“Leukemia Biomarkers: Diagnostic and Prognostic Significance
Related Articles Leukemia Biomarkers: Diagnostic and Prognostic Significance
- Lifestyle Changes To Manage Chronic Conditions – Part 6
- Ethical Considerations In Chronic Disease Research – Part 4
- Nutritional Therapy For Chronic Disease Prevention – Part 4: Implementing Personalized Nutrition Plans And Overcoming Challenges
- Integrative Medicine In Chronic Disease Care – Part 8: Integrative Approaches To Autoimmune Disorders
- Disability Rights And Advocacy For Chronic Disease Patients – Part 8
Introduction
We will be happy to explore interesting topics related to Leukemia Biomarkers: Diagnostic and Prognostic Significance. Come on knit interesting information and provide new insights to readers.
Table of Content
Leukemia Biomarkers: Diagnostic and Prognostic Significance

Leukemia, a group of hematological malignancies affecting the bone marrow and blood, is characterized by the uncontrolled proliferation of abnormal leukocytes. These malignant cells disrupt normal blood cell production, leading to anemia, thrombocytopenia, and increased susceptibility to infections. Leukemia is broadly classified into acute and chronic forms, each with distinct subtypes based on the lineage of the affected cells (myeloid or lymphoid) and the presence of specific genetic abnormalities.
The diagnosis and management of leukemia rely on a combination of clinical findings, morphological examination of blood and bone marrow smears, immunophenotyping, cytogenetic analysis, and molecular studies. In recent years, the identification and characterization of leukemia biomarkers have revolutionized the field, providing valuable tools for diagnosis, risk stratification, monitoring treatment response, and predicting prognosis.
What are Biomarkers?
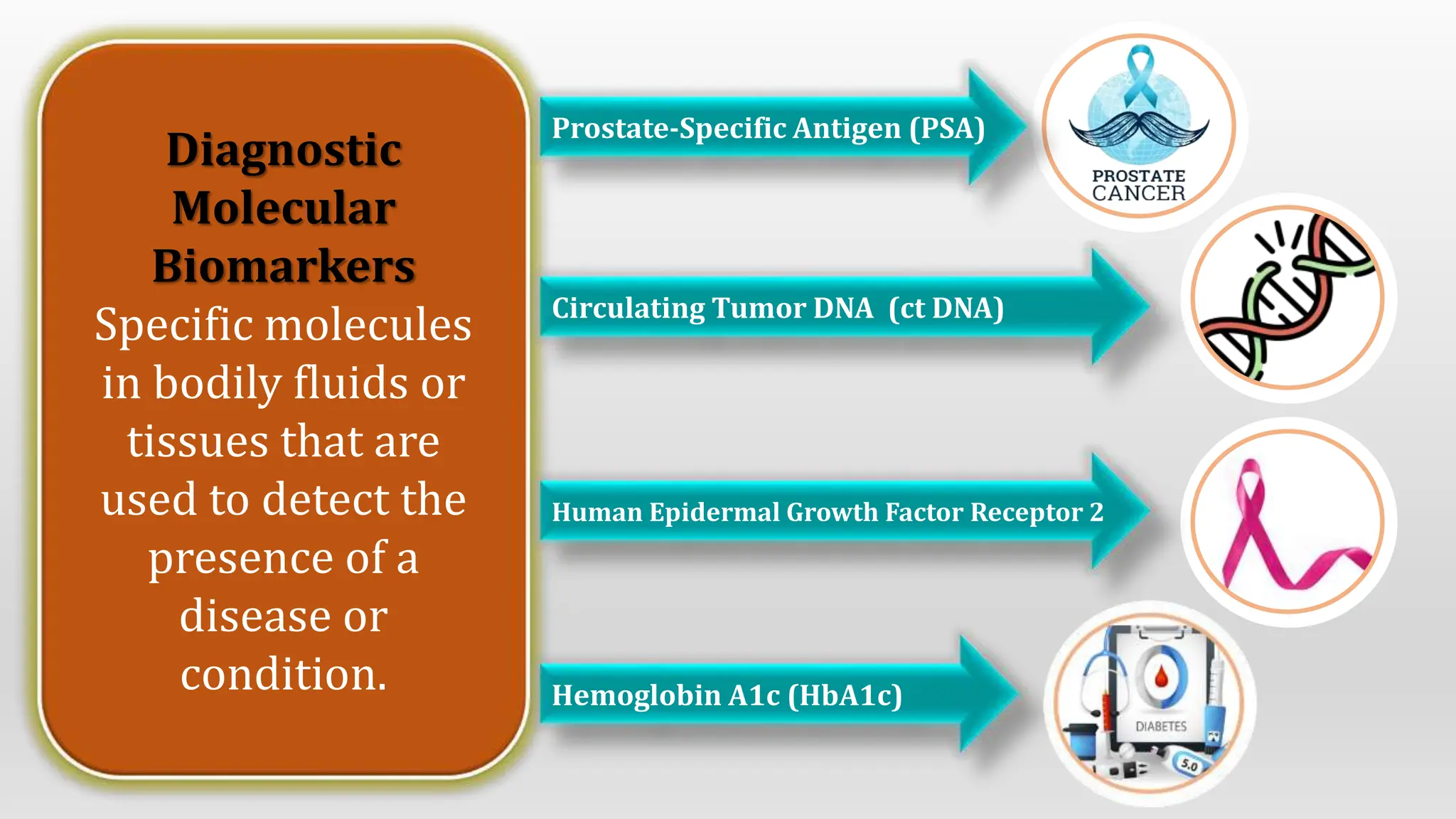
Biomarkers are measurable indicators of a biological state or condition. In the context of leukemia, biomarkers can be molecules, genes, proteins, or cellular characteristics that are associated with the presence, progression, or response to therapy of the disease. These biomarkers can be detected in various biological samples, including blood, bone marrow, cerebrospinal fluid, and tissue biopsies.
Diagnostic Biomarkers in Leukemia
Diagnostic biomarkers play a crucial role in confirming the presence of leukemia, differentiating between subtypes, and identifying specific genetic abnormalities that can guide treatment decisions. Some of the key diagnostic biomarkers in leukemia include:
