“Integrative Care Models for Complex Chronic Diseases – Part 10: Navigating Ethical Considerations in Integrative Chronic Disease Management
Related Articles Integrative Care Models for Complex Chronic Diseases – Part 10: Navigating Ethical Considerations in Integrative Chronic Disease Management
- Technology’s Role In Chronic Disease Self-Management – Part 5: The Future Of Connected Care And Personalized Health
- Environmental Factors And Chronic Disease Risk – Part 3
- The Role Of Genetics In Chronic Disease Development
- The Impact Of Chronic Illness On Mental Health – Part 10
- Yoga And Mindfulness Practices For Chronic Disease Patients – Part 8
Introduction
With great enthusiasm, let’s explore interesting topics related to Integrative Care Models for Complex Chronic Diseases – Part 10: Navigating Ethical Considerations in Integrative Chronic Disease Management. Come on knit interesting information and provide new insights to readers.
Table of Content
Integrative Care Models for Complex Chronic Diseases – Part 10: Navigating Ethical Considerations in Integrative Chronic Disease Management
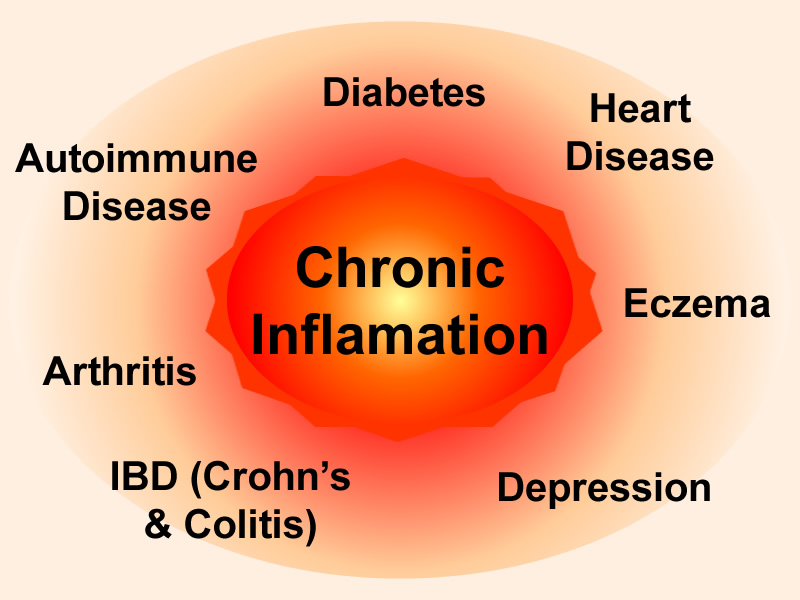
The rise in the prevalence of complex chronic diseases has driven the need for innovative and patient-centered approaches to healthcare. Integrative care models, which combine conventional medicine with complementary and alternative therapies, have emerged as a promising strategy for managing these conditions. However, the integration of diverse modalities and philosophies raises a range of ethical considerations that must be carefully addressed to ensure patient safety, autonomy, and well-being.
1. Informed Consent and Patient Autonomy
Informed consent is a cornerstone of ethical medical practice, and it is particularly crucial in integrative care settings. Patients must receive comprehensive information about the risks, benefits, and evidence base of all treatment options, including both conventional and complementary therapies. This information should be presented in a clear and accessible manner, allowing patients to make informed decisions that align with their values and preferences.
Patient autonomy is another key ethical principle that must be respected in integrative care. Patients have the right to choose the treatments they prefer, even if those treatments differ from the recommendations of their healthcare providers. Integrative practitioners should support patient autonomy by providing unbiased information, facilitating shared decision-making, and respecting patients’ choices.
2. Scope of Practice and Professional Boundaries
Integrative care often involves practitioners from different disciplines working together to provide comprehensive care. It is essential that each practitioner adheres to their scope of practice and respects the professional boundaries of other team members. This helps to ensure that patients receive safe and appropriate care and that there is no overlap or conflict in treatment plans.
Integrative practitioners should also be aware of the legal and regulatory requirements governing their practice. This includes obtaining the necessary licenses and certifications, adhering to ethical codes of conduct, and maintaining adequate liability insurance.
3. Evidence-Based Practice and Transparency
Integrative care should be grounded in evidence-based practice, meaning that treatment decisions should be based on the best available scientific evidence. This includes conducting thorough literature reviews, critically evaluating research findings, and using validated assessment tools.
