“Supportive Care in Chronic Lymphocytic Leukemia (CLL): A Comprehensive Guide
Related Articles Supportive Care in Chronic Lymphocytic Leukemia (CLL): A Comprehensive Guide
- Nutritional Therapy For Chronic Disease Prevention – Part 7: The Role Of Personalized Nutrition In Managing Chronic Conditions
- Understanding Chronic Diseases: Causes And Management – Part 6
- Sleep Disorders And Chronic Disease Relationships – Part 3: Exploring The Complex Interplay And Management Strategies
- Disability Rights And Advocacy For Chronic Disease Patients – Part 10: Intersectionality, Chronic Disease, And Disability Rights
- Chronic Disease Management In Low-Income Communities – Part 7: Leveraging Technology And Innovation For Enhanced Care Delivery
Introduction
With great enthusiasm, let’s explore interesting topics related to Supportive Care in Chronic Lymphocytic Leukemia (CLL): A Comprehensive Guide. Let’s knit interesting information and provide new insights to readers.
Table of Content
Supportive Care in Chronic Lymphocytic Leukemia (CLL): A Comprehensive Guide
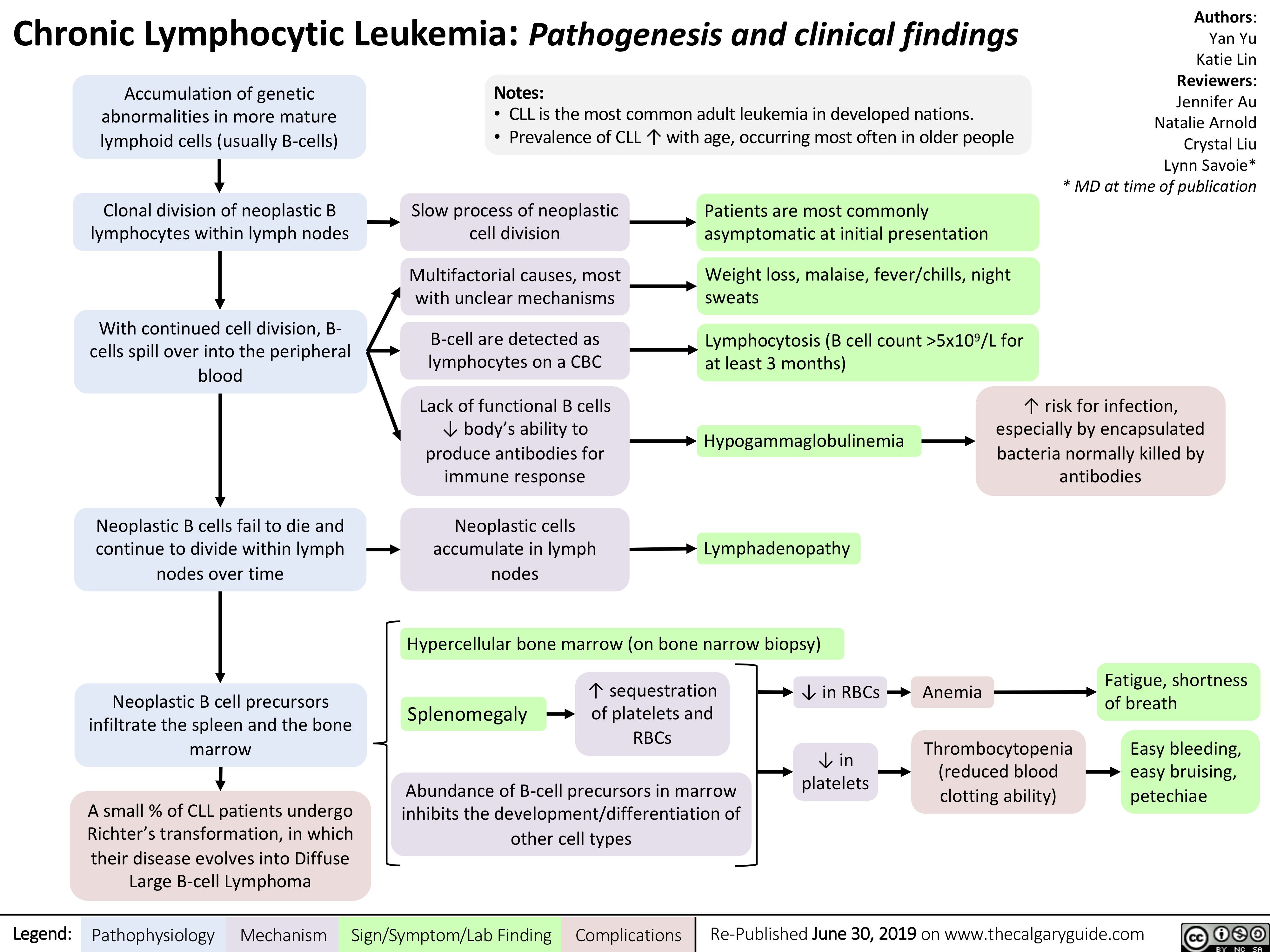
Chronic lymphocytic leukemia (CLL) is a type of cancer that affects the blood and bone marrow. It is characterized by the slow accumulation of abnormal lymphocytes, a type of white blood cell. While significant advances have been made in the treatment of CLL, supportive care remains a crucial aspect of managing the disease and improving the quality of life for patients.