-
Complete Blood Count (CBC) and Peripheral Blood Smear:
- CBC is a basic hematological test that measures the number of red blood cells, white blood cells, and platelets in the blood. In leukemia, CBC often reveals abnormal white blood cell counts, anemia, and thrombocytopenia.
- Peripheral blood smear involves microscopic examination of blood cells to identify abnormal morphology, such as blasts (immature leukemia cells) and dysplastic features.
-
Bone Marrow Aspirate and Biopsy:
- Bone marrow aspiration and biopsy are essential for confirming the diagnosis of leukemia and assessing the extent of bone marrow involvement.
- Morphological examination of bone marrow cells helps to identify the type of leukemia (acute or chronic, myeloid or lymphoid) and assess the percentage of blasts.
-
Immunophenotyping:
- Immunophenotyping uses flow cytometry to identify specific proteins (antigens) on the surface of leukemia cells.
- This technique is crucial for differentiating between various subtypes of leukemia, such as acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML), and chronic lymphocytic leukemia (CLL).
- Immunophenotyping can also detect aberrant antigen expression, which is associated with specific genetic abnormalities and prognostic implications.
-
Cytogenetic Analysis:
- Cytogenetic analysis involves examining the chromosomes of leukemia cells to identify structural abnormalities, such as translocations, deletions, and inversions.
- Specific chromosomal abnormalities are associated with distinct subtypes of leukemia and have prognostic significance.
- For example, the t(9;22) translocation, which results in the BCR-ABL1 fusion gene, is a hallmark of CML.
-
Molecular Genetic Testing:
- Molecular genetic testing detects specific gene mutations, translocations, and other genetic alterations in leukemia cells.
- These genetic abnormalities can provide valuable information for diagnosis, risk stratification, and targeted therapy.
- Commonly tested genes in leukemia include FLT3, NPM1, CEBPA, KIT, IDH1, IDH2, TP53, and RUNX1.
Prognostic Biomarkers in Leukemia
Prognostic biomarkers are used to predict the likely course of leukemia and to identify patients who are at higher risk of relapse or treatment failure. These biomarkers help clinicians to tailor treatment strategies and to monitor patients more closely. Some of the key prognostic biomarkers in leukemia include:
-
Cytogenetic Abnormalities:
- Certain cytogenetic abnormalities are associated with favorable or unfavorable prognosis in leukemia.
