“Mental Health Interventions for Chronic Disease Patients – Part 10
Related Articles Mental Health Interventions for Chronic Disease Patients – Part 10
- Medical Advances In Treating Rare Chronic Conditions – Part 6
- Financial Challenges Of Living With Chronic Illness – Part 7: Navigating The Labyrinth Of Government Assistance Programs
- Public Policy And Chronic Disease Prevention Strategies: A Comprehensive Overview
- Yoga And Mindfulness Practices For Chronic Disease Patients – Part 8
- Integrative Medicine In Chronic Disease Care – Part 8: Integrative Approaches To Autoimmune Disorders
Introduction
On this special occasion, we are happy to review interesting topics related to Mental Health Interventions for Chronic Disease Patients – Part 10. Come on knit interesting information and provide new insights to readers.
Table of Content
Mental Health Interventions for Chronic Disease Patients – Part 10
Introduction
Chronic diseases, such as diabetes, heart disease, cancer, and chronic respiratory diseases, pose significant challenges to global health. While medical advancements have improved disease management and survival rates, the psychological and emotional well-being of individuals living with chronic conditions often remains overlooked. The intricate interplay between physical health and mental health is well-established, with chronic diseases frequently leading to increased rates of depression, anxiety, and other mental health disorders. These psychological comorbidities can negatively impact treatment adherence, disease progression, and overall quality of life.
Recognizing the profound impact of mental health on chronic disease outcomes, healthcare professionals and researchers have increasingly focused on developing and implementing mental health interventions tailored to the unique needs of this population. These interventions aim to address psychological distress, promote coping skills, enhance self-management abilities, and improve overall well-being. In this comprehensive article, we delve into the various mental health interventions available for chronic disease patients, exploring their effectiveness, benefits, and practical applications.
The Importance of Mental Health in Chronic Disease Management
The prevalence of mental health disorders is significantly higher among individuals with chronic diseases compared to the general population. Depression, for instance, is estimated to affect approximately 20-30% of individuals with chronic conditions, while anxiety disorders are also highly prevalent. These psychological comorbidities can have a detrimental impact on various aspects of chronic disease management, including:
-
Treatment Adherence: Mental health disorders can impair an individual’s ability to adhere to prescribed treatment regimens, such as medication adherence, dietary modifications, and lifestyle changes. Depression, for example, can lead to feelings of hopelessness and a lack of motivation, making it challenging to follow through with recommended treatments.
-
Disease Progression: Psychological distress can exacerbate chronic disease symptoms and accelerate disease progression. Stress, anxiety, and depression can trigger physiological changes, such as increased inflammation and impaired immune function, which can negatively impact the course of chronic diseases.
-
Quality of Life: Mental health disorders can significantly diminish an individual’s overall quality of life. Chronic disease patients with depression or anxiety may experience reduced energy levels, impaired social functioning, and difficulty engaging in activities they once enjoyed.
-
Healthcare Costs: The presence of mental health comorbidities can lead to increased healthcare costs. Individuals with chronic diseases and mental health disorders often require more frequent medical visits, hospitalizations, and specialized treatments.
Types of Mental Health Interventions for Chronic Disease Patients
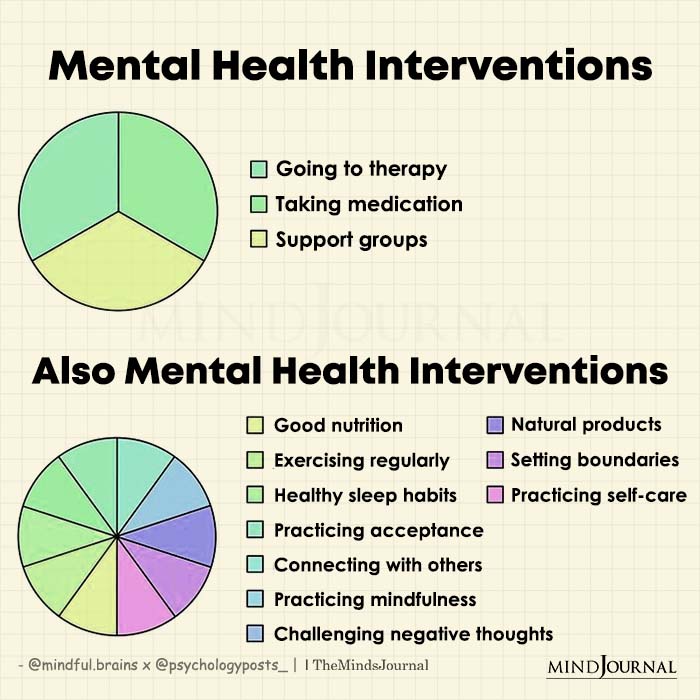
A variety of mental health interventions have been developed and implemented to address the psychological needs of chronic disease patients. These interventions can be broadly categorized into the following types:
-
Psychotherapy: Psychotherapy, also known as talk therapy, involves working with a trained mental health professional to address psychological distress, develop coping skills, and improve overall well-being. Several types of psychotherapy have been shown to be effective for chronic disease patients, including:
-
Cognitive Behavioral Therapy (CBT): CBT is a widely used psychotherapy approach that focuses on identifying and modifying negative thought patterns and behaviors that contribute to psychological distress. CBT can help chronic disease patients manage symptoms of depression, anxiety, and pain, as well as improve coping skills and self-management abilities.
