“Personalized Medicine in Leukemia Care: Tailoring Treatment for Optimal Outcomes
Related Articles Personalized Medicine in Leukemia Care: Tailoring Treatment for Optimal Outcomes
- The Role Of Stress In Chronic Disease Progression
- Gender Disparities In Chronic Disease Diagnosis And Treatment – Part 6
- Integrative Medicine In Chronic Disease Care – Part 2
- Patient Education And Health Literacy In Chronic Disease Care – Part 10
- Leukemia Research Innovations: Breakthroughs And Promising Areas
Introduction
With great enthusiasm, let’s explore interesting topics related to Personalized Medicine in Leukemia Care: Tailoring Treatment for Optimal Outcomes. Come on knit interesting information and provide new insights to readers.
Table of Content
Personalized Medicine in Leukemia Care: Tailoring Treatment for Optimal Outcomes
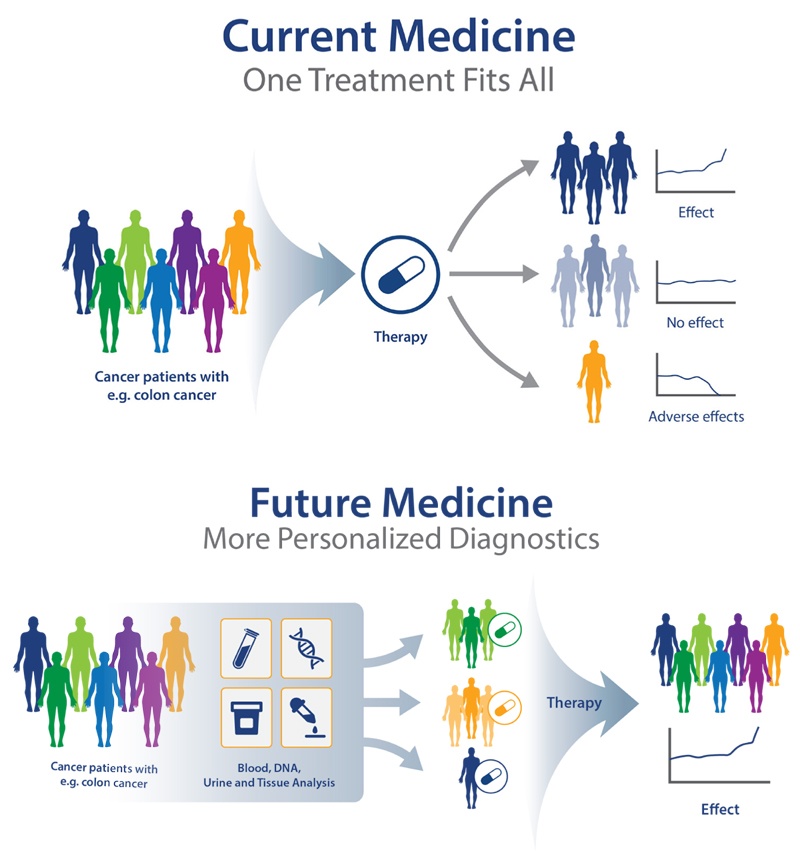
Leukemia, a cancer of the blood and bone marrow, is a complex and heterogeneous disease. In recent years, personalized medicine has emerged as a promising approach to improve the diagnosis, treatment, and management of leukemia. By considering individual patient characteristics, such as genetic mutations, gene expression patterns, and other biomarkers, personalized medicine aims to tailor treatment strategies to maximize efficacy and minimize side effects. This article will explore the principles of personalized medicine in leukemia care, discuss the various diagnostic and therapeutic strategies employed, and highlight the challenges and future directions of this rapidly evolving field.
Understanding Leukemia and Its Heterogeneity
Leukemia is characterized by the uncontrolled proliferation of abnormal blood cells in the bone marrow, which can then infiltrate the bloodstream and other organs. There are several types of leukemia, each with distinct clinical features, genetic abnormalities, and treatment approaches. The major types of leukemia include:
-
Acute Lymphoblastic Leukemia (ALL): This type of leukemia primarily affects lymphocytes, a type of white blood cell. ALL is more common in children, but it can also occur in adults.
-
Acute Myeloid Leukemia (AML): AML affects myeloid cells, which are precursors to red blood cells, platelets, and certain types of white blood cells. AML is more common in adults, but it can occur at any age.
-
Chronic Lymphocytic Leukemia (CLL): CLL is a slow-growing leukemia that affects lymphocytes. It is the most common type of leukemia in adults.
-
Chronic Myeloid Leukemia (CML): CML is characterized by the presence of the Philadelphia chromosome, a genetic abnormality that leads to the production of an abnormal protein called BCR-ABL.
Each type of leukemia is further divided into subtypes based on specific genetic mutations, chromosomal abnormalities, and other molecular markers. This heterogeneity underscores the need for personalized medicine approaches to accurately diagnose and treat leukemia.
Principles of Personalized Medicine in Leukemia Care
Personalized medicine in leukemia care is based on the following principles:
-
Comprehensive Molecular Profiling: Personalized medicine relies on the use of advanced diagnostic techniques, such as next-generation sequencing (NGS), to identify genetic mutations, gene expression patterns, and other molecular markers that are specific to each patient’s leukemia.
-
Risk Stratification: Based on the molecular profile, patients are stratified into different risk groups. This allows clinicians to tailor treatment intensity and select the most appropriate therapeutic strategies for each patient.
