of some congenital heart defects.
VI. Conclusion
Pediatric heart disease encompasses a wide range of conditions that require early diagnosis and appropriate treatment. With advances in diagnostic techniques, interventional procedures, and surgical techniques, the outcomes for children with heart disease have significantly improved. Long-term management and follow-up are essential to ensure optimal health and quality of life for these children. Continued research and innovation in pediatric cardiology hold promise for further improving the lives of children with heart disease.








Leave a Reply