- For example, in AML, t(8;21), inv(16), and t(15;17) are generally associated with a better prognosis, while complex karyotype, monosomy 7, and deletion 5q are associated with a poorer prognosis.
-
Molecular Mutations:
- Specific gene mutations have been shown to have prognostic significance in leukemia.
- For example, in AML, FLT3-ITD mutations are associated with a higher risk of relapse, while NPM1 mutations in the absence of FLT3-ITD are associated with a better prognosis.
- In CLL, IGHV mutation status, TP53 mutations, and del(17p) are associated with a poorer prognosis.
-
Minimal Residual Disease (MRD):
- MRD refers to the presence of a small number of leukemia cells that remain after treatment.
- MRD is a powerful prognostic biomarker in both AML and ALL.
- Patients who achieve MRD negativity after treatment have a significantly lower risk of relapse compared to those who remain MRD positive.
- MRD can be detected using flow cytometry or molecular techniques, such as quantitative polymerase chain reaction (qPCR).
-
Age:
- Age is an important prognostic factor in leukemia.
- Older patients generally have a poorer prognosis than younger patients, due to a higher incidence of comorbidities, poorer tolerance of chemotherapy, and a higher frequency of adverse genetic abnormalities.
-
White Blood Cell Count at Diagnosis:
- A high white blood cell count at diagnosis is associated with a poorer prognosis in some subtypes of leukemia, particularly AML and ALL.
-
Performance Status:
- Performance status, which measures a patient’s overall physical condition and ability to perform daily activities, is an important prognostic factor in leukemia.
- Patients with poor performance status are less likely to tolerate intensive chemotherapy and have a higher risk of complications.
Emerging Biomarkers in Leukemia
In addition to the established diagnostic and prognostic biomarkers, several emerging biomarkers are being investigated for their potential clinical utility in leukemia. These include:
-
Circulating Tumor DNA (ctDNA):
- ctDNA refers to DNA fragments that are released into the bloodstream by cancer cells.
- ctDNA can be analyzed to detect leukemia-specific mutations and to monitor treatment response.
- ctDNA analysis has the potential to provide a non-invasive method for detecting MRD and predicting relapse.
-
MicroRNAs (miRNAs):
- miRNAs are small non-coding RNA molecules that regulate gene expression.
- miRNAs have been shown to be dysregulated in leukemia and may serve as diagnostic and prognostic biomarkers.
-
Metabolomics:
- Metabolomics is the study of small molecules (metabolites) in biological samples.
- Metabolic profiling can identify metabolic signatures that are associated with leukemia and may provide insights into disease pathogenesis and treatment response.
-
Proteomics:
- Proteomics is the study of proteins in biological samples.
- Proteomic analysis can identify protein biomarkers that are associated with leukemia and may provide targets for drug development.
Clinical Significance of Leukemia Biomarkers
Leukemia biomarkers have a significant impact on clinical decision-making, including:
-
Diagnosis and Subtyping:
- Biomarkers are essential for confirming the diagnosis of leukemia and differentiating between subtypes.
-
Risk Stratification:
- Biomarkers are used to identify patients who are at higher risk of relapse or treatment failure.
-
Treatment Selection:
- Biomarkers can guide treatment decisions, such as the choice of chemotherapy regimen, the use of targeted therapy, or the need for stem cell transplantation.
-
Monitoring Treatment Response:
- Biomarkers, such as MRD, are used to monitor treatment response and to detect early signs of relapse.
-
Prognosis Prediction:
- Biomarkers can help to predict the likely course of leukemia and to provide patients with realistic expectations.
Conclusion
Leukemia biomarkers have revolutionized the diagnosis, risk stratification, and management of leukemia. These biomarkers provide valuable information for clinicians to tailor treatment strategies, monitor treatment response, and predict prognosis. As new biomarkers are discovered and validated, the field of leukemia diagnostics and therapeutics will continue to evolve, leading to improved outcomes for patients with this challenging disease.







Leave a Reply