-
Targeted Therapies: Personalized medicine aims to identify specific molecular targets that can be targeted with drugs or other therapies. This approach minimizes off-target effects and maximizes the efficacy of treatment.
-
Monitoring Treatment Response: Personalized medicine also involves monitoring the patient’s response to treatment using molecular markers. This allows clinicians to adjust treatment strategies as needed to achieve optimal outcomes.
Diagnostic Strategies in Personalized Leukemia Care
Several diagnostic strategies are used in personalized leukemia care to identify molecular markers and guide treatment decisions. These include:
-
Cytogenetics: Cytogenetic analysis involves examining the chromosomes of leukemia cells to identify abnormalities such as translocations, deletions, and inversions. These abnormalities can provide important prognostic information and help guide treatment decisions.
-
Fluorescence In Situ Hybridization (FISH): FISH is a technique that uses fluorescent probes to detect specific DNA sequences within leukemia cells. FISH can be used to identify chromosomal abnormalities that are not detectable by conventional cytogenetics.
-
Polymerase Chain Reaction (PCR): PCR is a technique that amplifies specific DNA sequences, allowing for the detection of genetic mutations and other molecular markers. PCR is highly sensitive and can be used to detect minimal residual disease (MRD) after treatment.
-
Next-Generation Sequencing (NGS): NGS is a high-throughput sequencing technology that allows for the rapid and cost-effective analysis of multiple genes simultaneously. NGS is used to identify genetic mutations, gene expression patterns, and other molecular markers in leukemia cells.
Therapeutic Strategies in Personalized Leukemia Care
Personalized medicine has led to the development of several targeted therapies for leukemia. These therapies target specific molecular pathways that are essential for the growth and survival of leukemia cells. Some of the targeted therapies used in leukemia care include:
-
Tyrosine Kinase Inhibitors (TKIs): TKIs are drugs that inhibit the activity of tyrosine kinases, enzymes that play a critical role in cell signaling. TKIs are used to treat CML, which is characterized by the presence of the BCR-ABL fusion protein, a tyrosine kinase.
-
Monoclonal Antibodies: Monoclonal antibodies are antibodies that are designed to target specific proteins on the surface of leukemia cells. Monoclonal antibodies can be used to kill leukemia cells directly or to stimulate the immune system to attack leukemia cells.
-
Immunotherapies: Immunotherapies are treatments that boost the immune system’s ability to fight cancer. Immunotherapies used in leukemia care include:
- Checkpoint Inhibitors: Checkpoint inhibitors are drugs that block the activity of checkpoint proteins, which normally prevent the immune system from attacking cancer cells.
- CAR T-cell Therapy: CAR T-cell therapy involves engineering a patient’s own T cells to express a chimeric antigen receptor (CAR) that recognizes a specific protein on the surface of leukemia cells. The CAR T cells are then infused back into the patient, where they can kill leukemia cells.
-
Targeted Chemotherapy: Targeted chemotherapy involves using chemotherapy drugs that are specifically designed to target leukemia cells. These drugs are often combined with other therapies, such as TKIs or monoclonal antibodies.
Challenges and Future Directions
Personalized medicine in leukemia care has made significant progress in recent years, but there are still several challenges that need to be addressed. These include:
-
Cost: Personalized medicine approaches can be expensive, particularly when they involve NGS and other advanced diagnostic techniques. This can limit access to personalized medicine for some patients.
-
Data Interpretation: Interpreting the vast amount of data generated by NGS and other molecular profiling techniques can be challenging. Clinicians need to be trained in bioinformatics and other data analysis skills to effectively use this information.
-
Drug Development: Developing new targeted therapies for leukemia is a complex and time-consuming process. There is a need for more research to identify new molecular targets and develop drugs that can effectively target these targets.
-
Resistance: Leukemia cells can develop resistance to targeted therapies over time. This is a major challenge in personalized medicine. Strategies to overcome resistance include developing new drugs that target different pathways or combining targeted therapies with other treatments.
Despite these challenges, personalized medicine holds great promise for improving the outcomes of patients with leukemia. Future directions in personalized medicine include:
-
Developing More Sensitive Diagnostic Tests: More sensitive diagnostic tests are needed to detect minimal residual disease (MRD) after treatment. This will allow clinicians to identify patients who are at high risk of relapse and to intervene early.
-
Identifying New Molecular Targets: More research is needed to identify new molecular targets that can be targeted with drugs or other therapies. This will lead to the development of new targeted therapies for leukemia.
-
Combining Targeted Therapies: Combining targeted therapies with other treatments, such as chemotherapy or immunotherapy, may be more effective than using targeted therapies alone.
-
Using Artificial Intelligence (AI): AI can be used to analyze large datasets of genomic and clinical data to identify patterns and predict treatment outcomes. This can help clinicians make more informed treatment decisions.
Conclusion
Personalized medicine is transforming the way leukemia is diagnosed, treated, and managed. By considering individual patient characteristics, such as genetic mutations, gene expression patterns, and other biomarkers, personalized medicine aims to tailor treatment strategies to maximize efficacy and minimize side effects. While there are still several challenges to overcome, personalized medicine holds great promise for improving the outcomes of patients with leukemia. As technology advances and our understanding of the molecular basis of leukemia grows, personalized medicine will play an increasingly important role in the fight against this devastating disease.







Leave a Reply