Integrative practitioners should be transparent about the evidence base for all treatments they offer. This includes discussing the strengths and limitations of the evidence, as well as any potential risks or side effects. Patients should be provided with clear and accurate information so that they can make informed decisions about their care.
4. Conflicts of Interest and Financial Transparency
Conflicts of interest can arise in integrative care settings when practitioners have financial or personal interests that could influence their treatment recommendations. For example, a practitioner may have a financial interest in a particular supplement or therapy, or they may have a personal relationship with a patient.
To mitigate conflicts of interest, integrative practitioners should disclose any potential conflicts to their patients. They should also avoid recommending treatments that are not in the patient’s best interests, even if they would benefit financially.
Financial transparency is also essential in integrative care. Patients should be provided with clear and accurate information about the costs of all treatments, including both conventional and complementary therapies. This allows patients to make informed decisions about their care and to avoid unexpected financial burdens.
5. Cultural Sensitivity and Humility
Integrative care should be culturally sensitive and respectful of patients’ diverse backgrounds and beliefs. Practitioners should be aware of the cultural factors that may influence patients’ health beliefs, values, and preferences. They should also be willing to adapt their treatment approaches to meet the unique needs of each patient.
Cultural humility is an important concept in integrative care. It involves recognizing that one’s own cultural beliefs and practices are not necessarily superior to those of others. Integrative practitioners should approach patients with humility and a willingness to learn from them.
6. Dual Relationships and Exploitation
Dual relationships occur when a healthcare provider has a personal or professional relationship with a patient outside of the therapeutic context. Dual relationships can compromise the provider’s objectivity and create opportunities for exploitation.
Integrative practitioners should avoid dual relationships with patients. This includes avoiding social interactions, business dealings, and romantic relationships. If a dual relationship is unavoidable, the practitioner should take steps to minimize the potential for harm.
Exploitation is a serious ethical concern in healthcare. It occurs when a provider takes advantage of a patient’s vulnerability for their own personal gain. Integrative practitioners should never exploit patients financially, emotionally, or sexually.
7. Confidentiality and Privacy
Confidentiality is a fundamental ethical principle in healthcare. Patients have the right to expect that their personal information will be kept private and confidential. Integrative practitioners should take steps to protect patient confidentiality, including securing medical records, using secure communication channels, and obtaining informed consent before sharing patient information with others.
Privacy is another important ethical consideration in integrative care. Patients have the right to privacy during examinations and treatments. Integrative practitioners should respect patients’ privacy by providing them with a private space, explaining the purpose of all procedures, and obtaining their consent before touching them.
8. Research Ethics and Integrity
Research is essential for advancing the field of integrative care. However, it is important to conduct research ethically and with integrity. This includes obtaining informed consent from research participants, protecting their privacy, and ensuring that the research is conducted in a safe and responsible manner.
Integrative researchers should also be transparent about their research methods and findings. They should avoid manipulating data or selectively reporting results to support their hypotheses.
9. End-of-Life Care and Palliative Care
Integrative care can play an important role in end-of-life care and palliative care. Integrative therapies can help to relieve pain, manage symptoms, and improve the quality of life for patients with terminal illnesses.
When providing end-of-life care, integrative practitioners should respect patients’ wishes and values. They should also provide support to patients’ families and caregivers.
10. Ethical Decision-Making Frameworks
Ethical decision-making can be complex, especially in integrative care settings where there may be conflicting values and priorities. To help navigate ethical dilemmas, integrative practitioners can use ethical decision-making frameworks. These frameworks provide a structured approach to identifying ethical issues, considering different perspectives, and making decisions that are in the best interests of the patient.
Some common ethical decision-making frameworks include:
- The utilitarian approach: This approach focuses on maximizing overall well-being and minimizing harm.
- The rights-based approach: This approach focuses on protecting the rights of individuals.
- The justice-based approach: This approach focuses on ensuring fairness and equity.
- The virtue-based approach: This approach focuses on developing moral character and acting in accordance with ethical principles.
Conclusion
Ethical considerations are paramount in integrative chronic disease management. By adhering to ethical principles such as informed consent, patient autonomy, evidence-based practice, and cultural sensitivity, integrative practitioners can ensure that patients receive safe, effective, and ethical care. As integrative care continues to evolve, it is essential to remain vigilant in addressing ethical challenges and promoting ethical practices. This will help to build trust between patients and practitioners and to ensure that integrative care is a valuable and ethical approach to healthcare.







Leave a Reply