What is Supportive Care?
Supportive care, also known as palliative care, focuses on managing the symptoms and side effects of CLL and its treatment. It aims to improve the patient’s overall well-being and quality of life, regardless of the stage of the disease or the treatment being received. Supportive care is not limited to end-of-life care; it can be provided at any point during the course of the illness.
Why is Supportive Care Important in CLL?
CLL can cause a variety of symptoms and complications, including:
- Fatigue: One of the most common and debilitating symptoms.
- Infections: CLL and its treatments can weaken the immune system, making patients more susceptible to infections.
- Anemia: Low red blood cell count, leading to fatigue and shortness of breath.
- Thrombocytopenia: Low platelet count, increasing the risk of bleeding.
- Enlarged Lymph Nodes: Causing discomfort and pressure on surrounding organs.
- Night Sweats: Disrupting sleep and causing discomfort.
- Weight Loss: Due to decreased appetite and metabolic changes.
- Pain: From enlarged lymph nodes or other complications.
- Emotional Distress: Anxiety, depression, and fear related to the diagnosis and treatment.
Supportive care addresses these symptoms and complications, helping patients maintain their physical, emotional, and social well-being.
Key Components of Supportive Care in CLL
Supportive care in CLL involves a multidisciplinary approach, with various healthcare professionals working together to provide comprehensive care. The key components include:
-
Management of Infections
- Vaccinations: Vaccinations against influenza, pneumococcal pneumonia, and other common infections are recommended to reduce the risk of infection. Live vaccines should be avoided in patients with CLL due to their weakened immune system.
- Prophylactic Antibiotics: In some cases, prophylactic antibiotics or antiviral medications may be prescribed to prevent infections, especially in patients with a history of recurrent infections or those undergoing intensive treatment.
- Prompt Treatment of Infections: Any signs of infection, such as fever, cough, or sore throat, should be promptly evaluated and treated with appropriate antibiotics or antiviral medications.
- Hygiene Practices: Maintaining good hygiene practices, such as frequent handwashing, avoiding close contact with sick individuals, and practicing safe food handling, can help prevent infections.
-
Management of Anemia and Thrombocytopenia
- Blood Transfusions: Red blood cell transfusions may be necessary to treat anemia and improve oxygen delivery to the tissues. Platelet transfusions may be required to manage thrombocytopenia and reduce the risk of bleeding.
- Growth Factors: Erythropoiesis-stimulating agents (ESAs) may be used to stimulate red blood cell production in patients with anemia. Thrombopoietin receptor agonists (TPO-RAs) may be used to increase platelet production in patients with thrombocytopenia.
- Treatment of Underlying Causes: Identifying and treating underlying causes of anemia and thrombocytopenia, such as autoimmune hemolytic anemia or immune thrombocytopenic purpura (ITP), can help improve blood counts.
-
Management of Enlarged Lymph Nodes
- Observation: In some cases, enlarged lymph nodes may not require immediate treatment and can be monitored closely.
- Radiation Therapy: Localized radiation therapy may be used to shrink enlarged lymph nodes that are causing significant discomfort or pressure on surrounding organs.