-
Acceptance and Commitment Therapy (ACT): ACT is a type of psychotherapy that emphasizes acceptance of difficult thoughts and feelings, as well as commitment to values-based actions. ACT can help chronic disease patients reduce psychological distress, improve coping skills, and enhance their ability to live a meaningful life despite their chronic condition.
-
Interpersonal Therapy (IPT): IPT is a type of psychotherapy that focuses on improving interpersonal relationships and social support. IPT can help chronic disease patients address relationship difficulties, improve communication skills, and build stronger social connections.
-
-
Mindfulness-Based Interventions: Mindfulness-based interventions involve cultivating awareness of the present moment without judgment. These interventions can help chronic disease patients reduce stress, improve emotional regulation, and enhance their overall well-being. Common mindfulness-based interventions include:
-
Mindfulness-Based Stress Reduction (MBSR): MBSR is an eight-week program that teaches participants mindfulness meditation techniques to reduce stress and improve coping skills. MBSR has been shown to be effective for chronic disease patients in reducing symptoms of anxiety, depression, and pain.
-
Mindfulness-Based Cognitive Therapy (MBCT): MBCT combines mindfulness meditation techniques with cognitive therapy principles to prevent relapse of depression. MBCT can help chronic disease patients identify and manage negative thought patterns and emotions that contribute to depression.
-
-
Support Groups: Support groups provide a safe and supportive environment for chronic disease patients to connect with others who share similar experiences. Support groups can offer emotional support, practical advice, and a sense of community.
-
Psychoeducation: Psychoeducation involves providing patients and their families with information about their chronic disease, its management, and the importance of mental health. Psychoeducation can help patients better understand their condition, reduce anxiety, and improve self-management skills.
-
Medication: In some cases, medication may be necessary to treat mental health disorders in chronic disease patients. Antidepressants and anti-anxiety medications can be effective in reducing symptoms of depression and anxiety. However, it is important to carefully consider the potential side effects and interactions of these medications with other medications the patient may be taking.
Benefits of Mental Health Interventions for Chronic Disease Patients
Mental health interventions offer a wide range of benefits for chronic disease patients, including:
- Reduced symptoms of depression and anxiety
- Improved coping skills
- Enhanced self-management abilities
- Increased treatment adherence
- Improved quality of life
- Reduced healthcare costs
Practical Applications of Mental Health Interventions
Mental health interventions can be integrated into various healthcare settings, including:
- Primary care clinics
- Specialty clinics
- Hospitals
- Community mental health centers
Healthcare professionals can play a vital role in identifying patients who may benefit from mental health interventions and referring them to appropriate services. It is essential to provide patients with information about the available options and support their decision to seek mental health care.
Conclusion
Mental health interventions are an essential component of comprehensive chronic disease management. By addressing the psychological and emotional needs of individuals living with chronic conditions, these interventions can improve treatment adherence, disease progression, quality of life, and overall well-being. Healthcare professionals should prioritize the integration of mental health services into chronic disease care to ensure that patients receive holistic and patient-centered care.
Future Directions
While significant progress has been made in the development and implementation of mental health interventions for chronic disease patients, further research is needed to:
- Develop more targeted and personalized interventions
- Improve access to mental health services
- Evaluate the long-term effectiveness of interventions
- Address the unique needs of diverse populations
By continuing to invest in research and innovation, we can further enhance the mental health and well-being of individuals living with chronic diseases.








Leave a Reply