- Systemic Therapy: Systemic therapy, such as chemotherapy or targeted therapy, may be used to reduce the size of enlarged lymph nodes throughout the body.
-
Management of Fatigue
- Addressing Underlying Causes: Identifying and addressing underlying causes of fatigue, such as anemia, infection, or depression, can help improve energy levels.
- Exercise: Regular exercise, such as walking, swimming, or cycling, can help improve energy levels and reduce fatigue.
- Nutrition: Eating a healthy, balanced diet can provide the body with the nutrients it needs to function properly and reduce fatigue.
- Sleep Hygiene: Practicing good sleep hygiene, such as maintaining a regular sleep schedule and creating a relaxing bedtime routine, can help improve sleep quality and reduce fatigue.
- Energy Conservation Techniques: Learning energy conservation techniques, such as pacing activities and prioritizing tasks, can help patients manage their energy levels and reduce fatigue.
-
Pain Management
- Pain Assessment: A thorough pain assessment is essential to identify the cause, location, and severity of pain.
- Pain Medications: Pain medications, such as analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and opioids, may be used to relieve pain.
- Non-Pharmacological Therapies: Non-pharmacological therapies, such as physical therapy, massage, acupuncture, and relaxation techniques, can also help manage pain.
-
Nutritional Support
- Dietary Counseling: A registered dietitian can provide dietary counseling to help patients maintain a healthy weight, manage side effects of treatment, and improve their overall nutritional status.
- Nutritional Supplements: Nutritional supplements, such as vitamins, minerals, and protein supplements, may be recommended to address nutritional deficiencies.
- Enteral or Parenteral Nutrition: In some cases, enteral (tube feeding) or parenteral (intravenous) nutrition may be necessary to provide adequate nutrition.
-
Psychosocial Support
- Counseling: Counseling can help patients cope with the emotional challenges of CLL, such as anxiety, depression, and fear.
- Support Groups: Support groups provide a safe and supportive environment for patients to share their experiences and connect with others who understand what they are going through.
- Spiritual Support: Spiritual support can provide comfort and meaning for patients and their families.
- Family Support: Family support is essential for helping patients cope with CLL. Family members can provide emotional support, practical assistance, and help with decision-making.
-
Management of Treatment-Related Side Effects
- Chemotherapy Side Effects: Chemotherapy can cause a variety of side effects, such as nausea, vomiting, hair loss, and mouth sores. Supportive care measures can help manage these side effects and improve the patient’s comfort.
- Targeted Therapy Side Effects: Targeted therapies can also cause side effects, such as rash, diarrhea, and fatigue. Supportive care measures can help manage these side effects and improve the patient’s adherence to treatment.
- Immunotherapy Side Effects: Immunotherapy can cause immune-related side effects, such as inflammation of the skin, lungs, or liver. Supportive care measures, such as corticosteroids, may be necessary to manage these side effects.
The Role of the Healthcare Team
A multidisciplinary healthcare team is essential for providing comprehensive supportive care in CLL. The team may include:
- Hematologist/Oncologist: The physician who specializes in the diagnosis and treatment of blood cancers.
- Nurse: Provides direct patient care, administers medications, and educates patients and families about CLL and its treatment.
- Social Worker: Provides emotional support, helps patients access resources, and assists with practical matters such as financial assistance and transportation.
- Registered Dietitian: Provides dietary counseling and helps patients maintain a healthy weight and nutritional status.
- Physical Therapist: Helps patients improve their strength, flexibility, and endurance.
- Occupational Therapist: Helps patients adapt to their environment and perform daily activities.
- Psychologist/Psychiatrist: Provides counseling and support for emotional and mental health issues.
- Palliative Care Specialist: Provides specialized care for patients with serious illnesses, focusing on symptom management and quality of life.
Conclusion
Supportive care is an integral part of managing CLL and improving the quality of life for patients. By addressing the symptoms and complications of the disease and its treatment, supportive care helps patients maintain their physical, emotional, and social well-being. A multidisciplinary healthcare team is essential for providing comprehensive supportive care. Patients with CLL should discuss their supportive care needs with their healthcare team to develop a personalized plan that meets their individual needs.








Leave a Reply